Definition
A valgus knee has a tibiofemoral angle of > 10o
Causes
Inflammatory
- RA
Osteomalacia
- rickets, renal
Trauma
- tibial malunion
- plateau fracture
Childhood
- physeal arrest
HTO
Primary OA
- most common
- females
- unresolved physiological valgus deformity
Pathology
Soft tissue abnormalities
A. Contraction of lateral structures
- ITB
- LCL
- Popliteus
- PL capsule
- Lateral head gastrocnemius
- Lateral IM septum
- Long head of biceps
B. Lax medial structures
Bony abnormalities
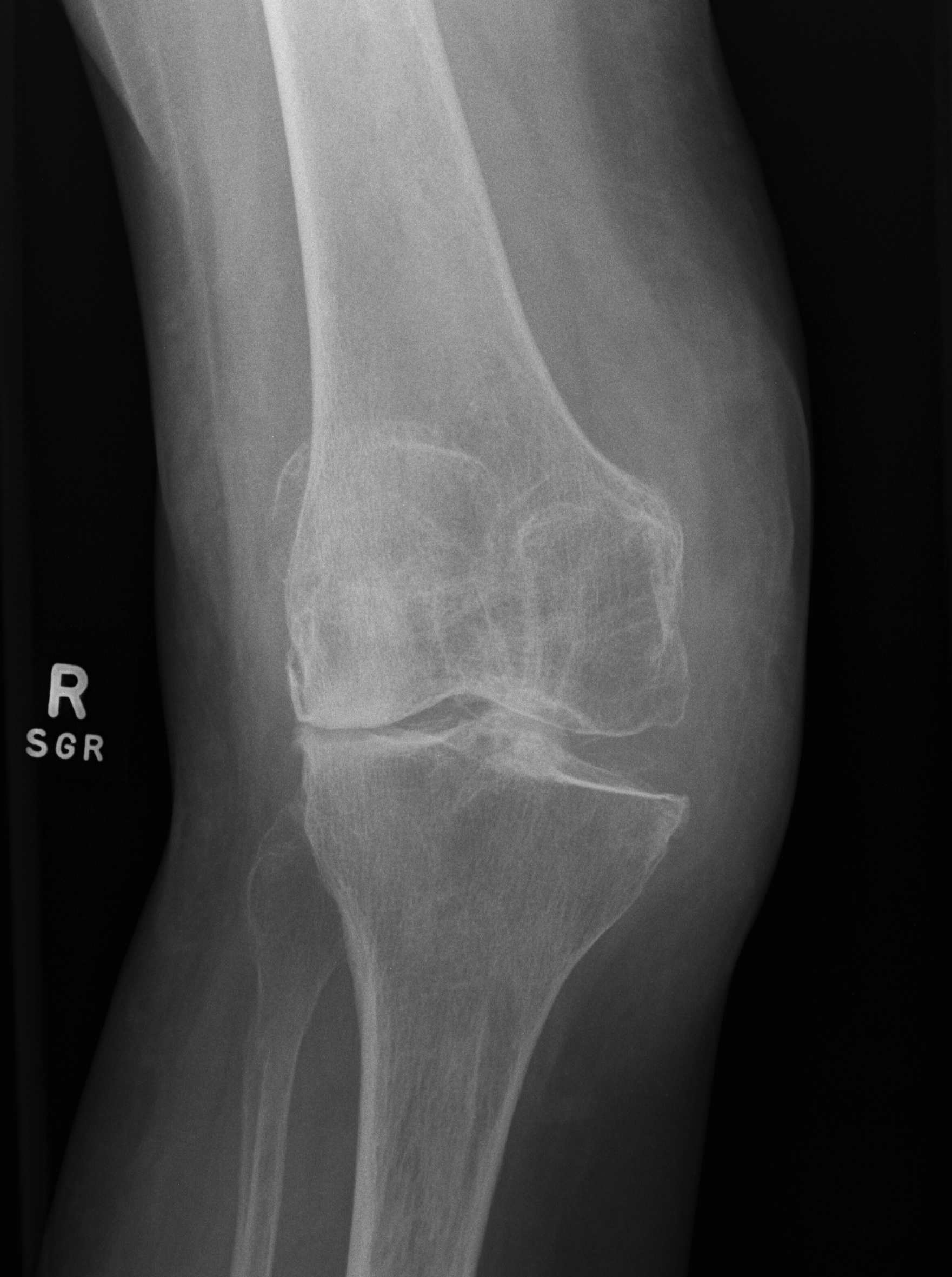
A. LFC hypoplasia
- beware posterior condyle referencing
- cause IR of the femoral component
- use Whiteside's AP axis / epicondylar axis
