Definition
Malignant mesenchymal cells producing osteoid
Epidemiology
Most common malignant primary bone tumour excluding myeloma
Bimodal peak
1. Second decade / teenagers - 75%
2. Elderly / 7th decade - Paget's
Male:Female 3:2
Etiology
Li-Fraumeni syndrome
Retinoblastoma - FHx / p53 Defect
Secondary
- Paget's / Radiotherapy / Osteomyelitis / Fibrous Dysplasia
- Chondrosarcomatous dedifferentiation
World Health Organization Classification 2020
Osteosarcoma, not otherwise specified (NOS)
i) Conventional (80%)
- high grade, intramedullary
- osteoblastic / chondroblastic / fibroblastic cell types
- all three types produce osteoid
ii) Telangiectatic (4%)
- blood filled cavities with high grade sarcomatous cells
- can be mistaken for ABC's
iii) Small Cell (1-2%)
- similar to Ewing's
- differentiated by osteoid production
Low Grade Central Osteosarcoma (LGCOS)
- 1-2%
- affects 3rd - 4th decade
- better prognosis
Surface
i) Parosteal (4-6%)
- low grade OS arising from periosteum
- typically posterior distal femur
ii) Periosteal
- less common
- forms as a periosteal reaction
iii) High grade surface
- behaves similar to conventional
Conventional Osteosarcoma
History
Pain
- often activity related likely due to microfracture
- most patients relate onset of pain to some minor trauma
- sometimes at night
No systemic symptoms
Xray
Typically metaphysis of long bones
- distal femur 35%
- proximal tibia 20%
- proximal humerus 10%
Can be diaphysis / axial skeleton
Features
- new bone formation / osteoid
- permeative cortical destruction
- wide zone of transition
- periosteal reaction
- soft tissue mass




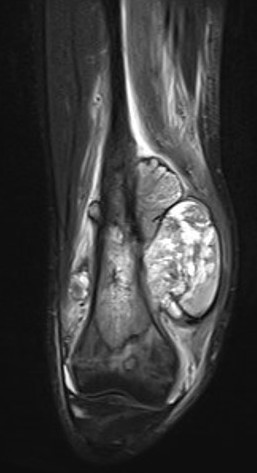
Osteosarcoma of the distal femur



Osteosarcomas of the proximal tibia


Osteosarcoma of the humerus Osteosarcoma of the fibula
Codman's Triangle
- triangular periosteal new bone formation
- at proximal and distal cortical margins
- reaction to rapid growth


Codman's triangle in osteosarcoma distal femur
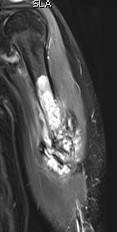
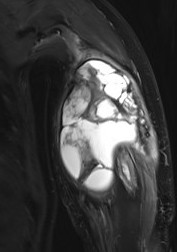
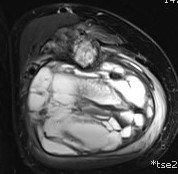
MRI

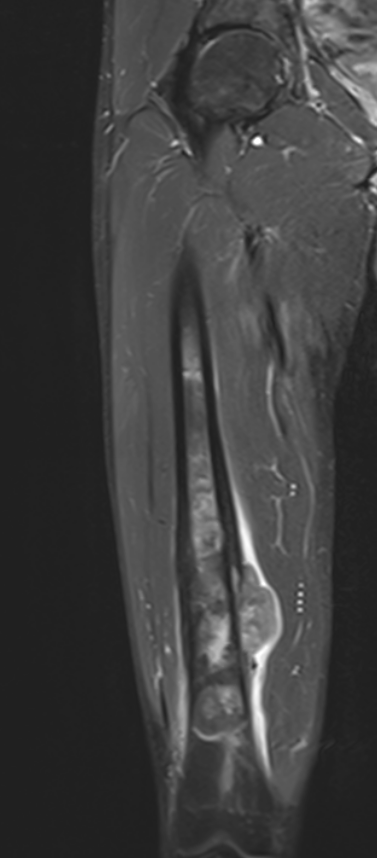
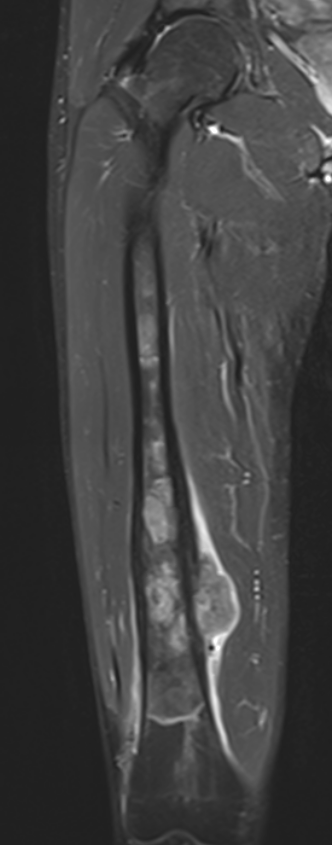
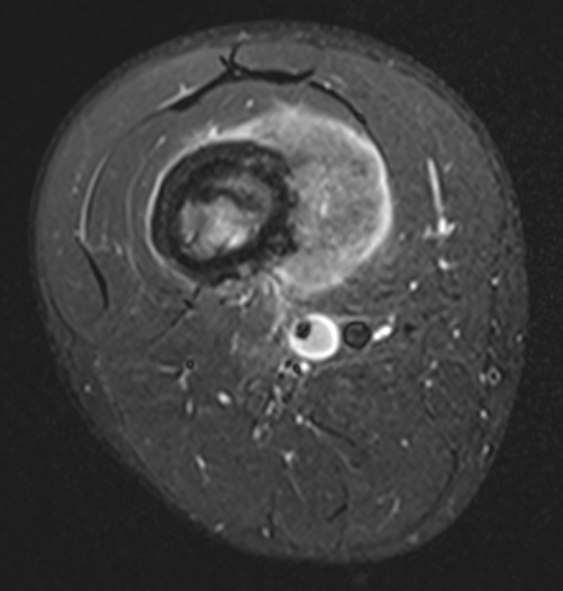
Evaluate
i) Soft tissue component
ii) Involvement of neurovascular bundle
iii) Marrow extent of tumour
- helpful in determining appropriate resection level
- satellite lesions - metastasis within reactive zone
iv) Identify skip lesions
- metastasis outside reactive zone
- sagittal and coronal images of the entire bone
v) Joint involvement


