Approach
1. Incision and skin flaps
- previous incision may be L shaped
- may be good to use a vertical midline incision initially in HTO
- can usually incorporate incision
2. Removal of hardware
- may wish to consider staged procedure
- staples not usually a problem (can ignore)
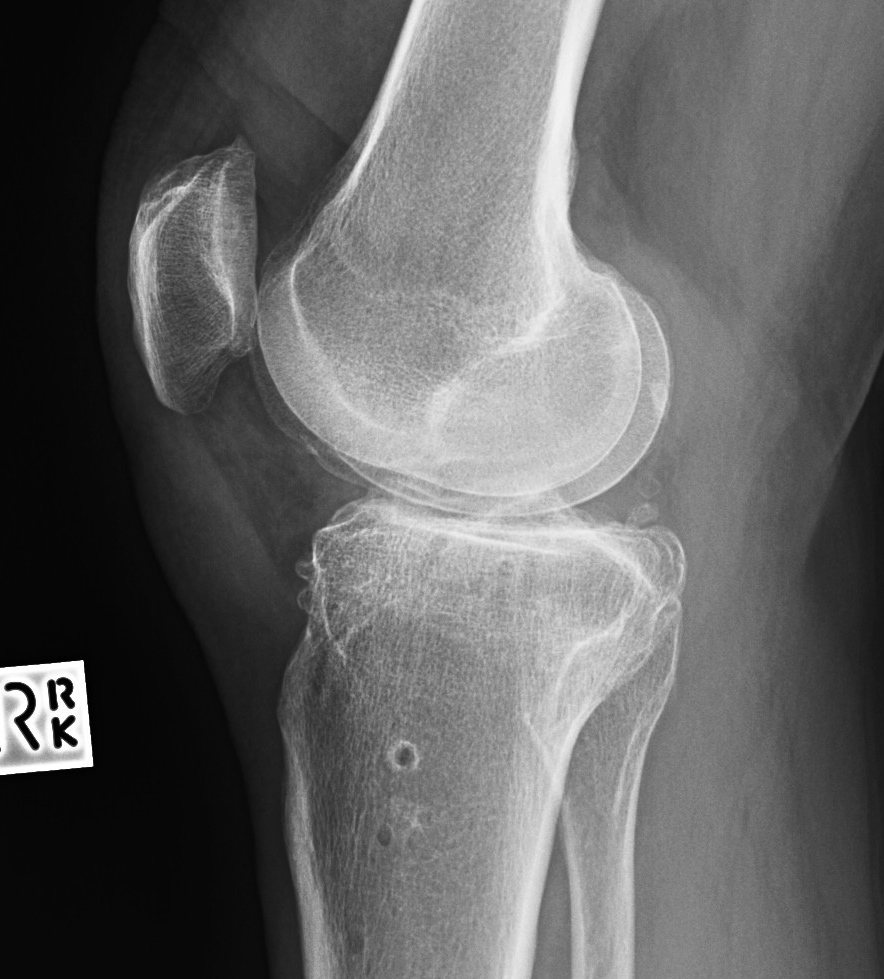
3. Patella Baja
Problem