B. Posterior aspect lateral tibial plateau
Krackow Classification
Type 1 / Lateral bone loss
Type 2 / MCL deficient
Type 3 / Secondary to HTO
Surgical Problems
1. Approach
Medial approach
Advantage
A. Easy to evert patella because
- increased Q angle
- tibial tuberosity lateralised
Disadvantage
A. More difficult to reach contracted lateral side
B. If perform lateral release, risk devascularising the patella
C. Must not perform any medial release
Lateral approach Keblish 1991
Advantage
A. Direct access to lateral structures
- makes these easier to release
B. Preserves blood supply to patella
Disadvantage
A. Wound closure at end of case
- not enough capsule to close after correction valgus
- closing only skin and soft tissue, may need to utilise the fat pad
Keblish Technique
- midline incision
- lateral release along lateral border of patella
- coronal z step cut in vastus lateralis
- is 6 - 9 mm thick
- lower 50% taken off patella
- superficial 50% attached to patella
2. Bony alignment
Rotation
- deficient LFC
- don't use posterior condylar axis to set rotation
- use Whiteside's AP axis and epicondylar axis
- can place a osteotome under LFC when placing sizing block
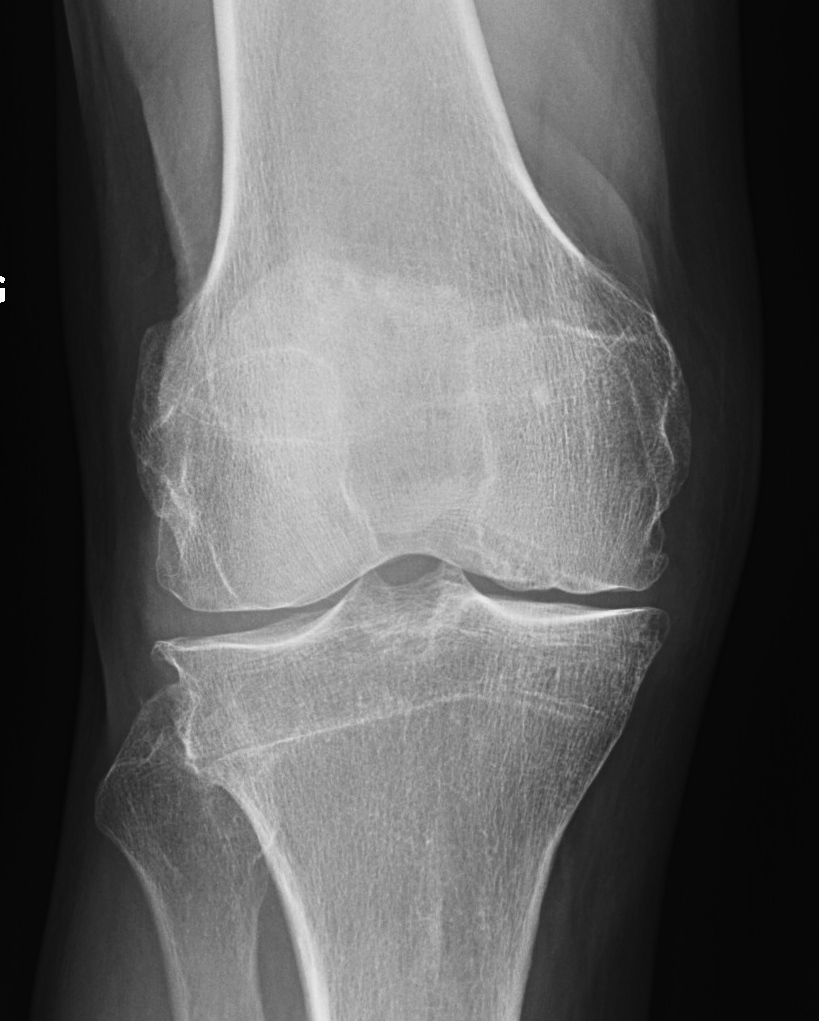
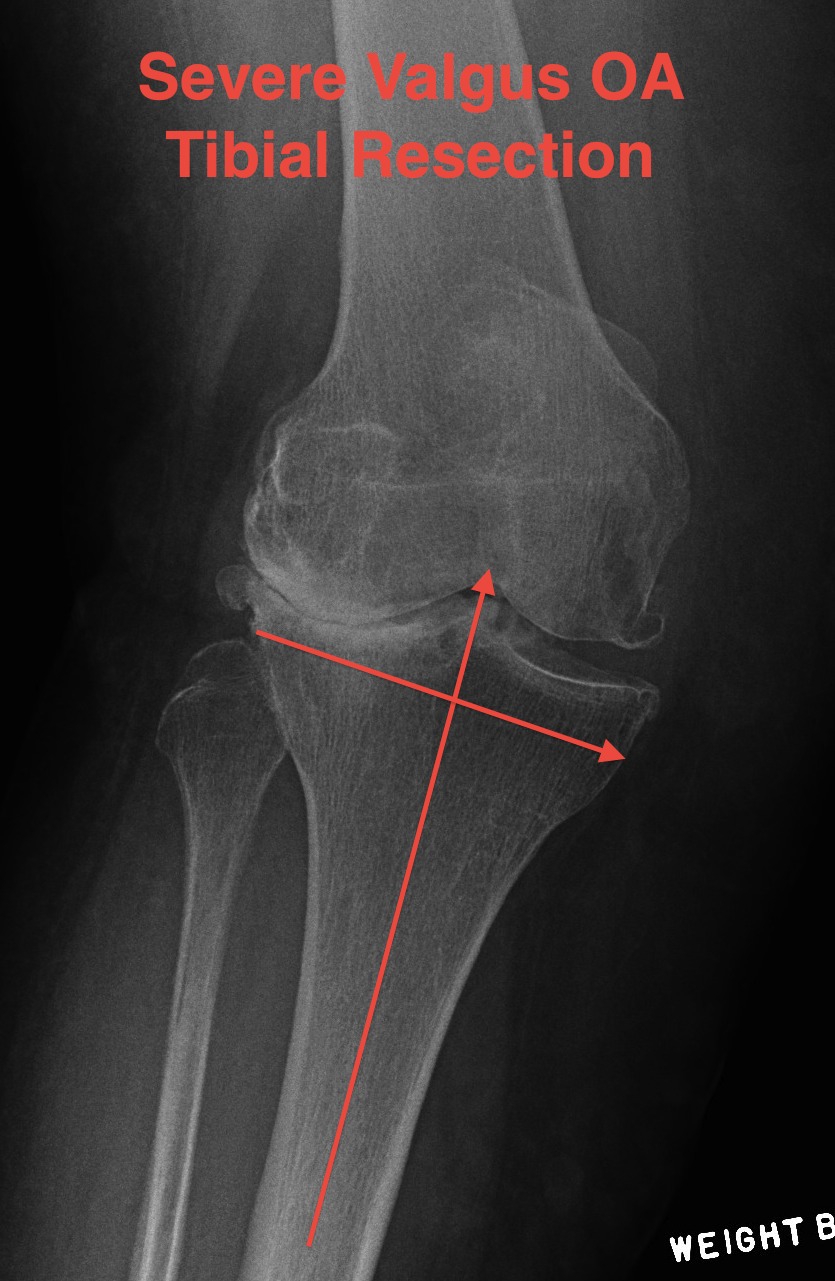
Tibial resection
