Epidemiology
Most common form of shoulder instability
- young males
- M:F = 2:1
Aetiology
Indirect ER and abduction moment on arm
- disruption of anterior stabilisers
History
Initial injury
- severe pain in shoulder
- ± transient paraesthesia / dead arm syndrome
History of dislocations
Examination
Very painful & tender shoulder
- significant muscle spasm
- arm held across abdomen
Hollow under acromion
- fullness in anterior shoulder
Axillary nerve palsy
- important to exclude
- look for parasthesis in badge area
- 20 years = 5% --> 90% recover
- 80 years = 90% --> 10% recover

Musculocutaneous Injury + Rotator Cuff Tear



Diagnostic Dilemma
Patient with history traumatic dislocation / wasting of shoulder / loss ROM
1. Wasting deltoid (AXN)
2. Wasting SS, not IS (RC tear)
3. Wasting SS & IS (SSN injury or massive tear)
4. Wasted deltoid + SS/IS (upper trunk brachial plexus or AXN palsy with RC tear)

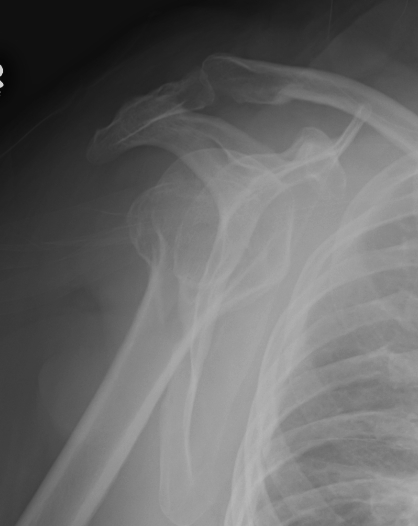
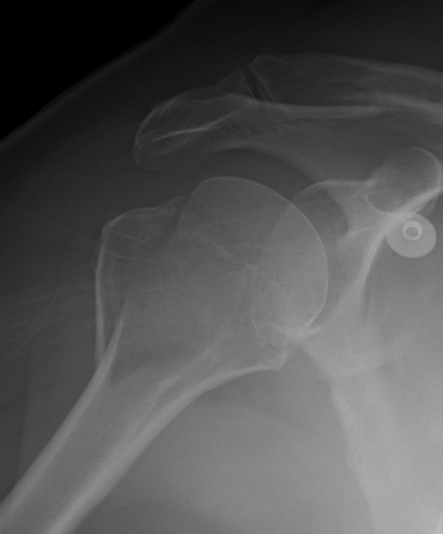
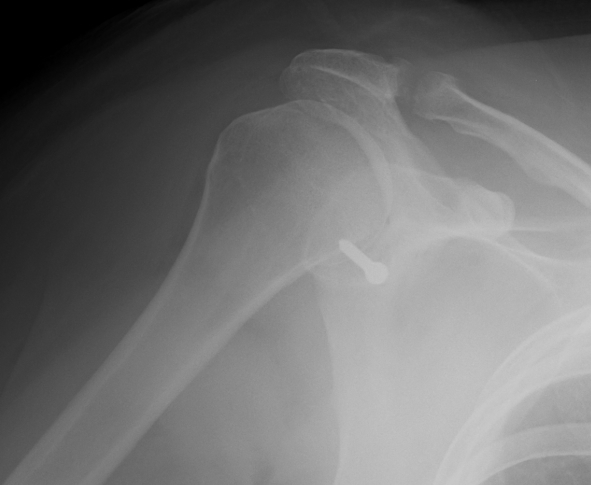
Xray
True AP
- dislocation
- fracture GT
- bony bankart
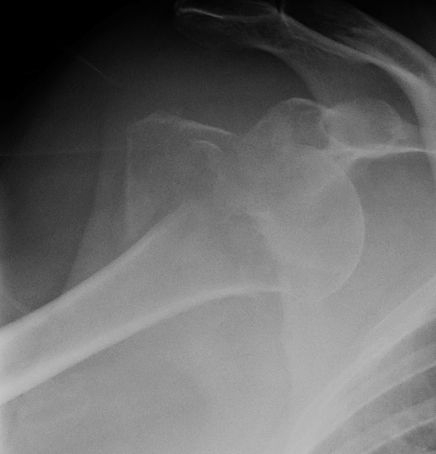

AP in IR
- Hill Sachs lesion
Scapular Lateral
- dislocation
- humeral head should be in centre of Y

