SONK vs Atraumatic AVN
>55 Often mid 30's
MFC Multiple areas
99% unilateral 80% bilateral
Knee only 60-90% other joint
Juxta-articular Epiphysis / diaphysis / metaphysis
Primary Spontaneous Osteonecrosis Knee (SONK)
Clinical
Usually healthy woman age 60+ years
- sudden onset of severe knee pain with normal Xray
Site
Almost always MFC (SONK is a MONK)
- there are case reports of LFC SONK
99% unilateral
Exquisite local tenderness
- may be effusion
SONK of tibial plateau less common
Aetiology
Yamamoto et al JBJS Am 200
- histological study
- evidence of microtrauma / insufficiency fracture
- initial event
- postulated that osteonecrosis is then secondary event around lesion
Primary vascular osteonecrosis may be much more rare
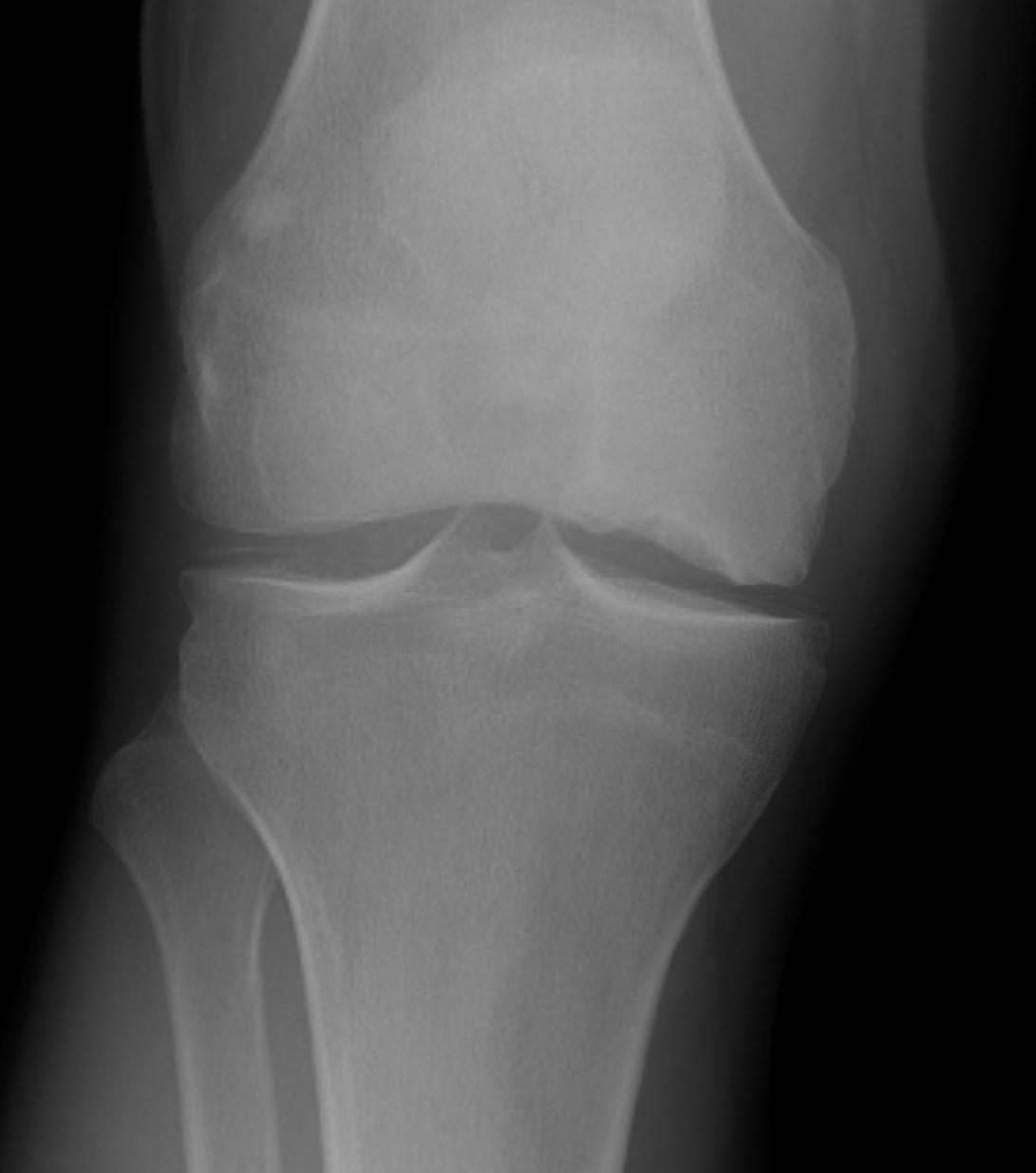
X-ray
Initially normal
Later develop
- subchondral lucent line / crescent Sign
- flattening of condyle
- patchy sclerosis
- can have rapid collapse into varus with development degenerative changes
Bone Scan
Normal x-ray & painful knee in 60 year old think AVN
- consider bone scan
- probably superceded by MRI
Findings
- focal increase in uptake on one side of joint
- if tibia and femur more likely OA
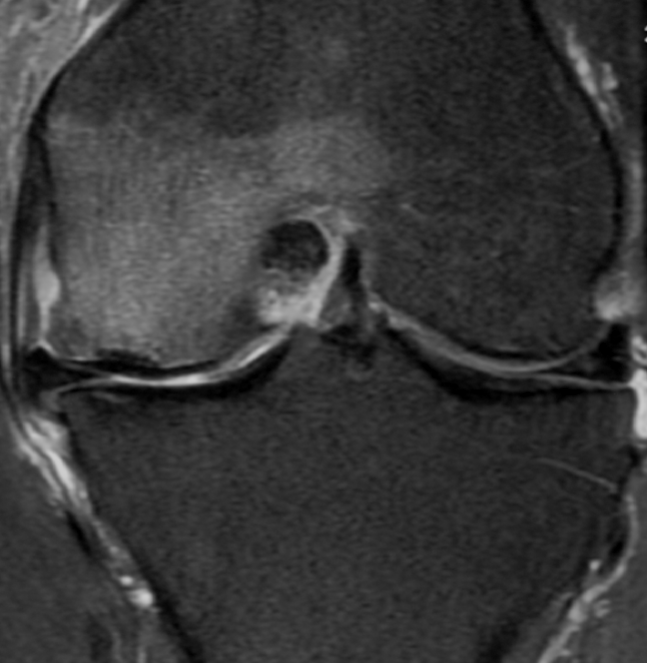
MRI
May be normal in early stages
TI
- low signal areas in subchondral region
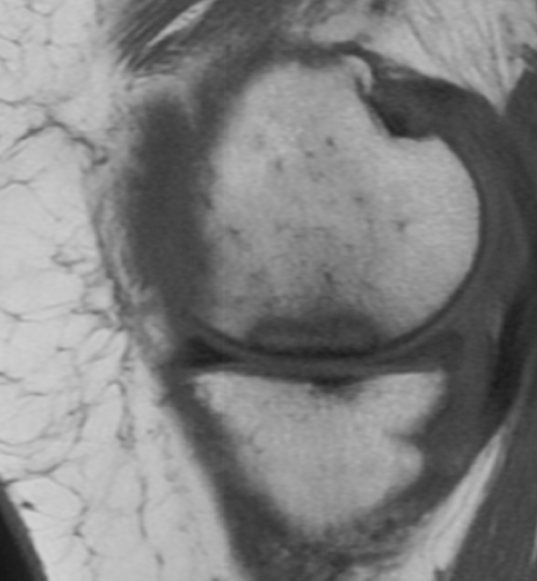
T2
- low signal
- surrounding high intensity signal secondary to oedema
