Epidemiology
Traumatic initial cause in 95%
M:F 2:1
Age of initial dislocation inversely related to recurrence rate
- patients younger than 20 have a redislocation rate of 90%
- between 20 - 40 years, redislocation rate of 60%
- patients > 40 years have a 10% rate of dislocation but a higher rate of cuff tears (up to 40% in patients > 60yrs)
Anatomy & Stability
1. Passive Stabilisers
Glenoid labrum
- significant deepening by 50%
- labrum attaches capsule / ligaments / biceps
Negative intra-articular joint pressure
Joint fluid adhesion/ cohesion
Capsule
- attaches to SNOH
Coracoacromial arch
- prevents superior displacement
Coracohumeral ligament
- attaches base of coracoid
- to lesser and greater tuberosity
- passess through rotator interval between SS and SSC
- static restraint to anteroinferior translation in the adducted shoulder
Capsulo-ligamentous structures
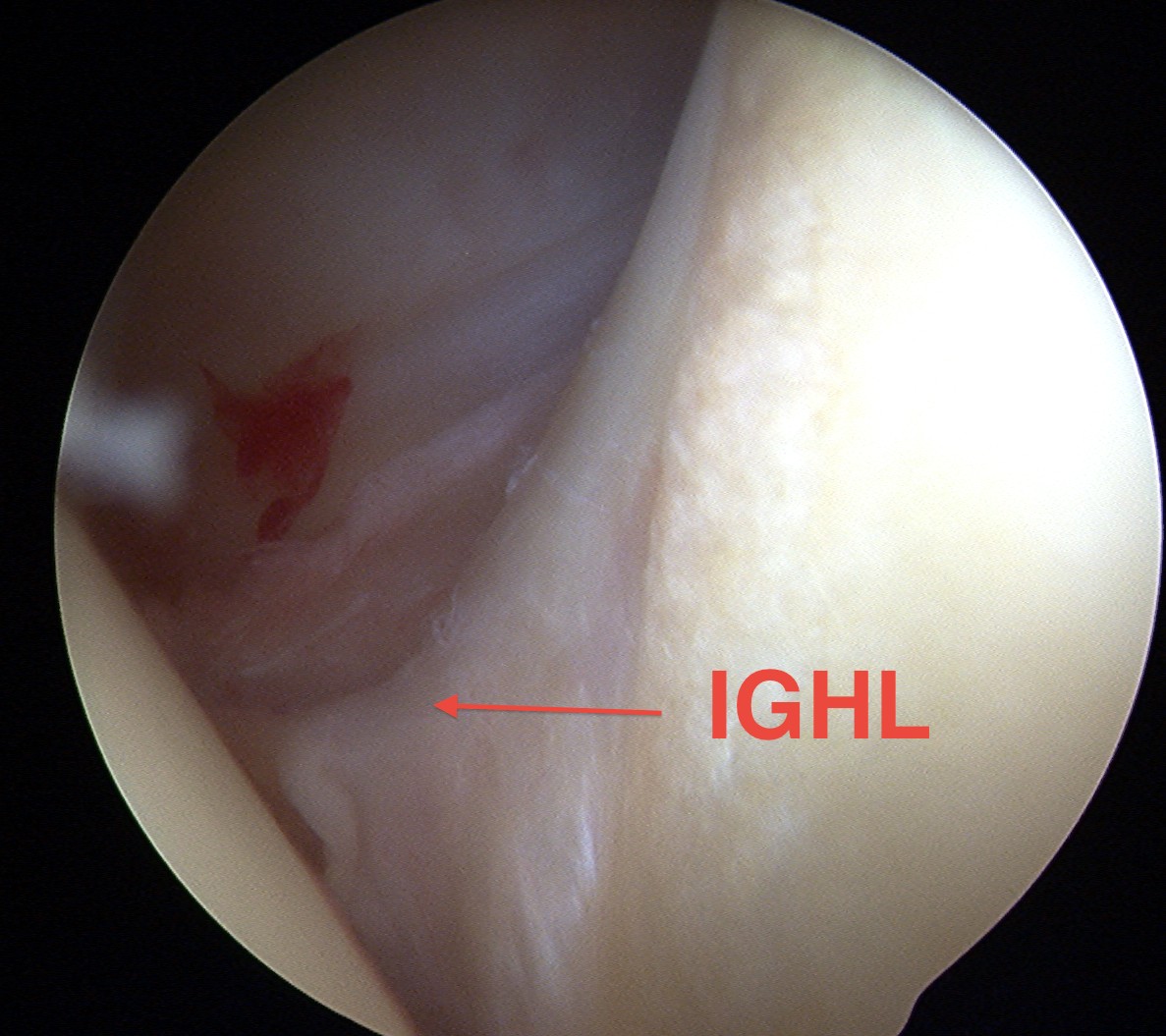
1. IGHL
Most important
- resists anterior translation in abduction and ER