Axillary Lateral
- dislocation
- Hill Sachs



Garth
- aim beam caudally
- bony bankart
Classification
According to direction seen on xrays
1. Subcoracoid / most common
2. Subglenoid
3. Intrathoracic
Management
Reduction
ASAP
- appropriate analgesia & muscle relaxation / conscious sedation
- atraumatic closed reduction performed
- if unsuccessful, may require GA
- rarely need open reduction
Post-reduction xray
- confirm reduction
- rule out associated fracture

Techniques
1. Stimpson
- patient prone
- arm hanging over side of bed
- weight applied to wrist
- give mild sedation
- not appropriate if obese / sleep apnea etc

2. Harvard / Traction & Countertraction method
- patient supine
- traction with abduction
- countertraction via sheet around axilla
- similar to Hippocratic but no foot in the axilla
3. Kocher
- externally rotate and maximally abduct arm
- relocate via adduction
- nil IR til located to avoid humeral fracture
4. Hippocrates
- foot in arm pit
- apply longitudinal traction
Immobilisation
No effect on re-dislocation rate
- no sport for 6/52 reduces dislocation rate
Protocol
- sling for comfort
- avoid provocation 6/52
- no sport until painless FROM
ER brace
Theoretical
- tightens SSC
- reduces bankart lesion into anatomical location whilst healing
- may reduce redislocation rates
- problems with compliance as is uncomfortable and in young population
Itoi et al JBJS Am 2007
- RCT ER brace v sling 198 patients 3 weeks duration
- relative risk reduction 38%
- 26% recurrence v 42% (p < 0.03)