- don't take 10 mm as bone worn laterally in valgus OA
- can't take 2mm off medial side as is the normal side
- need to estimate
- take 6 mm from lateral tibia intially, stay above fibula head
- much more symmetric proximal tibial resection
- use trial blocks to assess flexion / extension gaps
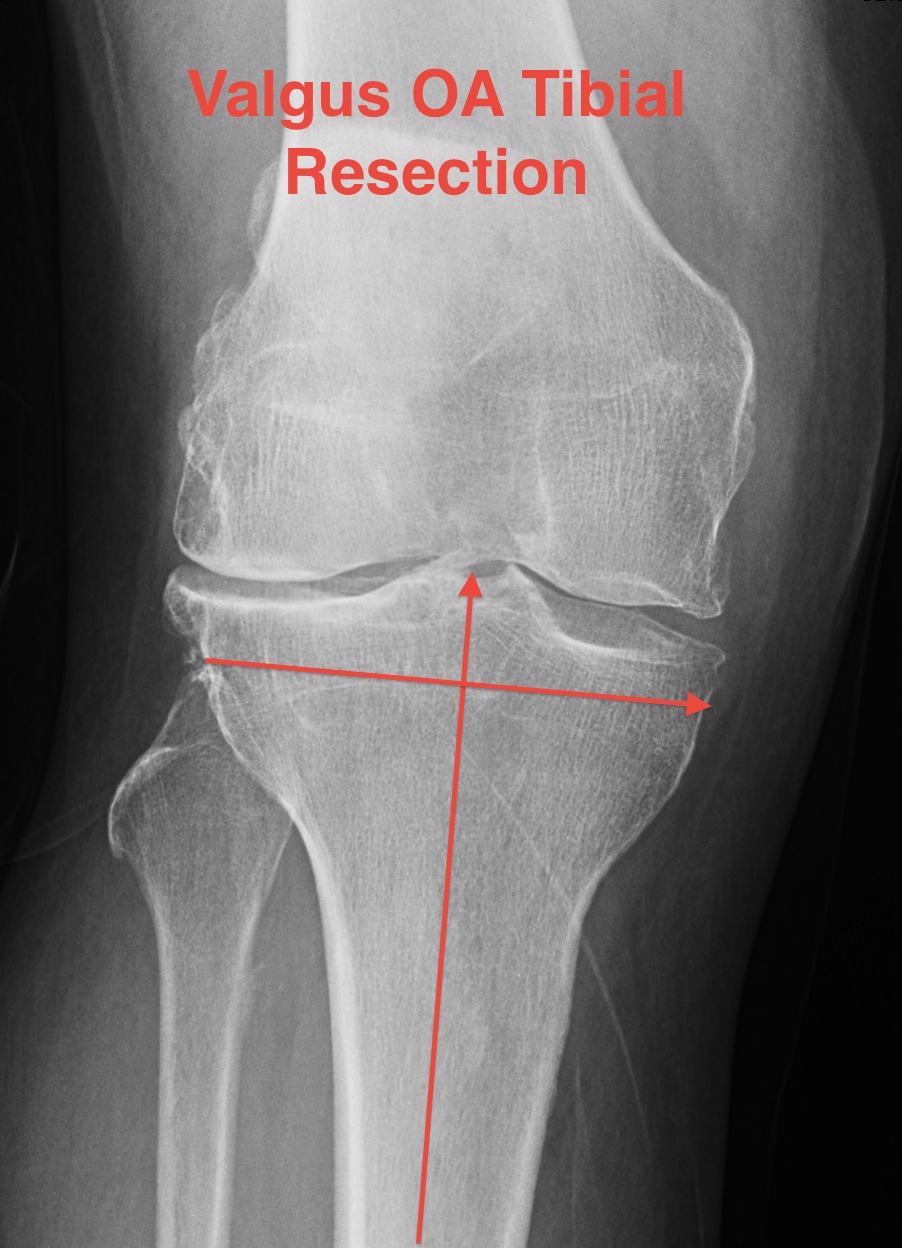
Deficient lateral tibial plateau
- don't take > 10 mm medial plateau
- will get down into soft bone
- preop plan
- may need augments laterally and therefore stems
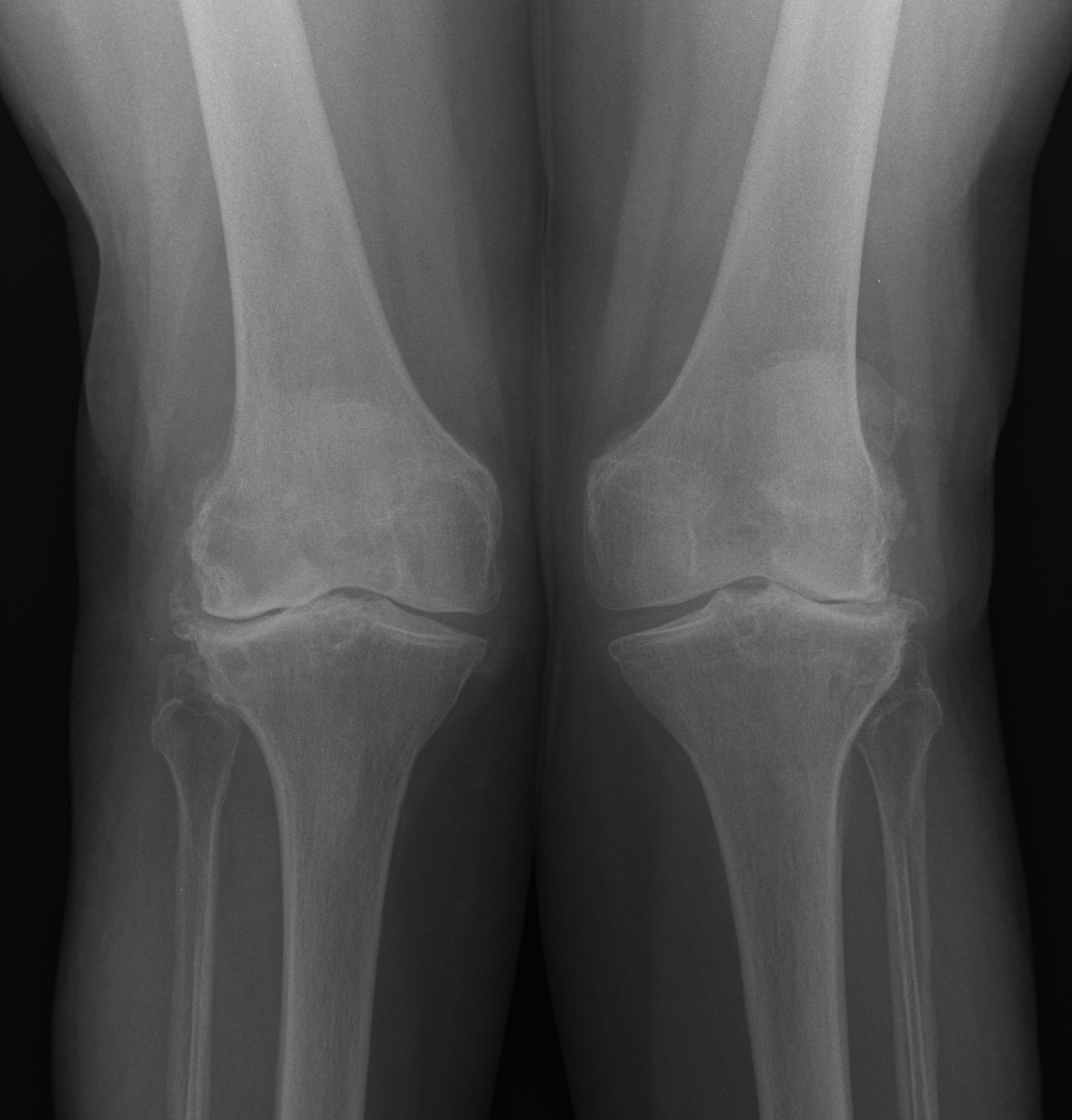
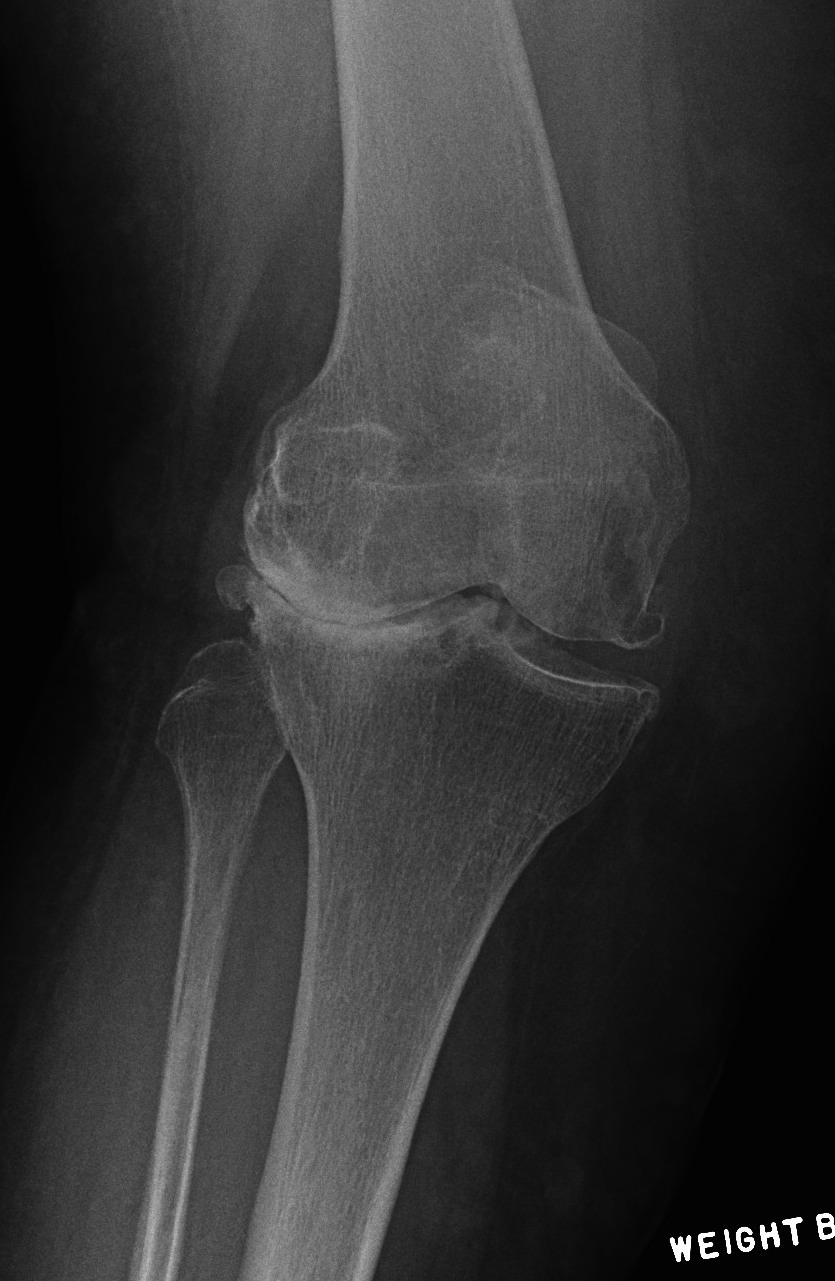
- below xray is borderline / but just ok
3. Soft tissue balancing
Best to sacrifice PCL early