- anterior & posterior band with sling between
- anteror band limits ER at abduction > 90°
Origin
- anterior band glenoid 3 o'clock
- posterior band 9 o'clock
Insertion
- inferior anatomical neck / head
2. MGHL
Action
- behind SSC
- 2° restraint anterior translation
- limits ER at 45° Abduction
- present in 60% population
Origin
- supraglenoid tubercle below SGHL
Insertion
- medial to LT
3. SGHL
Action
- adjacent to biceps tendon
- prevents inferior subluxation
- functions only in adduction
- no function in decreasing anterior translation
- present 50% population
Origin
- supraglenoid Tubercle
Insertion
- LT
2. Dynamic Stabilisers
Rotator Cuff
- SSC resists anterior translation
- compresses head into glenoid socket
LH Biceps
Deltoid
- especially when arm is elevated 90o
Scapular Rotators
- move glenoid into stable position
Pathology
No essential pathological lesion responsible for every recurrent subluxation or dislocation
Thomas and Matsen Aetiology Classification
AMBRII
- Atraumatic, Multidirectional, Bilateral
- Rehabilitation, Inferior capsular shift, closure rotator Interval
TUBS
- Traumatic, Unidirectional, Bankart, Surgery
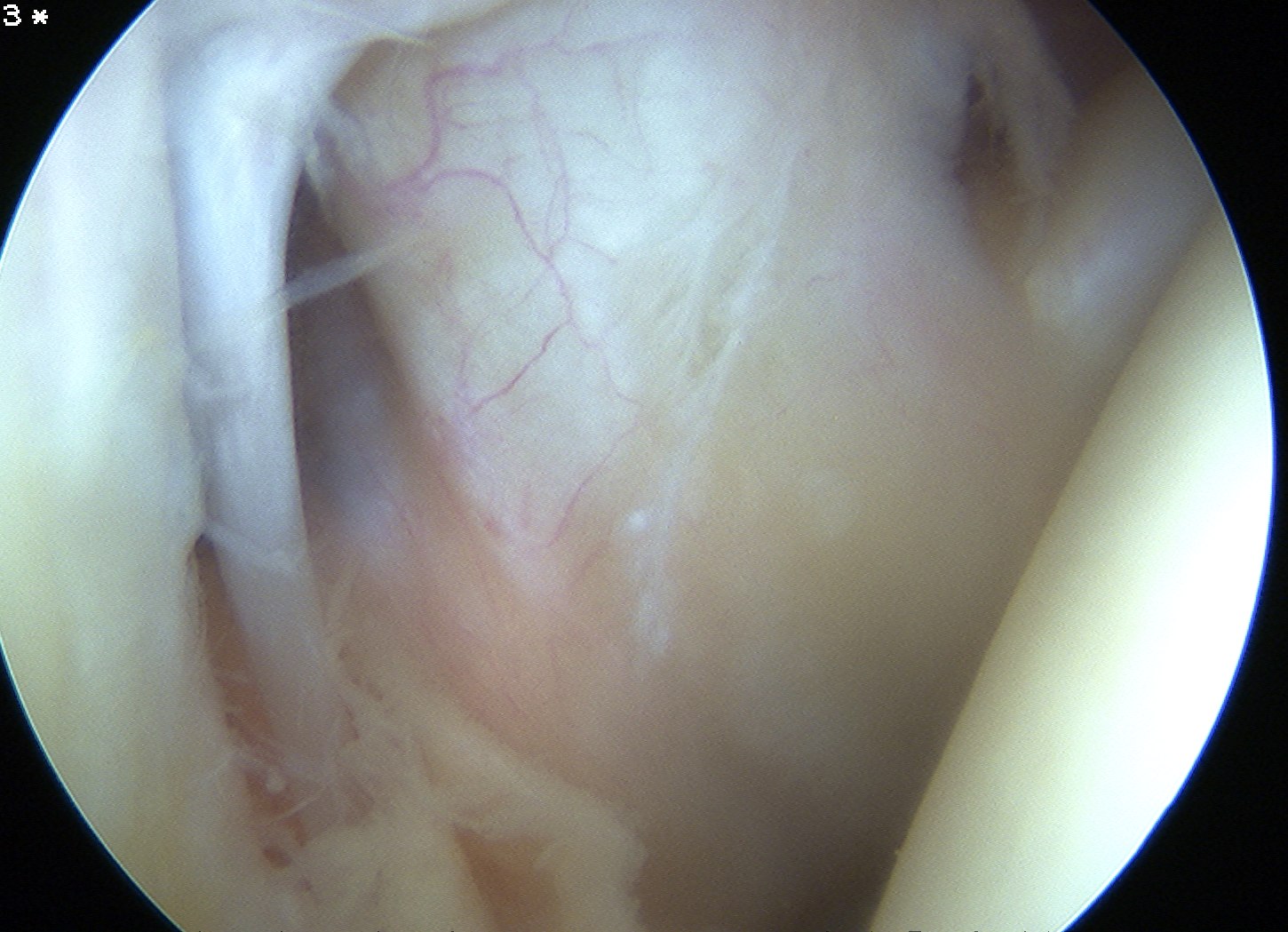
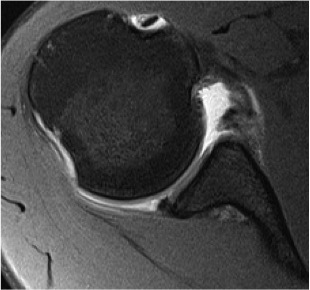
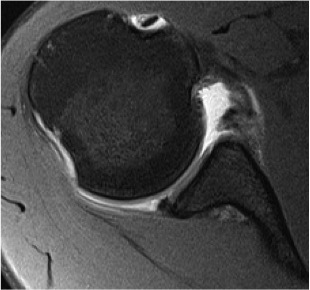
1. Labrum / Ligament / Capsule
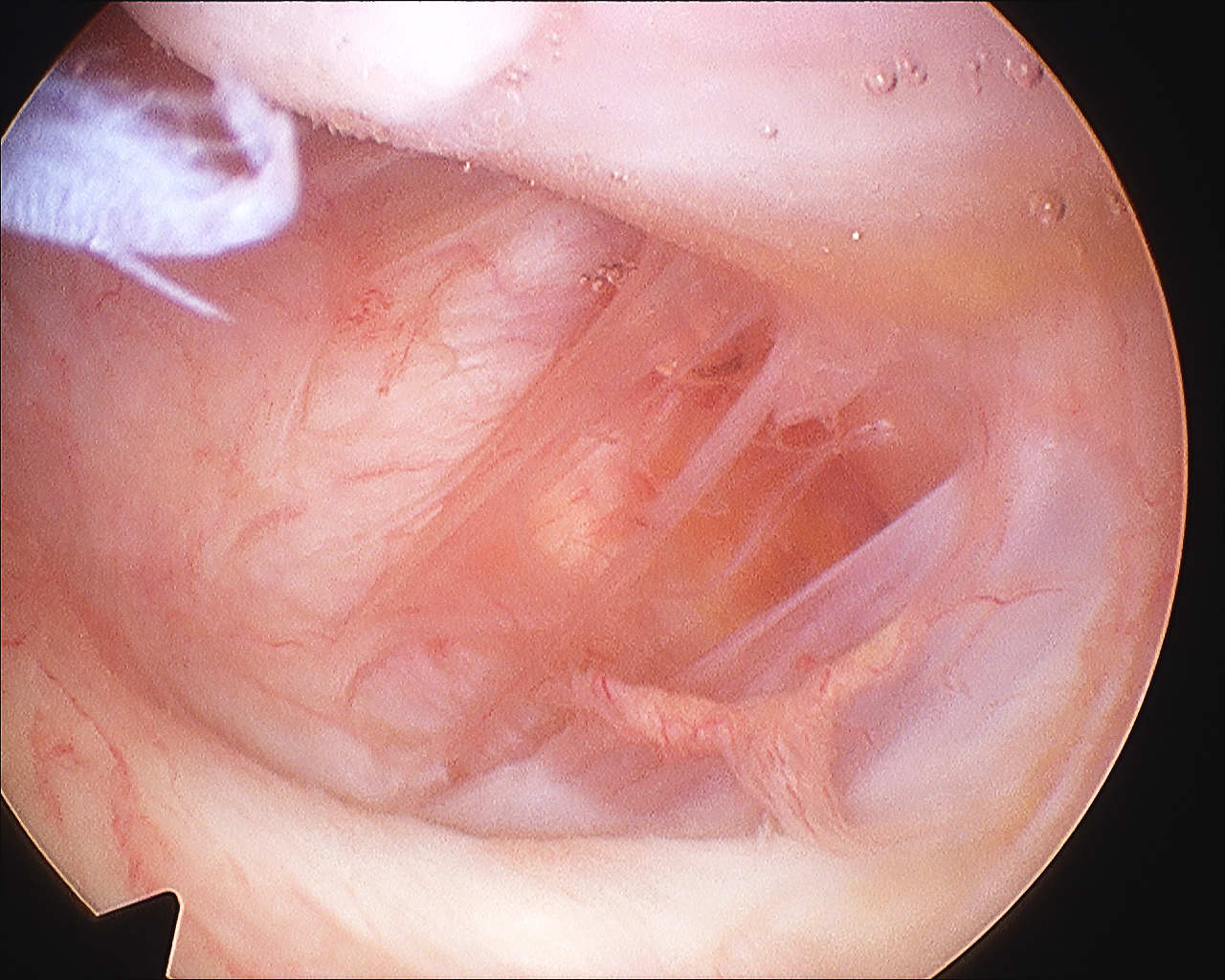
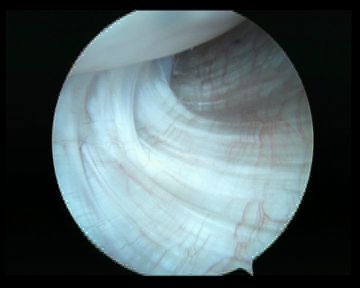
A. Bankart lesion
Pathology
- described in 1938
- humeral head forced through capsule
- humeral head tears fibrocartilaginous labrum from almost entire anterior 1/2 of glenoid rim
- is an IGHL avulsion
- usually between 3 and 6 o'clock
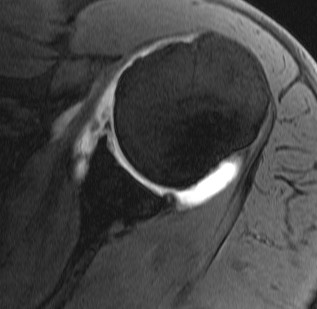
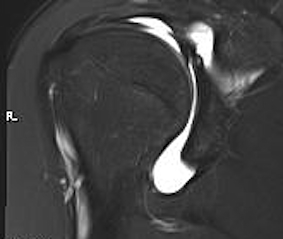
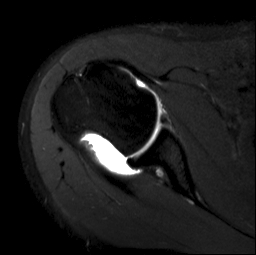
MRA
- see detachment of anterior labrum
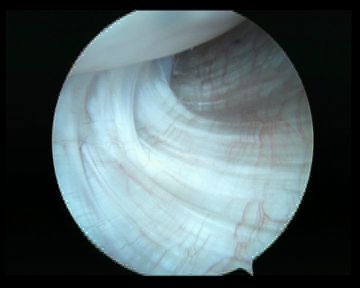
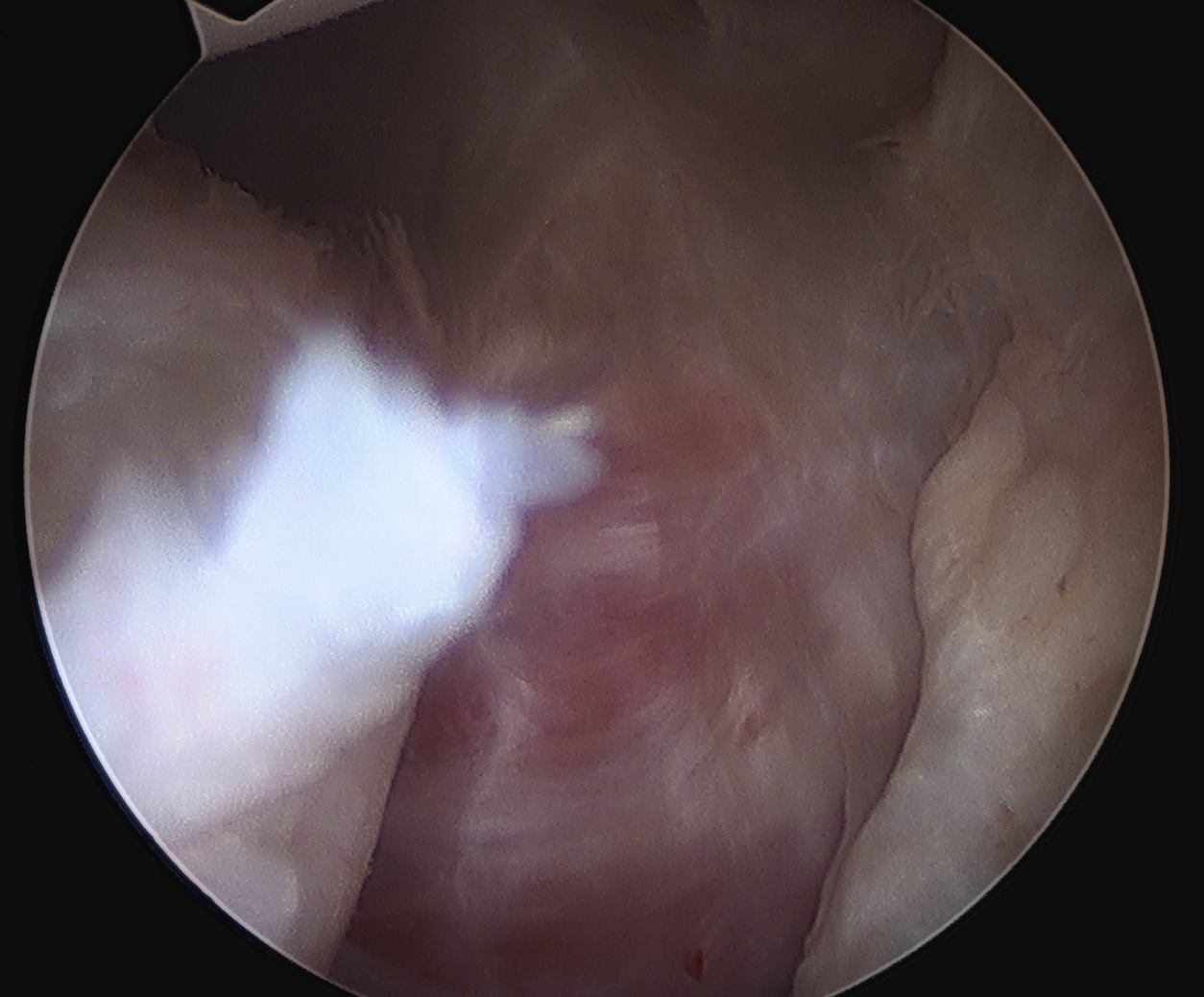
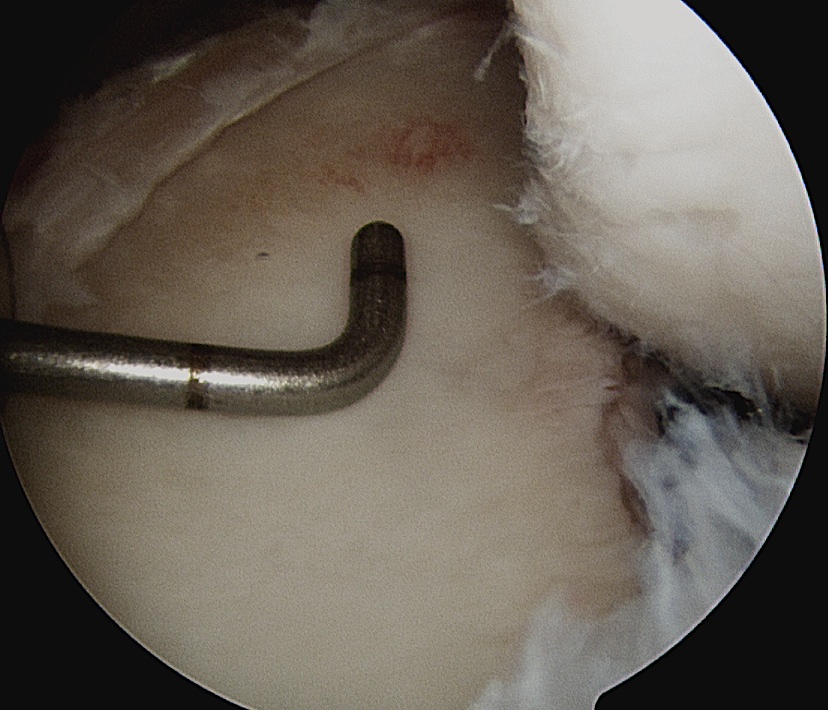
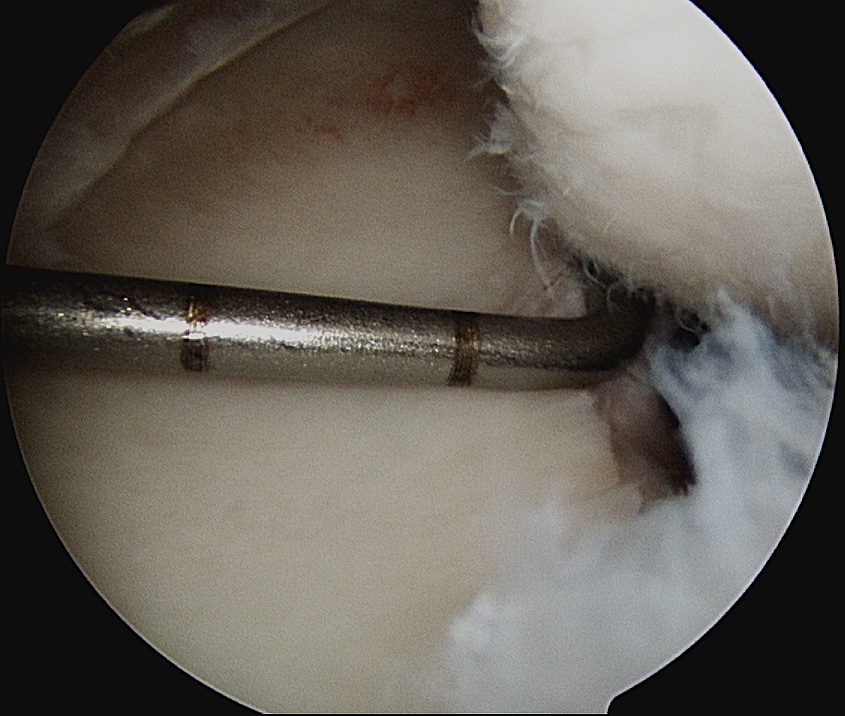
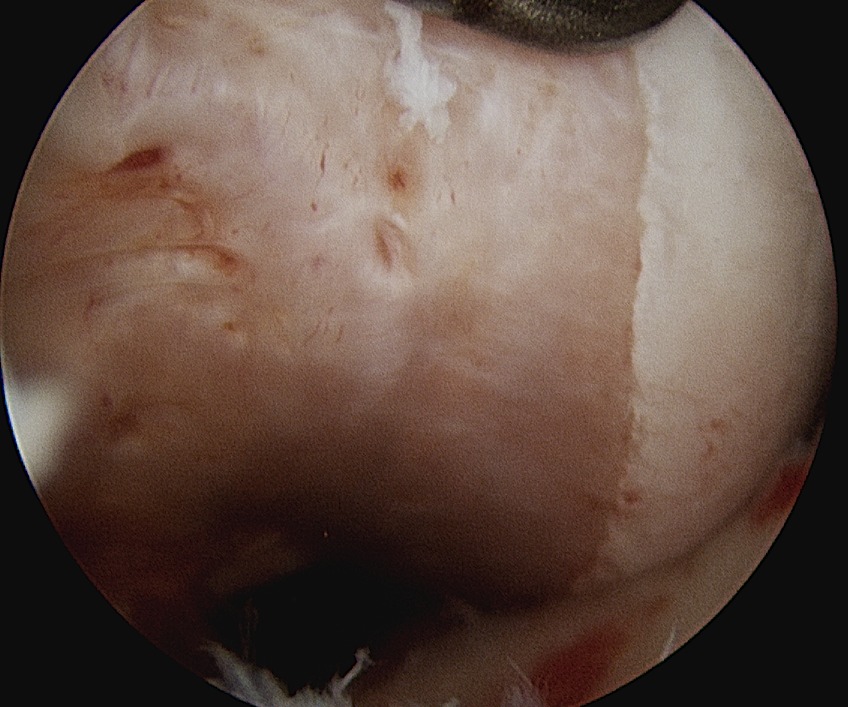
Arthroscopy
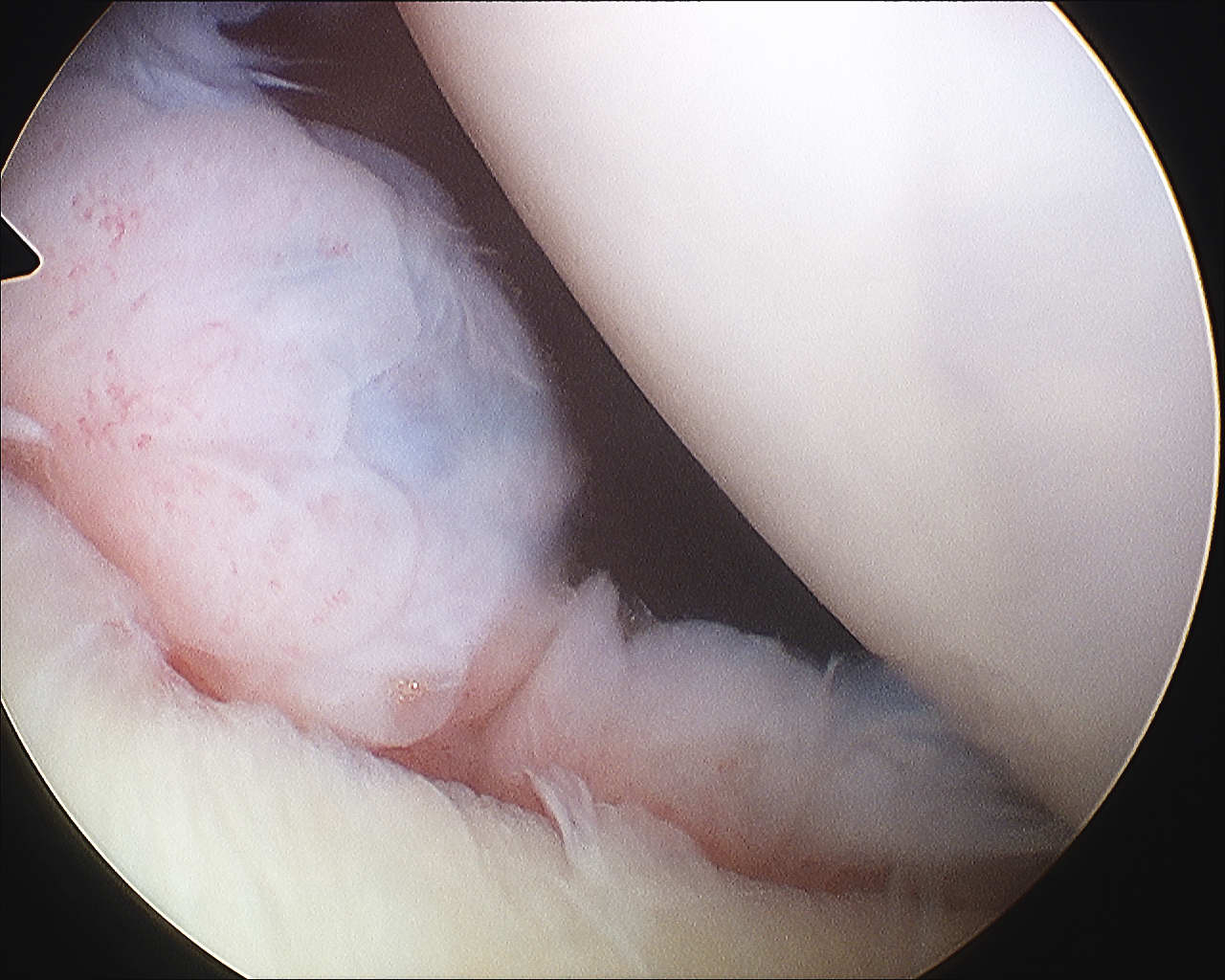