- particularly beneficial if < 30
Finestone et al JBJS Br 2009
- RCT 51 patients
- no difference
Rehabilitation
Start with ROM exercises
- pendulum / active Assisted / active
Progress to shoulder strengthening
Prognosis
1. Age at first dislocation
Increased in young
- the majority of recurrences occur within 2 years of the first traumatic dislocation
Classic paper Rowe CORR '61
- < 20 90% redislocation
- 20-30 60% redislocation
- 30-40 30% redislocation
- > 40 10% redislocation
McLaughlin and MacLellan 1967
- 95% traumatic dislocations in teenagers recurred
Simonet and Cofield 1982
- overall incidence of recurrence 33% over 4 years
- 66% in patients < 20 years
- 17% in patients 20 - 40 years
2. Trauma of First Dislocation
Decreased incidence of re-dislocation with
- severe trauma
- associated fracture (usually LT / GT)
3. Activity
Re-dislocation more common in athletes
- 80% in athletes
- 30% in non-athletes
4. Rehabilitation
Activity restriction & effective muscle strengthening reduces re-dislocation
- overall re-dislocation rate 25% at 3 years in Army
- need strict adherence with program
Indications Operative Management in Acute Dislocation
1. Rotator cuff tear
2. Displaced GT fracture
3. Large glenoid rim fracture
4. ? Athlete
Rotator cuff tear
Diagnosis
Important not to miss
- high incidence in patients > 40
- suspect if pain or decreased ROM
- MRI
Incidence
Berbig et al J Should Elbow Surg 1999
- prospect ultrasound on 167 patients with dislocation
- full thickness tears in 31.7%