Tight Extension
- pie crust or release ITB
- +/- lat gastrocneumius off femur
- +/- Z lengthen biceps
Tight Flexion
- PL corner
- release popliteus proximally
Tight Extension & Flexion
- release LCL from lateral epicondyle
- usually done last
- periosteal sleeve as per popliteus
4. Management MCL Deficiency
A. Young Patient
Tighten MCL
- advance femoral insertion (Krackow)
- cut mid-substance and imbricate (Krackow)
- take off femur with bone plug / advance
CCK Prosthesis
- acts as an internal splint whilst MCL heals
B. Older patient
Consider hinged prosthesis
5. Prosthesis
PS to aid balancing
CCK / MCL Deficient
Augments / lateral bone loss
5. Patella tracking
Tends to track laterally after correction
- resurface / place button medially
- lateral release may be required
- issue if have done medial approach
- may get patella AVN
6. CPN
Need to check in recovery
- splint the knee in flexion post operatively
Complications
ML instability
- release too many lateral structures
- can develop late
- incidence 6-25%
- may need CCK on hand
Avoid by
- pie crusting ITB
- releasing popliteus / LCL as sleeve
Recurrent / residual valgus
- prone to maltracking
Wound healing
Patella maltracking
Patella fracture
- secondary to AVN from medial approach and lateral release
Stiffness
CPN
- more common if valgus > 12o