Incidence
- present in 85% traumatic recurrent dislocations
- may be associated with avulsion fracture of glenoid rim / bony bankart
B. Excessive Capsular laxity
Incidence
- may be present alone or with Bankart lesion
- 30% have both
- 85% previous failed surgical procedures
Causes
- congenital collagen deficiency / MDI
- plastic deformation of capsuloligamentous complex
- single macro-traumatic event or repetitive micro-traumatic events
C. Capsular Tears
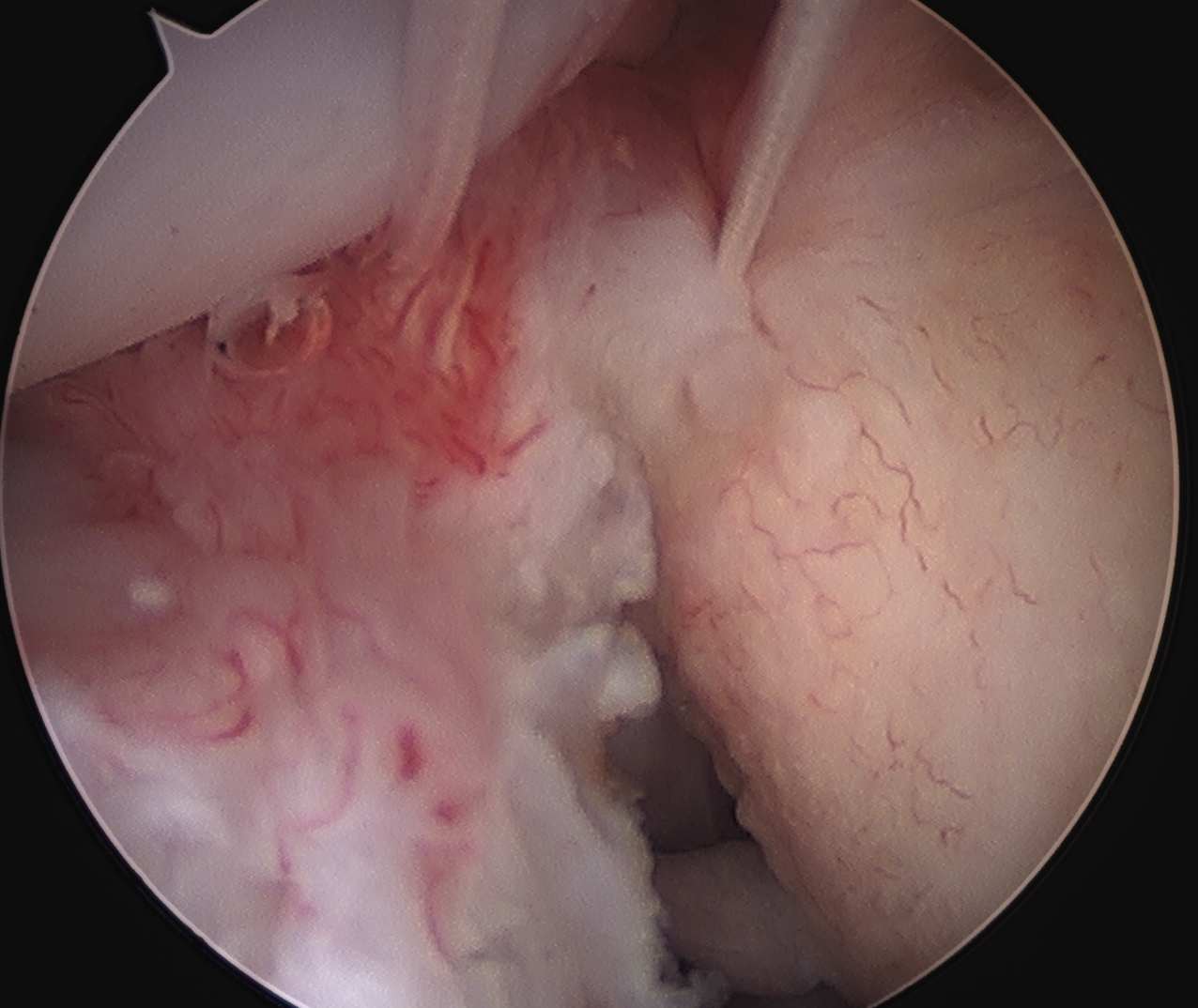
D. HAGL
Definition
- avulsion of IGHL from anterior humeral neck
- Humeral Avulsion of Glenohumeral Ligament
Incidence
- 2 - 10%
Associations
- can be in combination with anterior bankart (Floating IGHL)
- association with subscapularis tear
Xray
- may see bony avulsion
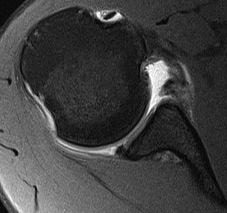
MRA
- enlarged inferior pouch
- discontinuity of IGHL / J sign


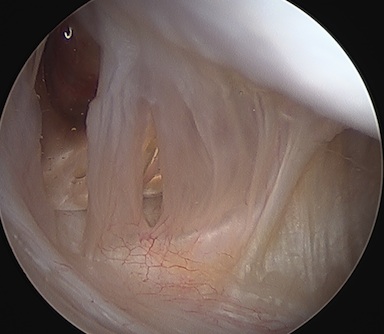
Arthroscopy
- will see exposed subscapularis muscle
Management
A. Open Repair