- only acute tears in patients younger than 60
- control group had no FT tears in patients younger than 60
Management Options
A. Repair RC / leave Bankart
B. Repair RC and Bankart
Voos et al Am J Sports Med 2007
- retrospective review of arthroscopic repair of RC and labrum
- average age 47, 16 patients
- good or excellent results in > 90%
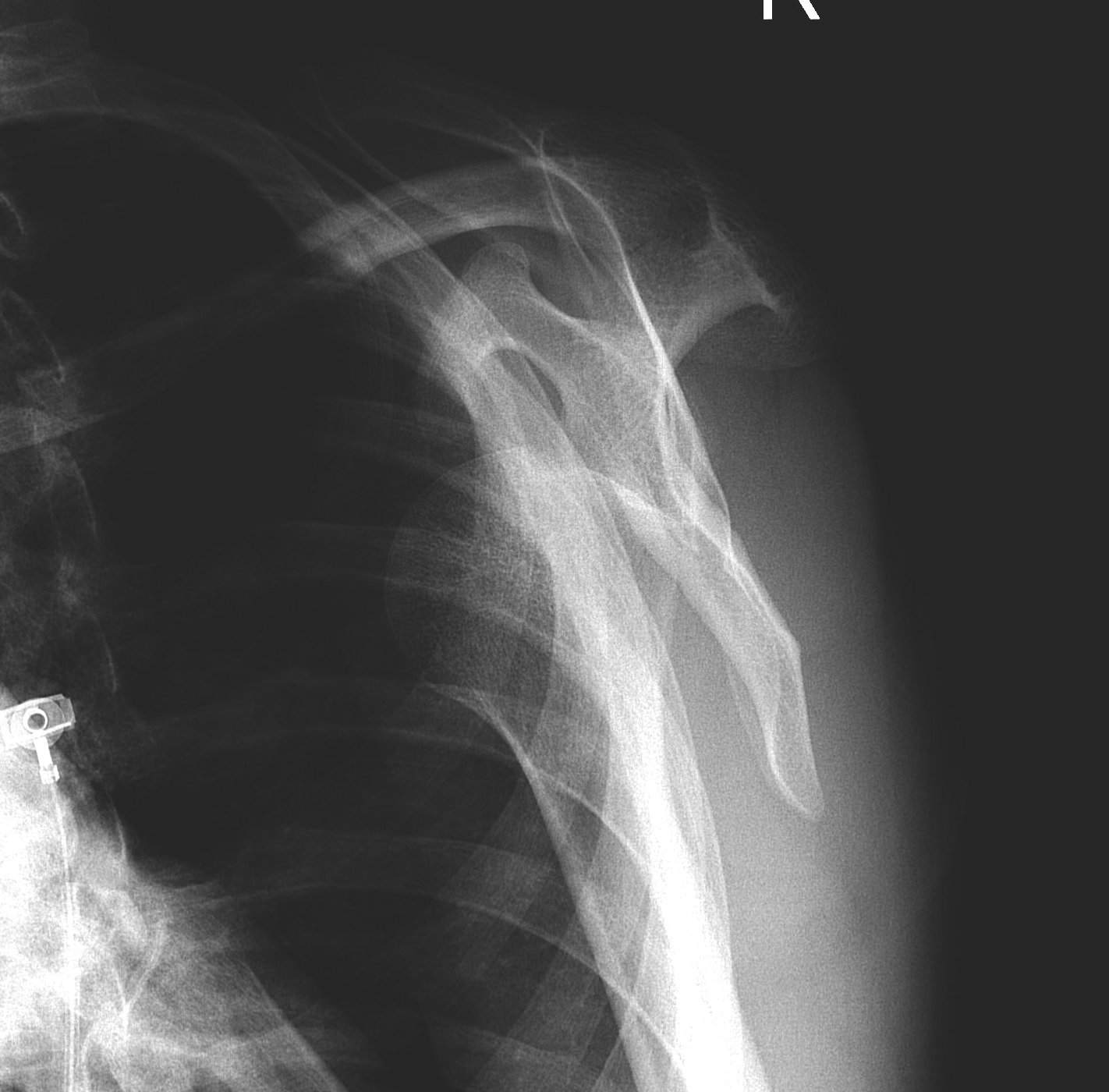
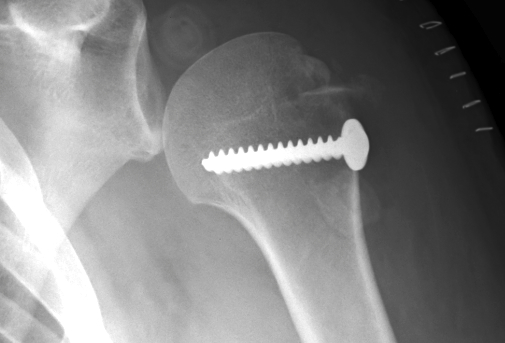
2. Displaced GT Fracture
Indications
- > 5 mm displacement
Management
- ORIF
- screw + suture repair
- screw alone in young patient
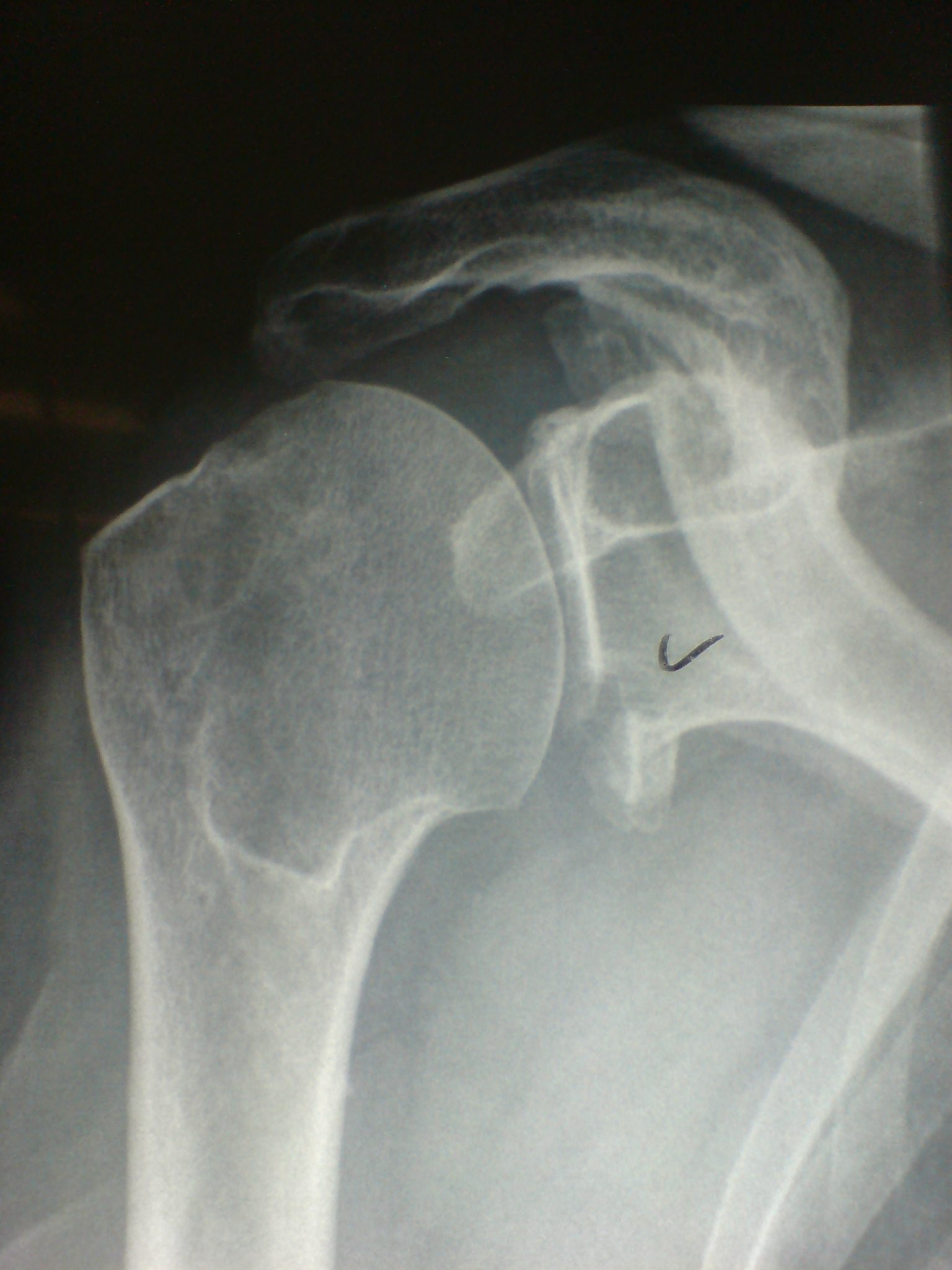
3. Large Glenoid Rim Fracture
Indications
- > 25 - 30% and displaced
Management
- open or arthroscopic
- fix with 1 or 2 cannulated screws


4. Acute dislocation in professional athlete
Robinson et al JBJS Am 2008
- prospective randomised control trial arthroscopic surgery in first time dislocators
- 88 patients under 35, arthroscopic stabilisation v arthroscopic lavage
- reduced risk of recurrence by 80%
- patient satisfaction and shoulder scores significantly improved
Kirkley et al Arthroscopy 2005
- RCT of 40 patients for arthroscopic stabilisation v immobilisation
- 3 recurrences in surgical group, 9 in non surgical group
- small improvement in shoulder scores in operative group
Jakobsen et al Arthroscopy 2007
- RCT 76 patients
- arthroscopy to diagnose labral injury
- either open repair or non operative
- 74% unsatisfactory results at 8 years in non operative group
- 75% good results in operative group (1 redislocation)