- patella eversion and exposure difficulties
- PT at risk for avulsion
- may need to consider quadriceps snip / osteotomy
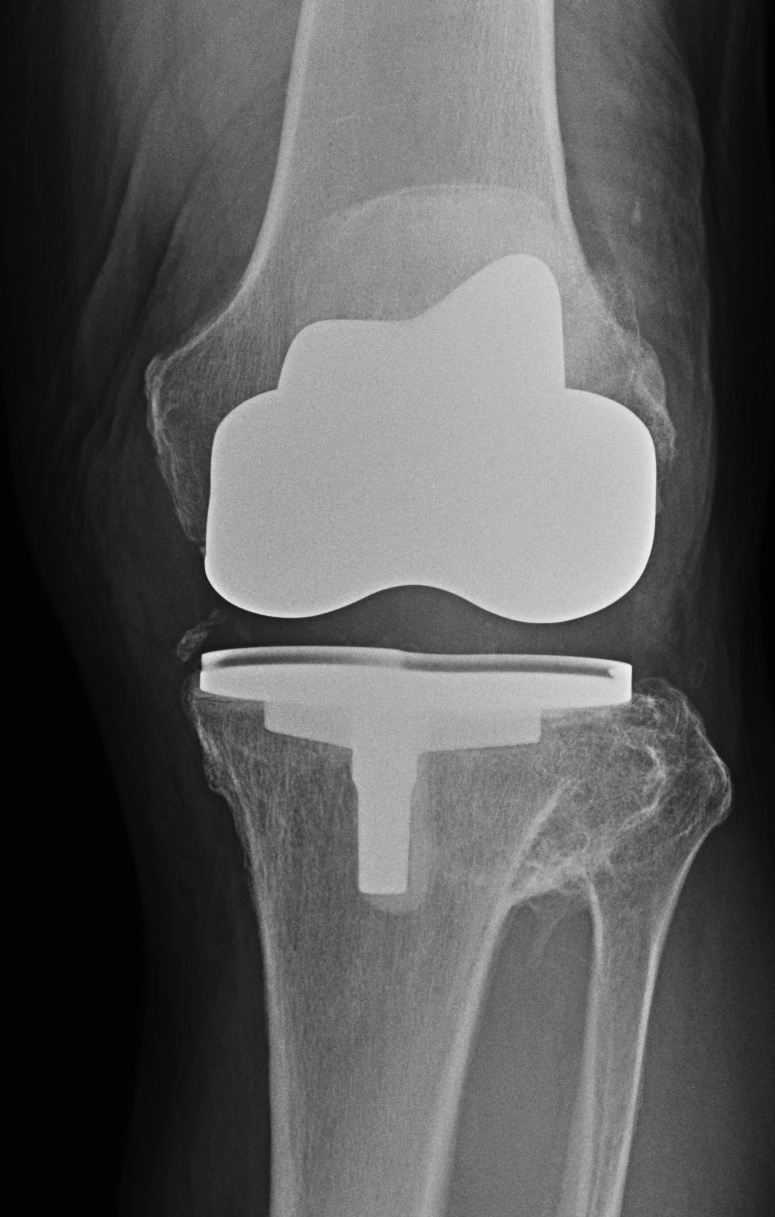
Bone Cuts
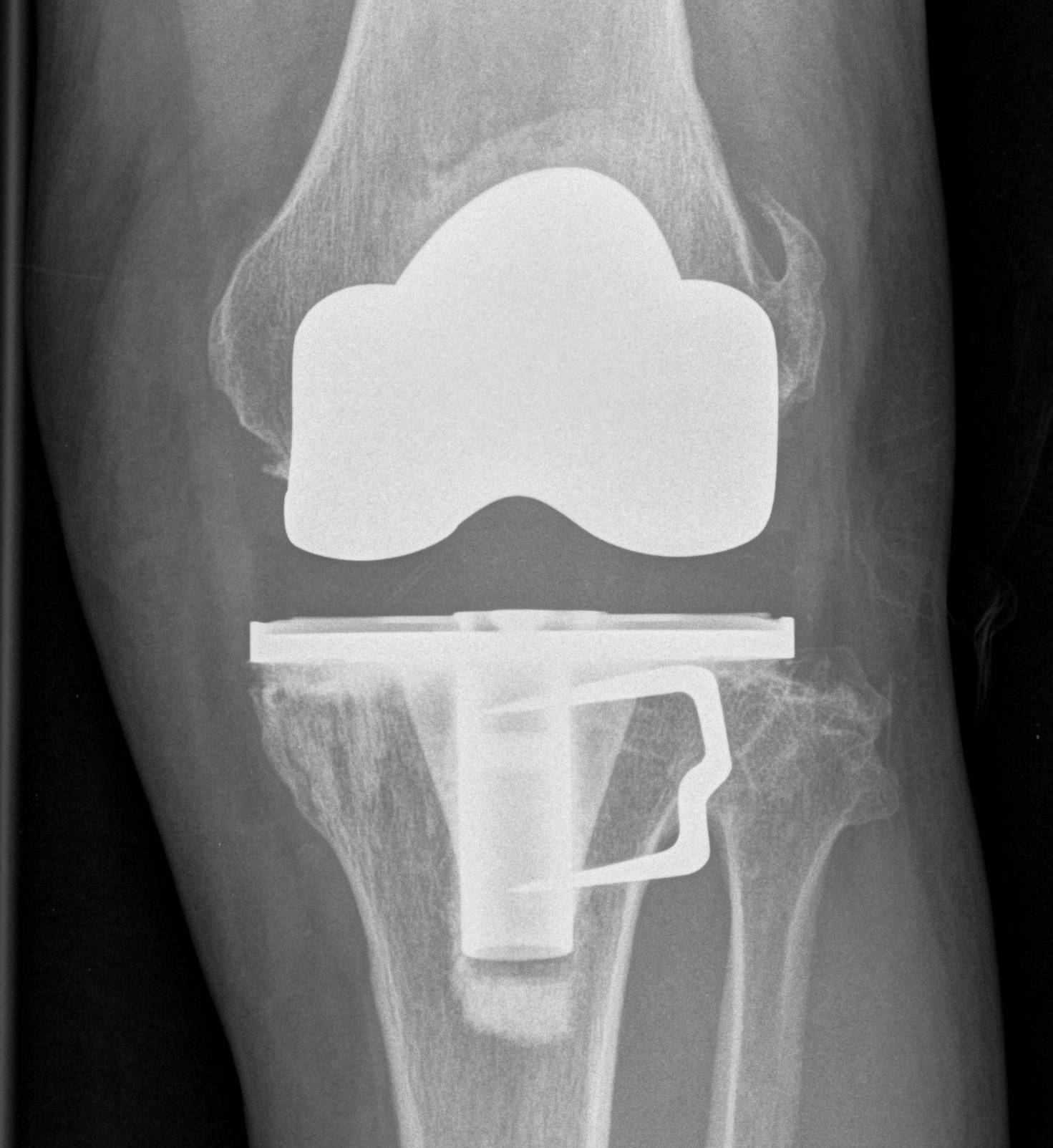
1. Decreased tibial bone stock
Lateral closing wedge
- loss of lateral bone stock
- may rarely need augments