- take down SSC
- repair via bone anchors to inferior neck
- can cause limitation ER
B. Arthroscopic repair
- 70o scope and 5 o'clock portal
E. Bankart Variations
ALPSA
- anterior labrum periosteal sleeve avulsion
- labral-ligamentous structures shifted medially
- roll up under the periosteum
Perthes Lesion
- stripping of the scapular periosteum medially
- labrum may or may not be attached

GLAD
- glenoid labrum articular disruption
- damage to the glenoid cartilage
- labrum undisplaced

F. Muscle
Cuff Tears
- Present as pain or weakness
- > 40 years = 30%
- > 60 years > 80%
Increased Rotator Interval
- between SS and SSC
- tends to open up with AMBRI
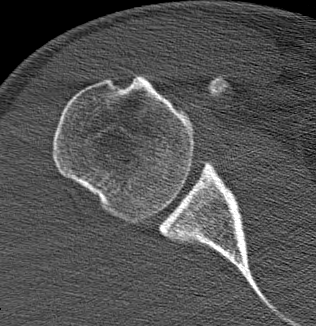
2. Bony
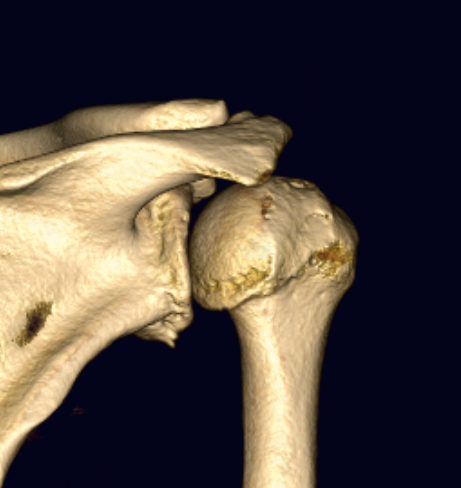
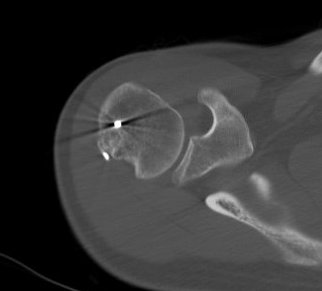
A. Bony Bankart
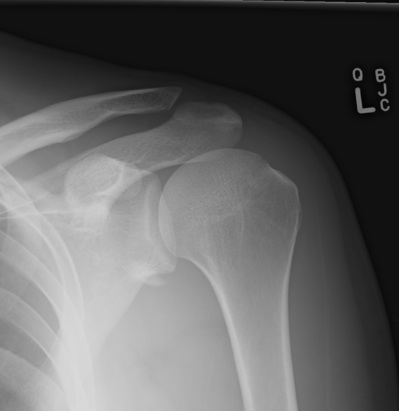
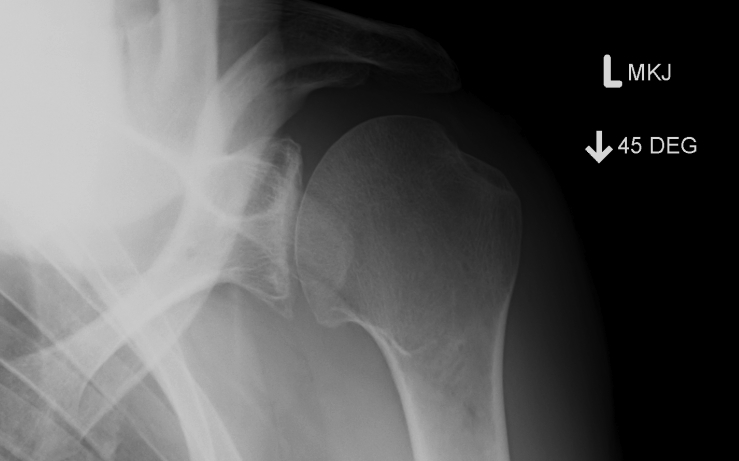
Xray
- AP
- Garth (aim beam caudally)

Importance
- large bony bankart increases risk of failure of soft tissue bankart repair
