Incidence
Knee > Hip
- superficial position
- limited cover of well vascularised muscle
- watershed area of skin blood supply anterior to the skin incision
- much increased in fully constrained prosthesis
Ideal < 1%
Risk Factors
Increased with
- revision
- prior infection
- RA / Psoriatic arthropathy
- DM
- Obesity
Aetiology
70% gram positive cocci
- 2/3 Staph epidermidis
- 1/3 Staph aureus
15% Gram negative
Symptoms
Pain
Wound problems
Stiffness
Diagnosis
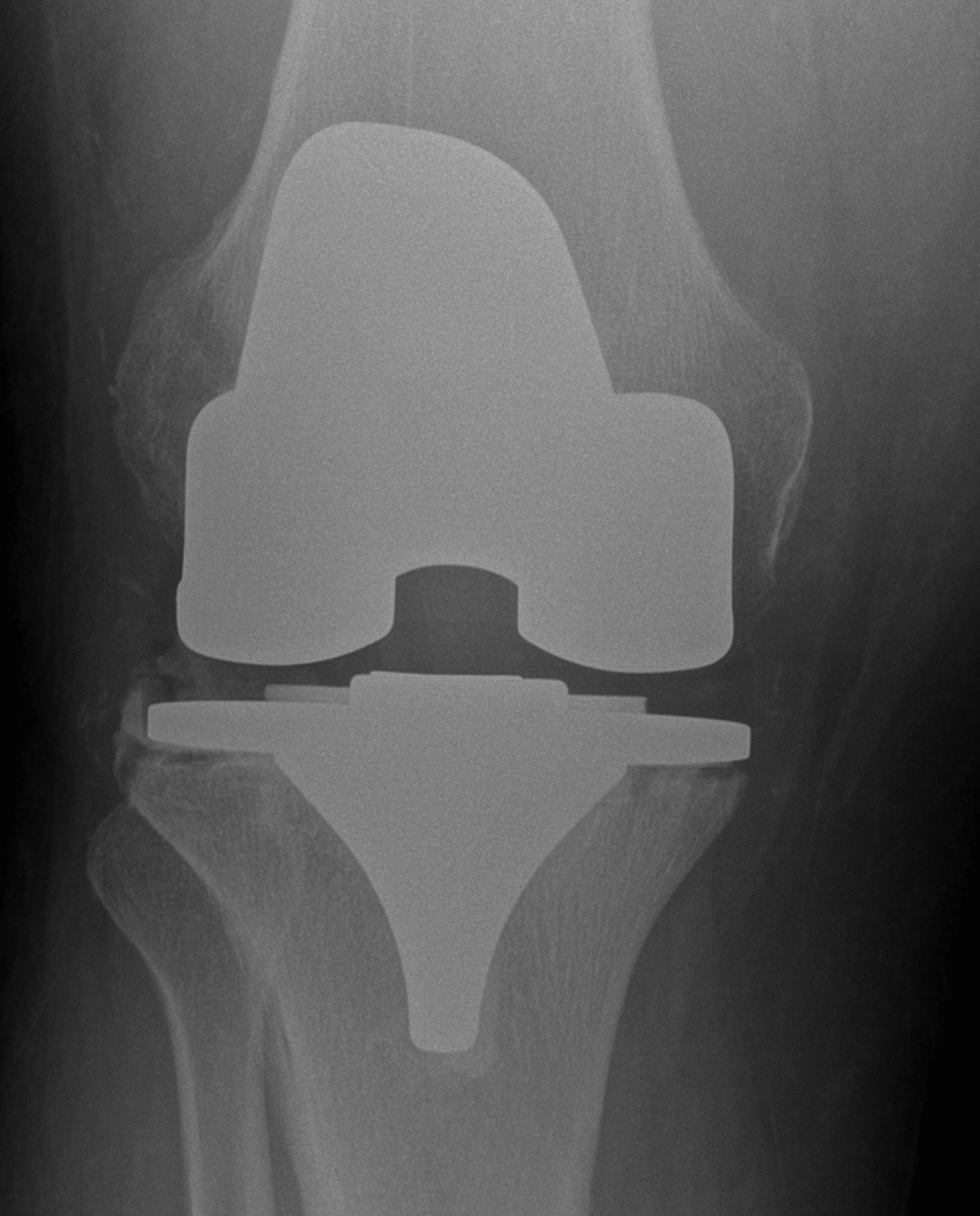
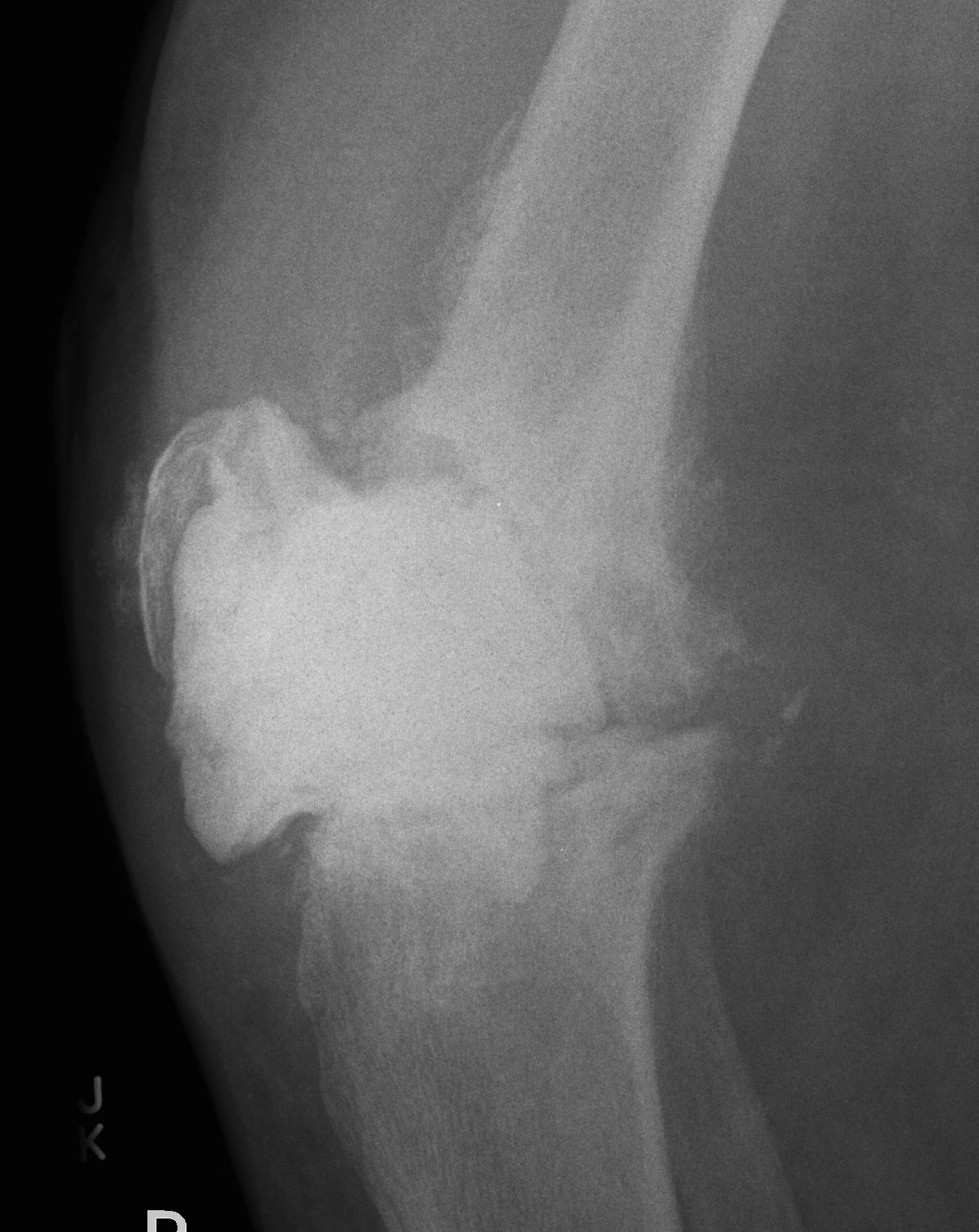
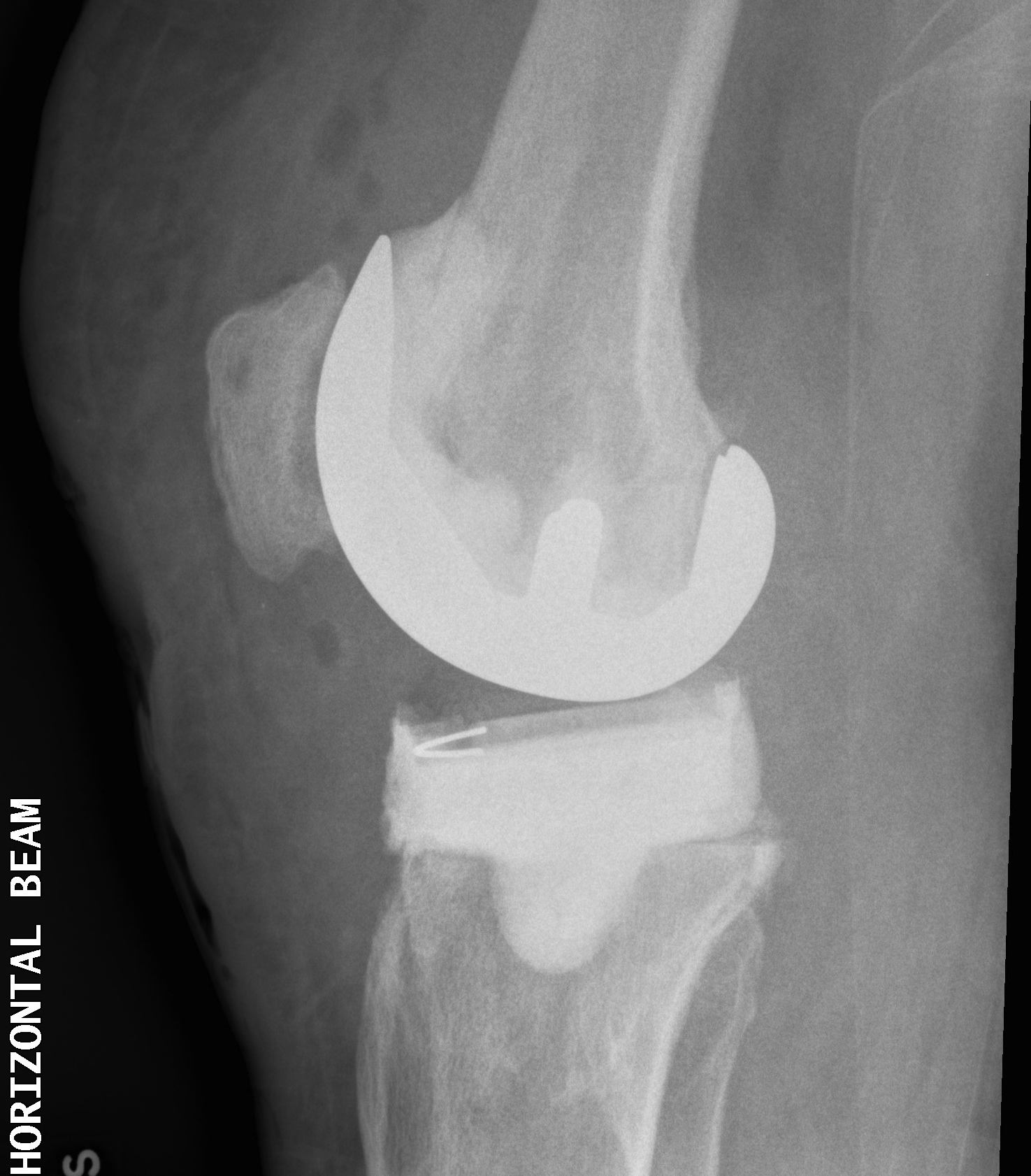
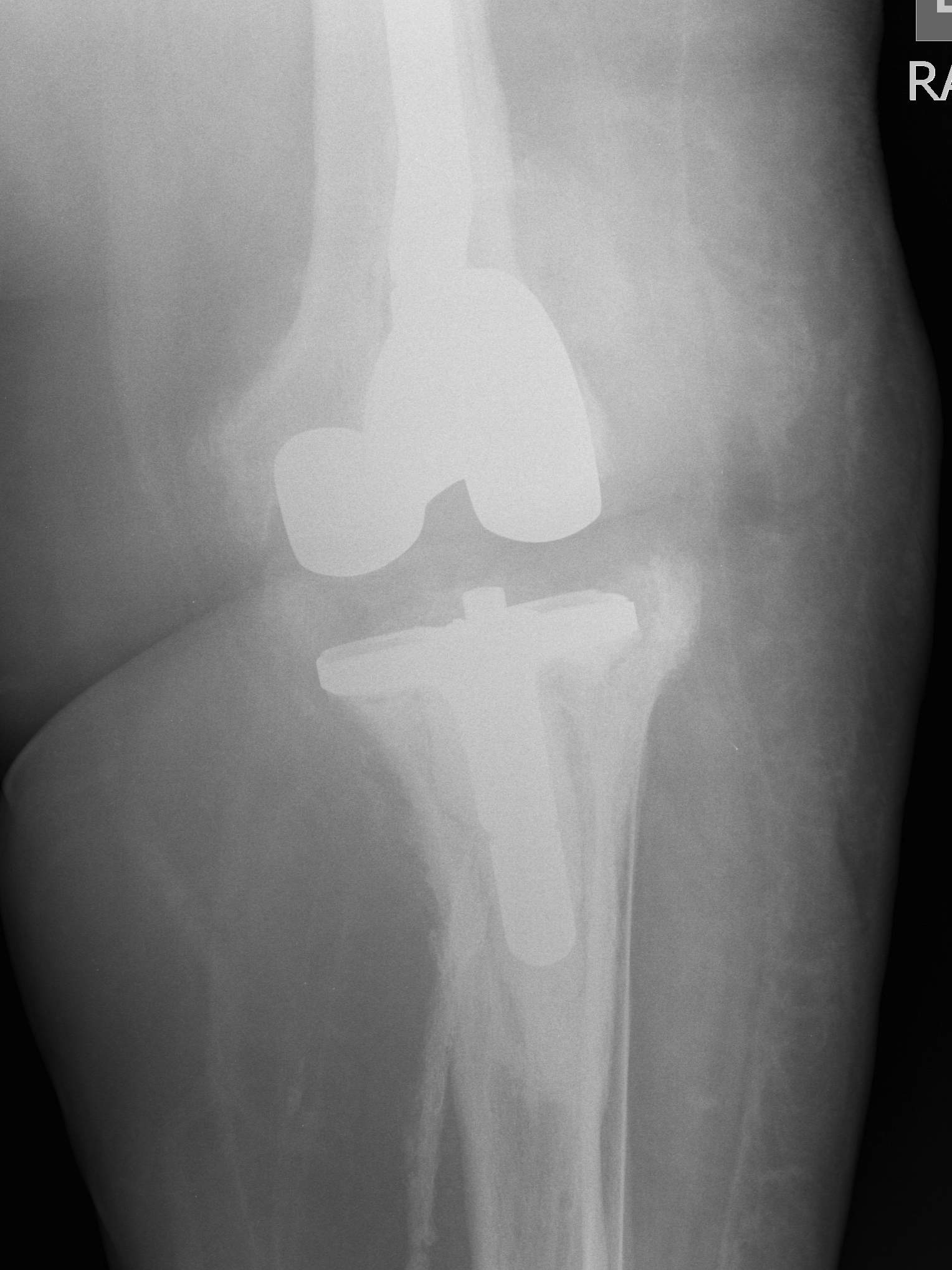
Xray
- progressive early lysis
ESR > 10 / CRP > 30
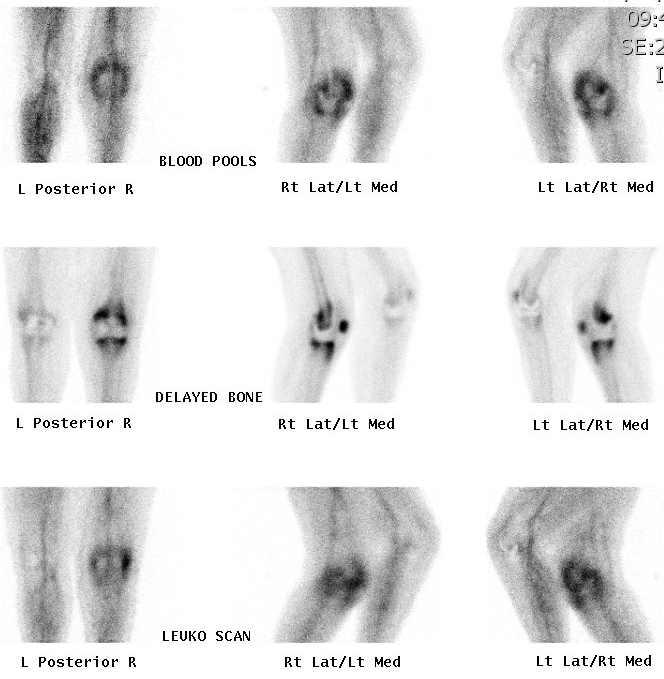
Bone scan
- typically hot blood pool / early and delayed bone phase
- hot on leukocyte scan
Aspiration
- off Antibiotics
Classification
Gustilo 1993
1. Early Post-operative
- < 1/12
- febrile patient