Staging Insall
Stage 1
- normal x-ray with positive bone scan / MRI
Stage 2
- subtle flattening of weight bearing portion of condyle
Stage 3
- typical lesion
- radiolucent area with sclerotic halo
Stage 4
- halo thickened with subchondral collapse
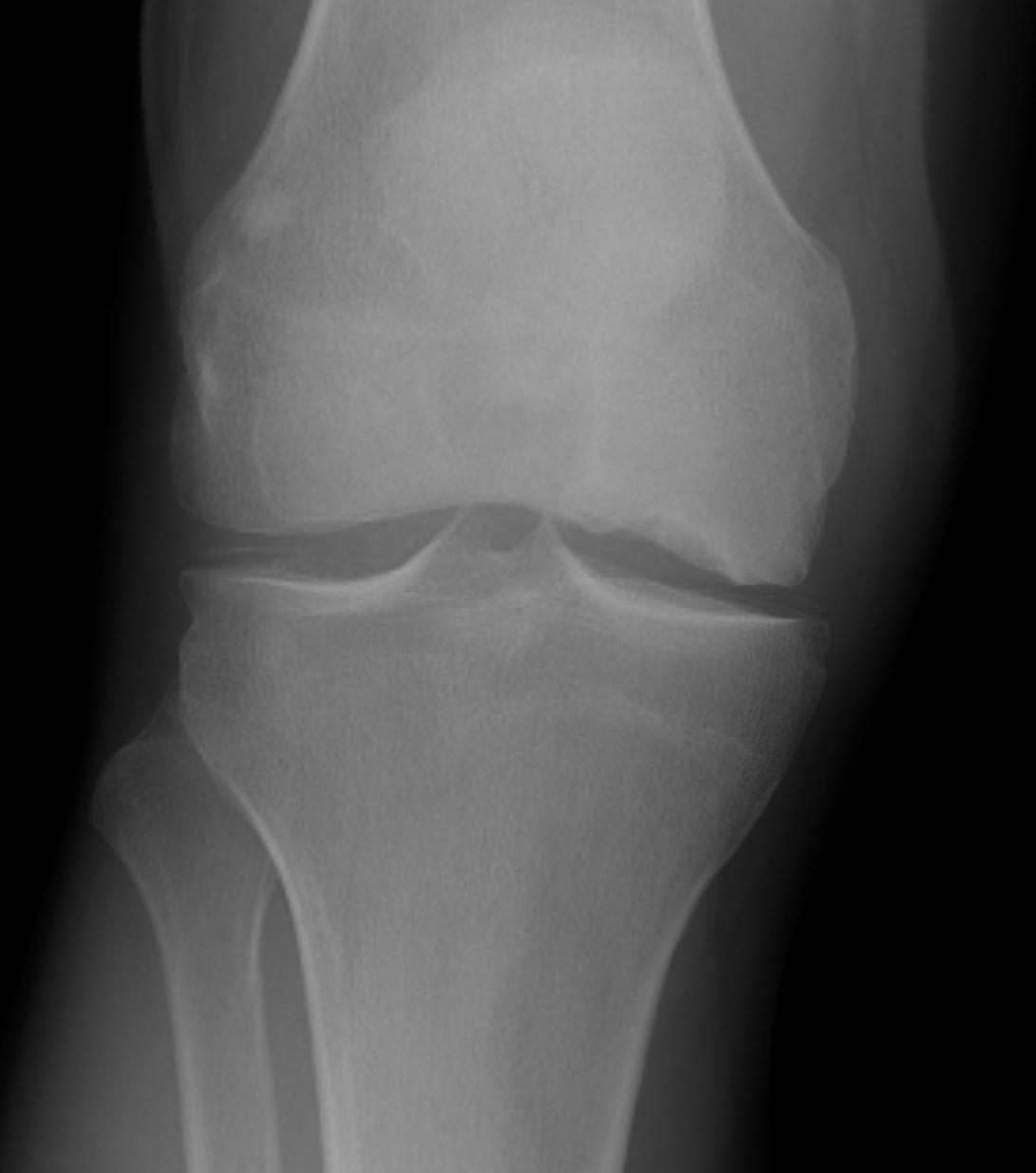
Stage 5
- degenerative change
- varus or valgus angulation

Arthroscopic findings
Localised area of flattened cartilage
- discoloured
- eventually demarcates
- develop flap of cartilage over necrotic bone
The articular sequestrum becomes partially separated as hinged flap
- may separate completely
- cartilage defect becomes filled with necrotic debris and fibrocartilage
- develop OA
Management
Non Operative Management
NHx
Many will resolve spontaneously
- especially small lesions
- best prognosis if chondral surface intact
Yates et al Knee 2007
- followed up 20 patients diagnosed on MRI
- average resolution of symptoms and lesion over 6 months
Program
Decrease impact exercises
Consider unloading brace
Analgesia / NSAID's
Consider bisphosphonates
Follow for 6 - 12 months with repeated MRI looking for resolution / progression
Operative Management
Intact chondral surface / Stage 1 lesion
Decompression / Percutaneous Drilling
Indication
- failure non operative treatment > 6/12
Forst et al Arch Orthop Trauma Surg 1998
- 16 patients with average age 60
- percutaneous drilling with 3 mm drill
- instant resolution of pain