Diagnosis
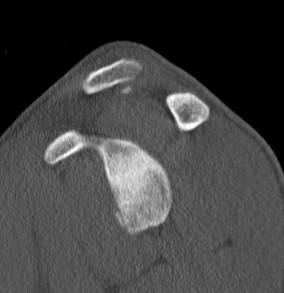
- may need CT to decide the size best
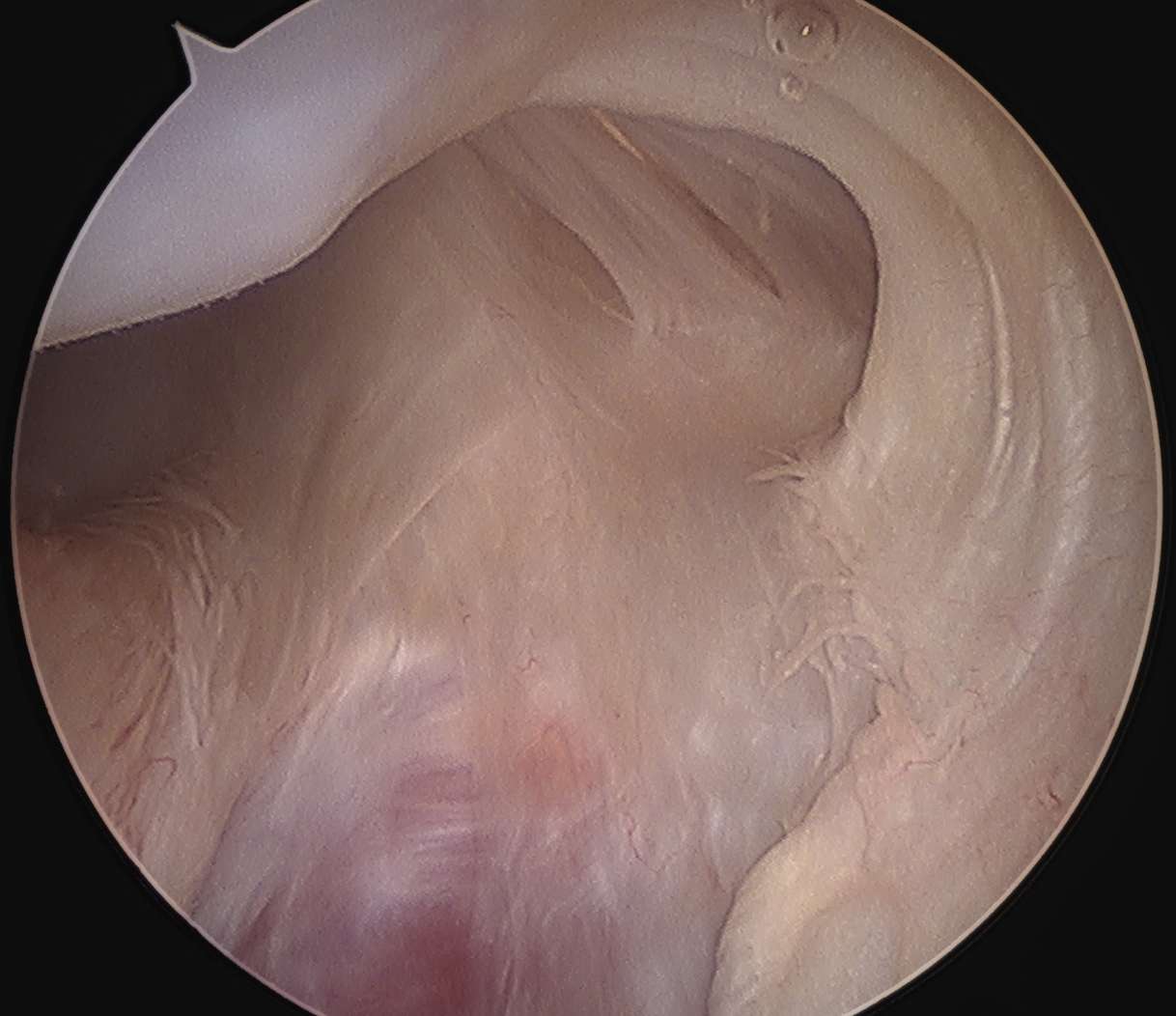
Burkhart and De Beer Arthroscopy 2000
- described the inverted pear appearance
- loss of bone antero-inferior
Small
Large



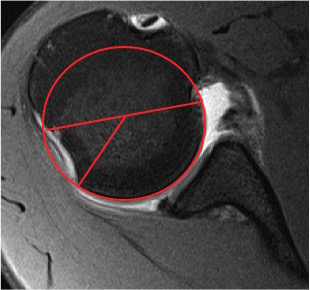
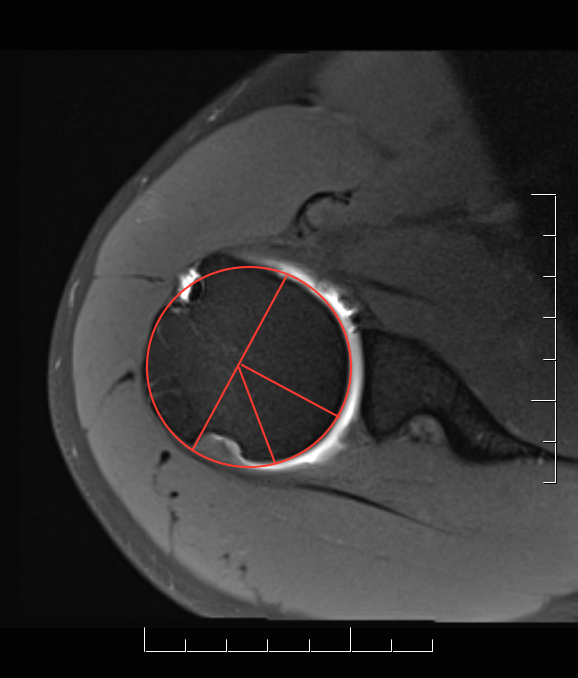
Size calculation

Lo Parten and Burkhart, Arthroscopy 2004
- calculation of percentage bone loss arthroscopically
1. Inferior glenoid is nearly a perfect circle
- centre is the bare area of the glenoid
- measure anterior radius v posterior radius at this level
2. Calculate the diameter of the inferior circle
- twice the posterior radius
3. Calculate the difference between anterior and posterior radius
The average diameter is 24 mm
- hence 12 mm posterior and 12 mm anterior
- if lose 8 mm anteriorly
- 12 mm posterior and 4 mm anterior
- calculation is 8/24 = 30%
Risks
25% loss and above poor prognostically
- means approximately 7.5 mm anterior bone loss