- red swollen discharging wound
2. Late Post-operative
- indolent (low virulent)
- > 1/12
- well patient with healed wound
- worsening of pain / stiffness
- never pain-free interval
3. Acute Haematogenous
- antecedent bacteraemia
- can occur several years after surgery
- well patient with previously well functioning knee
- sudden deterioration / swelling / pain
- often have UTI etc
4. Positive Intra-operative Culture
- presumptive diagnosis aspetic loosening
- intra-operative M/C/S comes back positive (2 out of 5)
Management Options
Stage infection
Host
A Fit
B Medically compromised
C Unfit for anaesthetic
Microbe
- type
- sensitivities
Implant
- stable
- loose
Options
1. Washout / debridement
2. Two stage revision
3. One stage revision
4. Antibiotic suppression
5. Arthrodesis
6. Amputation
1. Debridement
Indications
- early post operative infection < 3/52
- acute haematogenous < 3/52
- sensitive organism
- stable prosthesis
- healthy host
Technique
Incision, drainage
- debridement / synovectomy
- copious irrigation
- poly exchange / also aids debridement
- 1° skin closure
- multiple swabs / tissue samples
Post operative
Administration of antibiotics depending on sensitivity
- duration of 6/52
Results
Gram Positive
Aboltins et al Clin Microbiol Infect 2007
- 20 patients with washout + rifampicin / fusidic acid
- risk of treatment failure 11%
- successful in 10 / 11 MRSA
Gram Negative
Martinez et al Antimicrob Agents Chemoth 2009
- gram negative acute infections in THR and TKR
- retention rates of 70%
- patients did better with a fluoroquinolone
MRSA
Bradbury et al J Arthroplasty 2009
- acute infection with MRSA
- failure rate of 84%
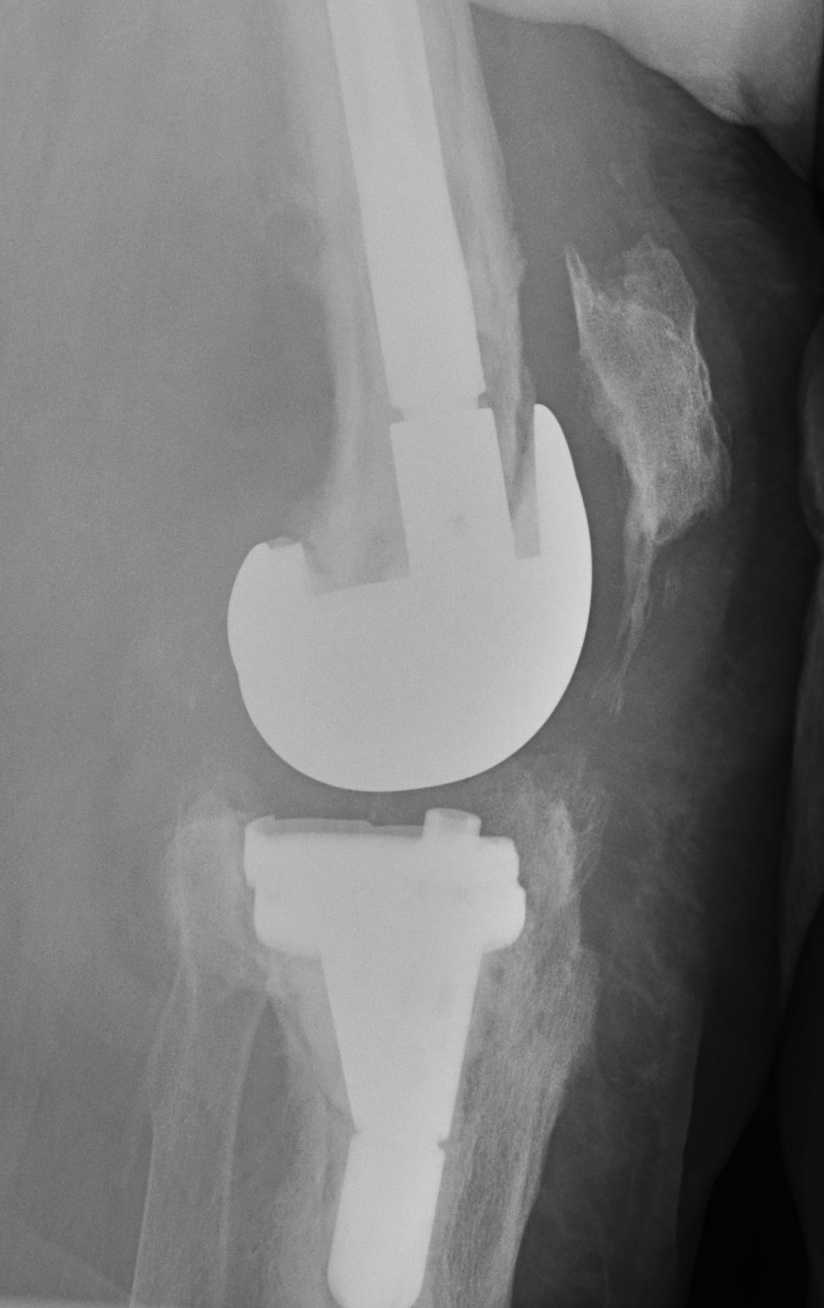
2. Two Stage Revision
Indication
- chronic infection
- Loose prosthesis
- failed early washout / debridement
1st Stage
Remove implant
- multiple swabs and tissue specimens