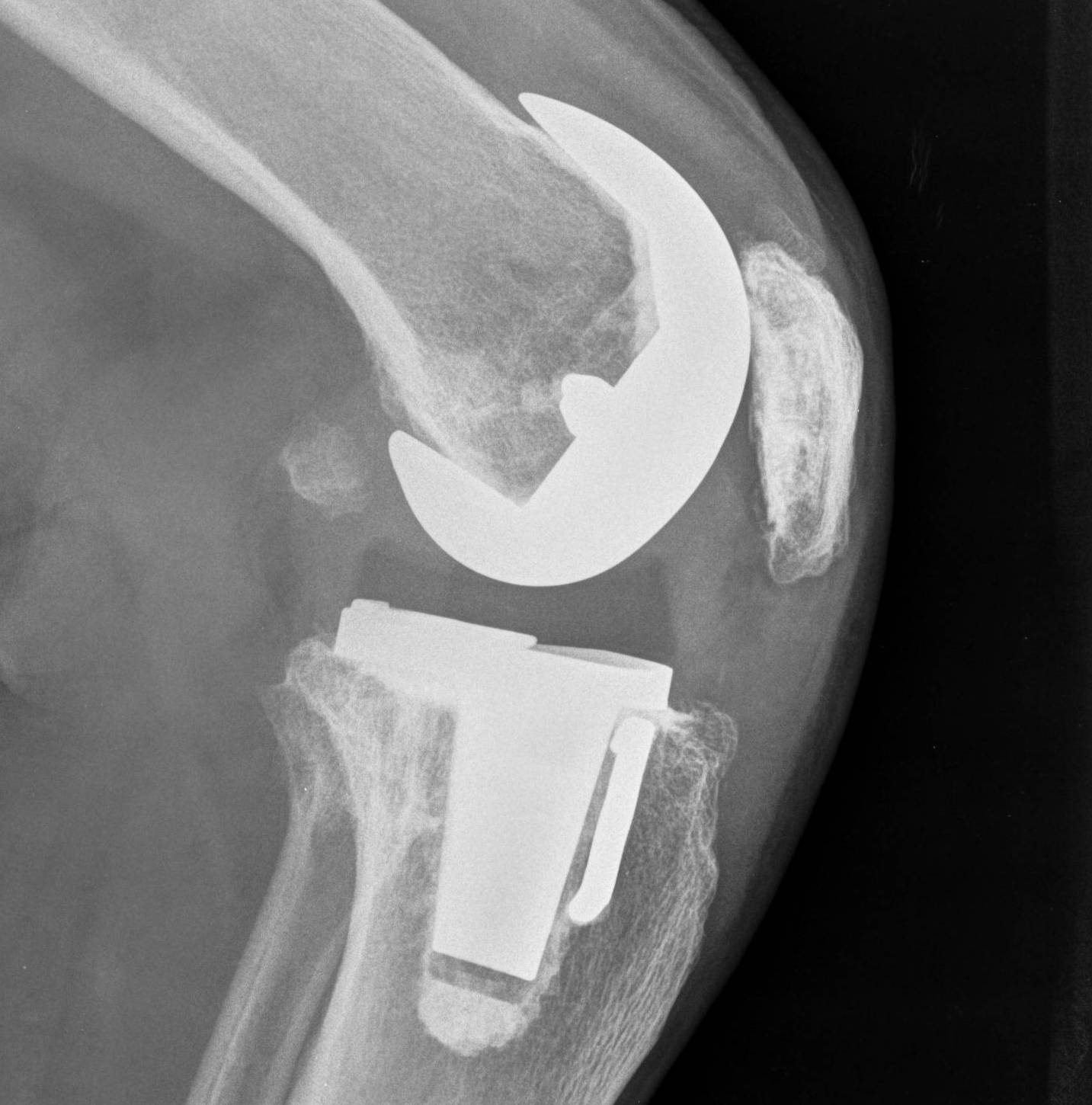
2. Anterior tibial slope
Due to incomplete posterior osteotomy closure
- need to be aware
- ensure correct slope with bone cuts
3. Offset tibial shaft medially
Seen with closing wedge
- need offset stem to avoid lateral overhang
- more common when large corrections have occurred
- have revision stems available