< 4mm anterior to bare area
- > 30%
- likely not amenable to soft tissue bankart repair alone
Acute Bankart Repair
Sugaya et al JBJS Am 2005
- demonstrated union of fragment with arthroscopic restoration
- must mobilise fragment, restore anatomically
- otherwise bony procedure
Decision Making
A. Small fragment < 15%
- arthroscopic bankart repair
- can attempt to include fragment
B. Intermediate 15 - 25%
C. > 25%
- must restore glenoid rim
- acute restoration of bony frament or
- bony procedure / Latarjet / Bristow
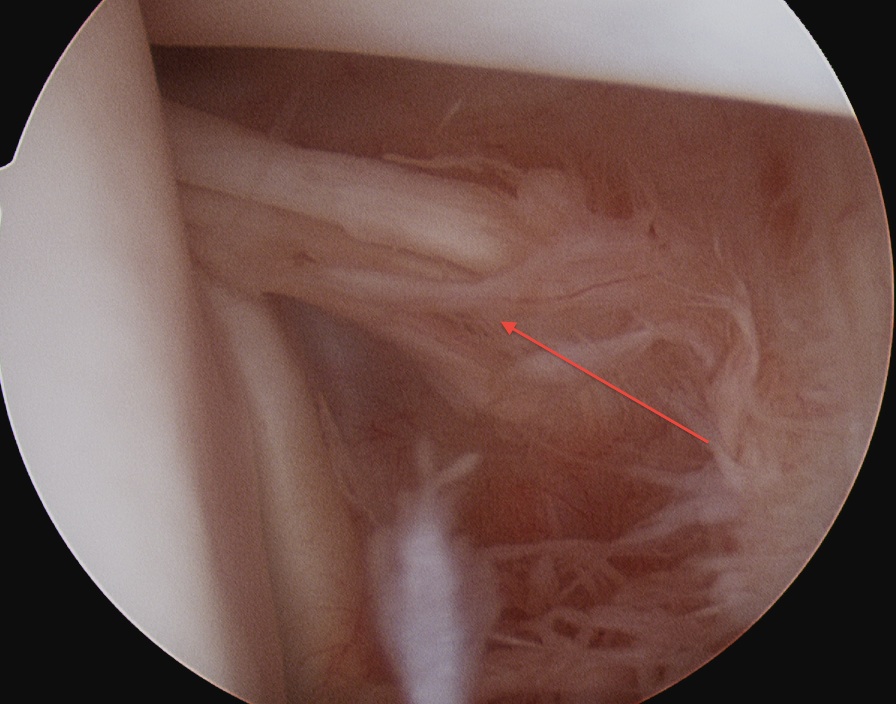
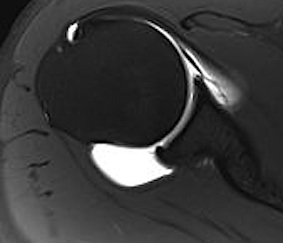
B. Hills Sachs Lesion
Definition
- lesion posterior aspect of head
- where head engages on anterior glenoid
Xray
- AP with IR
- Garth view


CT
Arthroscopy
- cartilage each side of lesion
- this differentiates it from the normal bare area next to infraspinatous

Issue
- large lesion can contribute to dislocation
- head engages defect in external rotation & abduction
Dynamic CT



Measurement
Estimate percentage of articular surface