- prosthesis + cement removed completely
- preserve bone as much as able
- combination micro-sagittal saw, flexible osteotomes & burr
- complete synovectomy and debridement is crucial to success of operation
- washout +++
Insert Intermediate implants
A. Block of antibiotic impregnated cement
Good at eradicating infection as high antibiotic load
- painful / poor ROM
- need to be kept in splint
- worsens bone loss



B. Autoclave old femur / poly tibia or PMMA tibia
Technique
- reimplant femoral component
- gentamicin PMMA + added vancomycin to loosely cement in femur
- all poly tibia or create PMMA tibial component
- patient able to fully weight bear and ROM

C. Femur and tibia made of antibitoic PMMA
Problem
- poor articulation / ROM


D. Femoral implant from antibiotic cement mould / all poly tibia
Technique
- palacos cement (tobramycin) + 3G vancomycin per bag
- make femoral component from various size moulds
- cement in appropriate size all poly tibia with cement +++
- create a balanced knee
- patients are able to fully weight bear and ROM
- no rush to second stage
Interim
Appropriate IV antibiotics for 6/52
- assessment of resolution of infection
- CRP & ESR should remain normal after cessation Abx
- re-aspiration off antibiotics one month to confirm eradication of infection
2nd Stage
Intra-operative
Gram stain & FFD intraoperatively
- abort procedure if positive (>5 WBC per HPF)
- send off swabs +++
Careful removal of prosthesis
Insertion of stemmed revision prosthesis with augments
- constraint as required
- antibiotic cement

Post operative
Need to watch carefully for signs residual infection
Results
Hart et al JBJB Br 2006
- 2 stage reimplantation using articulating cement prosthesis
- 42 / 48 successful (88%)
Anderson et al J Arthroplasty 2009
- autoclaved femur and inserted new poly in 25 patients
- only 1 failure of treatment (4%)
- excellent ROM with spacer 5 - 112o
Mittal et al JBJS Am 2007
- MRSA infection treated with two stage in 37 patients
- 24% reinfection rate
- 10% with MRSA, 14% with different organism
3. One Stage Revision
Advantage
- less debilitating to patient
- less expensive management
Disadvantage
- increased risk of failure
Indication
- healthy host
- known sensitive organism
Technique
- remove implant / cement
- debride as above
- change all operating equipment / rescrub
- new implants with antibiotic laden cement
- post operative Antibiotics
Results
Sofer et al Orthopade 2005
- successful in 14 / 15 knees
- careful patient selection / experienced surgeon
4. Antibiotic Suppression
Indication
1. Prosthesis removal not feasible
- patient medically unwell
2. Organism
- susceptibility to oral antibiotic
- minimal toxicity from antibiotic
3. Prosthesis not loose
Results
Long term success very unlikely