- cannot prevent progression of disease if chondral flattening present
Chondral Defect
Microfracture
Akgun et al Arthroscopy 2005
- debridement of chondral defect and microfracture
- 26 patients average age 48
- 71% could participate in strenous exercise with minimal exertion
- in the remainder the ON progressed on MRI
HTO
Technique
- unload MFC
- younger high demand patient
- combine with microfracture / osteochondral grafting
Osteochondral grafting
Tanaka et al Knee 2009
- 6 patients average age 50
- stage III and IV
- good results in knee scores at 2 years
UKA
Good option as disease is unicompartmental
Langdown et al Acta Orthop 2005
- 29 knees treated with Oxford UKA
- good outcomes and no implant failures at average 5 years
TKR
Secondary osteonecrosis


Causes
- Steroid Therapy (90%)
- Alcohol
- SLE
- Sickle Cell Disease
- Diver's / Caisson's
- marrow proliferative disorder
- chemotherapy
Clinical
Gradual onset of pain
- lateral condyle in 60%
- younger patients, mid 30's
Site
Bilateral in 50%
- 70% have other joints involved
MRI
More extensive involvement through knee
Operative Options
Indications
- failure non operative treatment
- continued pain
Percutaneous Drilling / Decompression
Marulanda et al JBJS Br 2006
- percutaneous drilling in 61 knees with secondary ON
- successfull in all 24 knees with small lesions
- successful in 32/37 (86%) knees with large lesions