- concern if 25% or more
Management options for engaging Hill Sachs
1. Posterior capsular advancement / Remplissage
2. Humeral head allograft
3. Anterior Bony Procedure / Latarjet / Bristow
- Hill Sach's lesion unable to engage on anterior glenoid rim
4. Humeral osteotomy
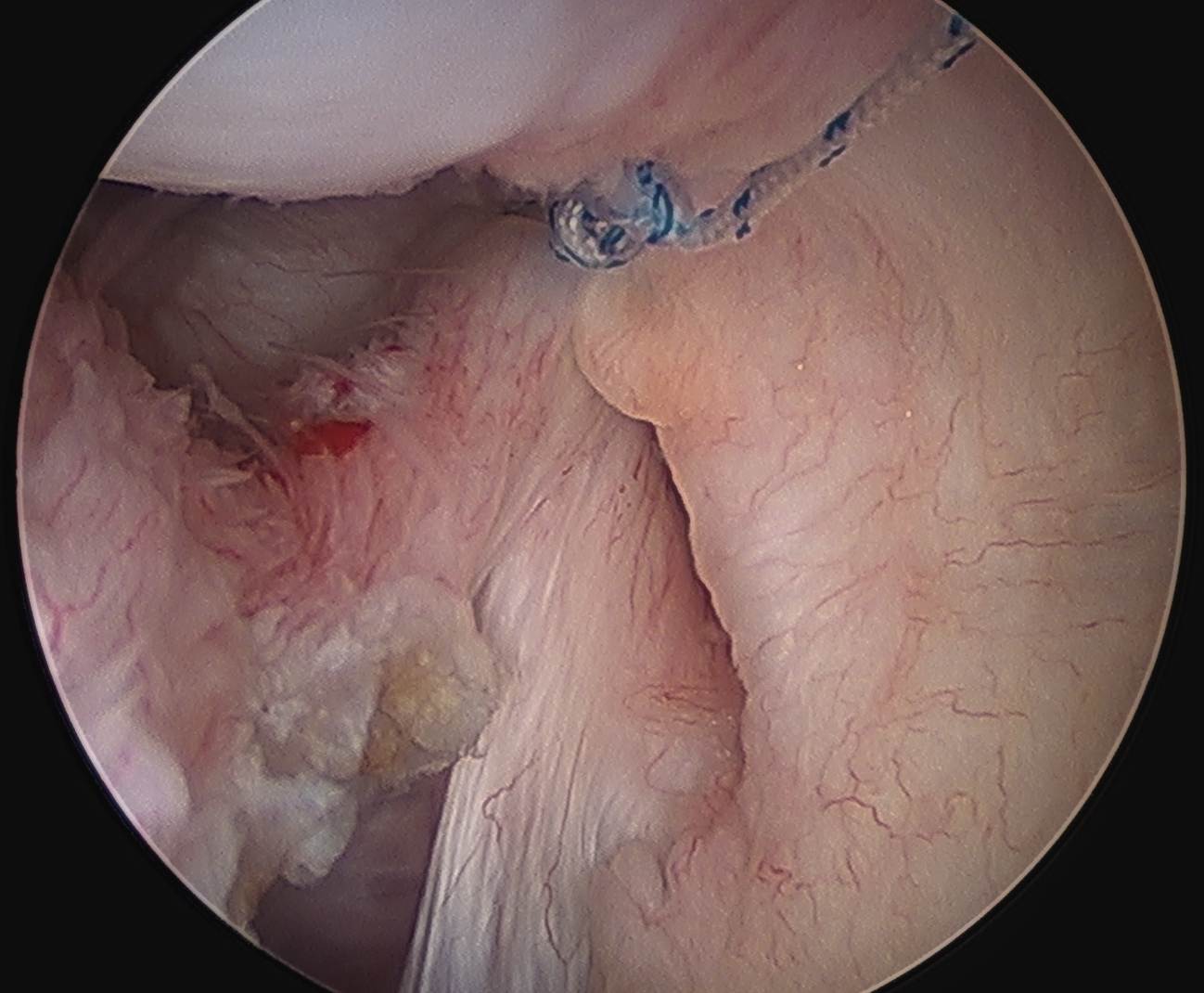
Remplissage
Theory
- described by Wolf Arthroscopy 2008
- advance IS into Hill Sachs lesion
- makes lesion extracapsular
Technique
- perform arthroscopic transtendinous advancement of IS and capsule into defect
- tie knots from subacromial space
Results
Zhu et al Am J Sports Med 2011
- 8.2% failure in 42 cases
Humeral head allograft


Technique
- anterior deltopectoral approach
- ER shoulder
- debride base of Hill Sachs
- secure allograft with 2 x screws
Issue
- late resorption of graft with recurrent instability
Humeral Head Osteotomy
Weber et al JBJS Am 1984
- series of 180 patients
- very low risk of recurrence
C. Abnormal Version
Glenoid or Head
- rarely a cause