Soft tissue Balancing
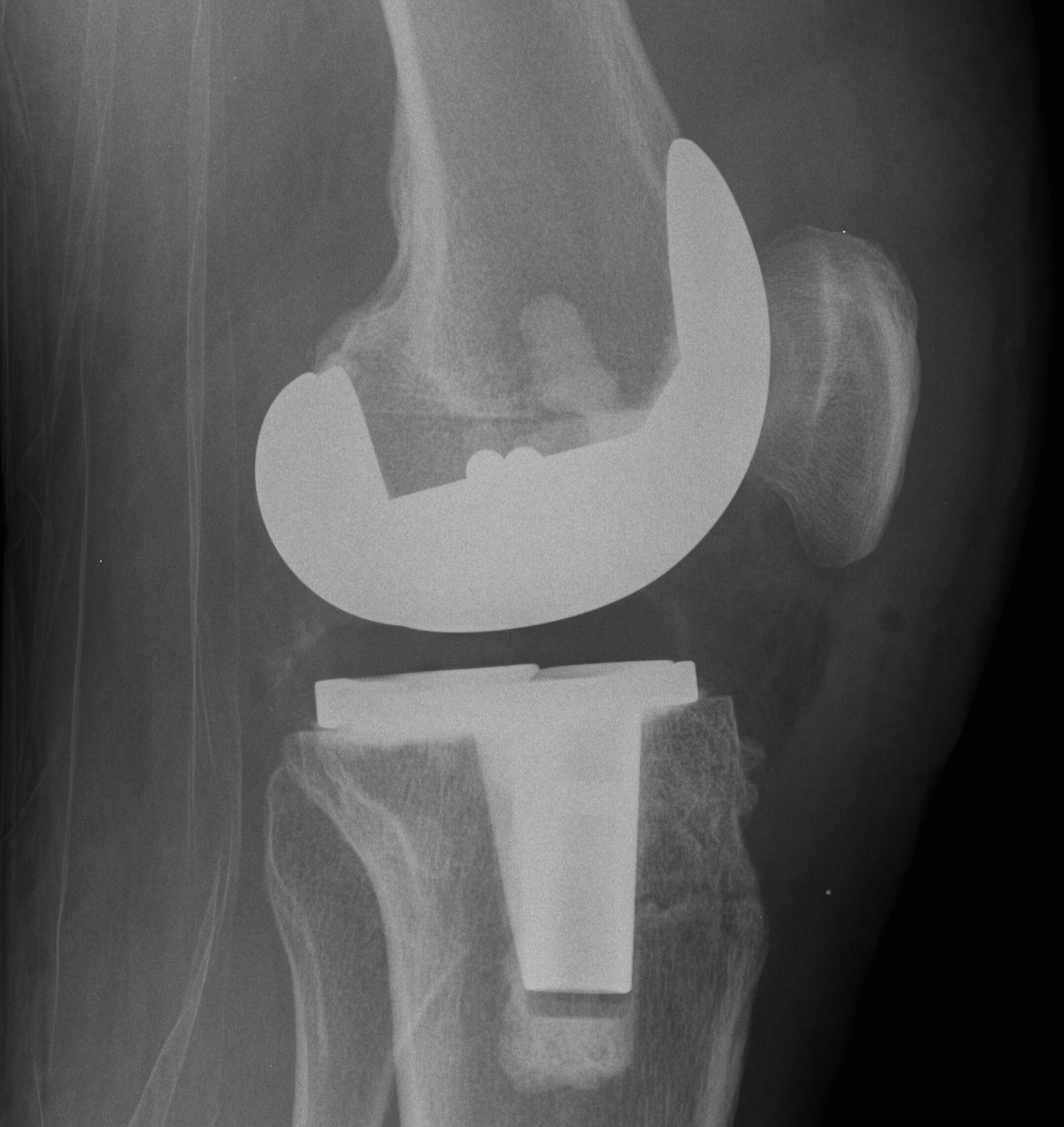
Valgus knee alignment
- need appropriate releases
Soft tissue balancing
- restoring the tibial slope
- difficulty with flexion / extension balancing
- may need higher constraint


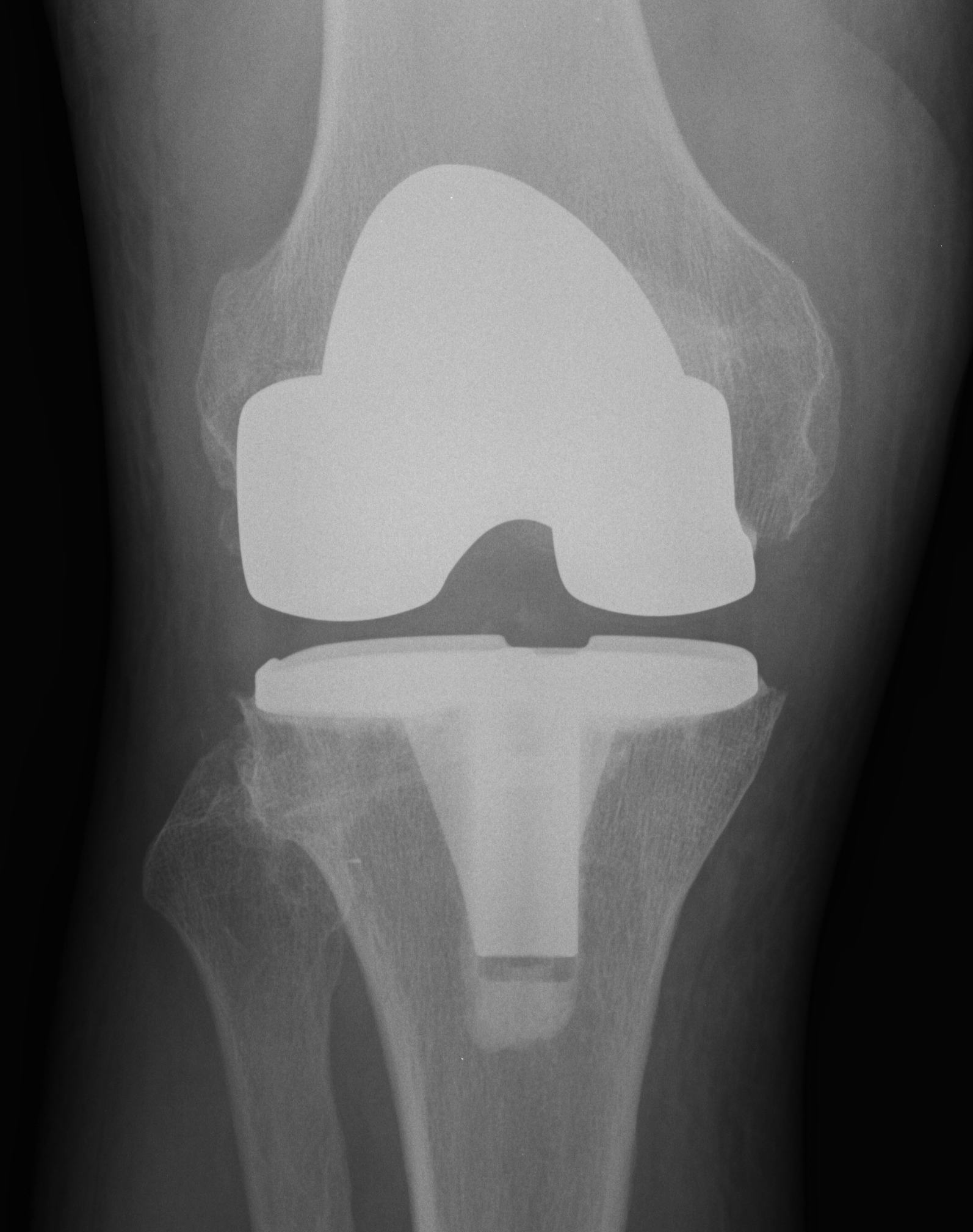
Results
Controversial
- conflicting reports
Outcomes
- 39 patients undergoing bilateral TKA after unilateral HTO
- at mean of 7.5 years, no difference between two groups
- systematic review of TKA after HTO
- no difference in outcome between opening and closing wedge
- more intra-operative technical issues with closing wedge
- higher incidence quadriceps snip / tibial tubercle osteotomy / lateral soft tissue release
Survivorship
- meta-analyis of primary TKA versus TKA following HTO
- no difference in complication rates
- worse ROM and long term survival rates with TKA following HTO
UKA versus TKA
El-Galaly et al Acta Orthop 2020
- Norwegian registry
- 1000 TKA following UKA: 88% 5 year survival
- 1000 TKA following HTO: 94% 5 year survival