CT
Complementary to MRI / very useful in the pelvis
Bone Scan
1. Identify margins for resection / identify skip lesions
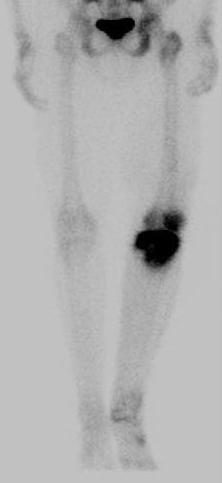

2. Identify metastatic disease
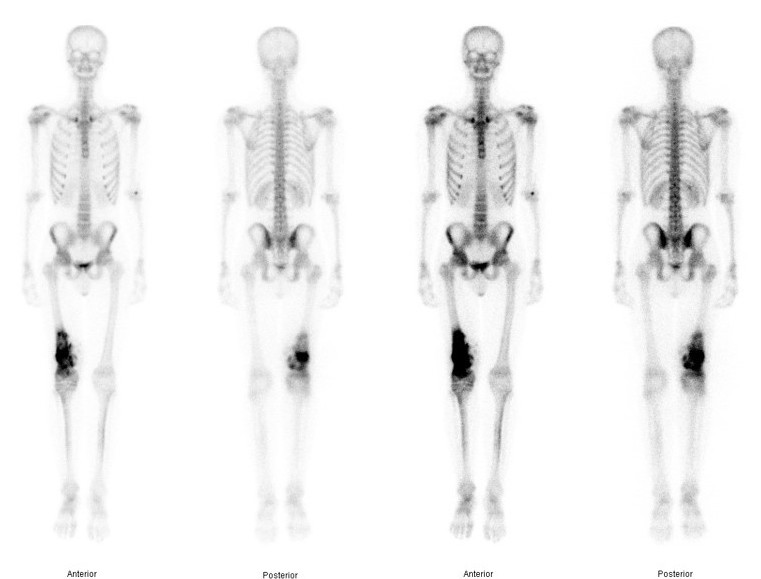
Bone scan with isolated disease
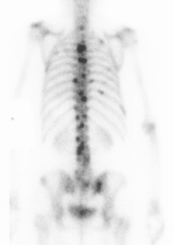

Bone scan metastasis
CT Chest / abdomen
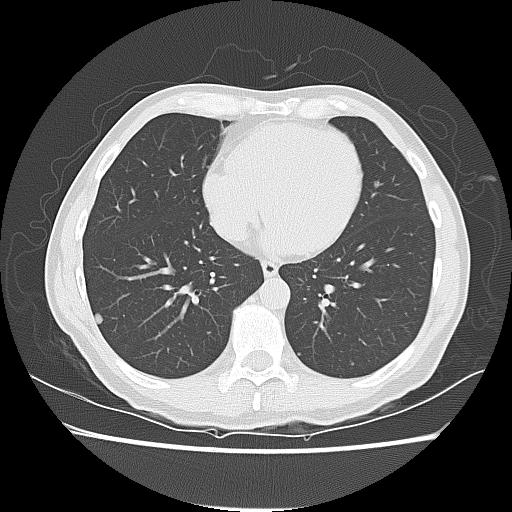
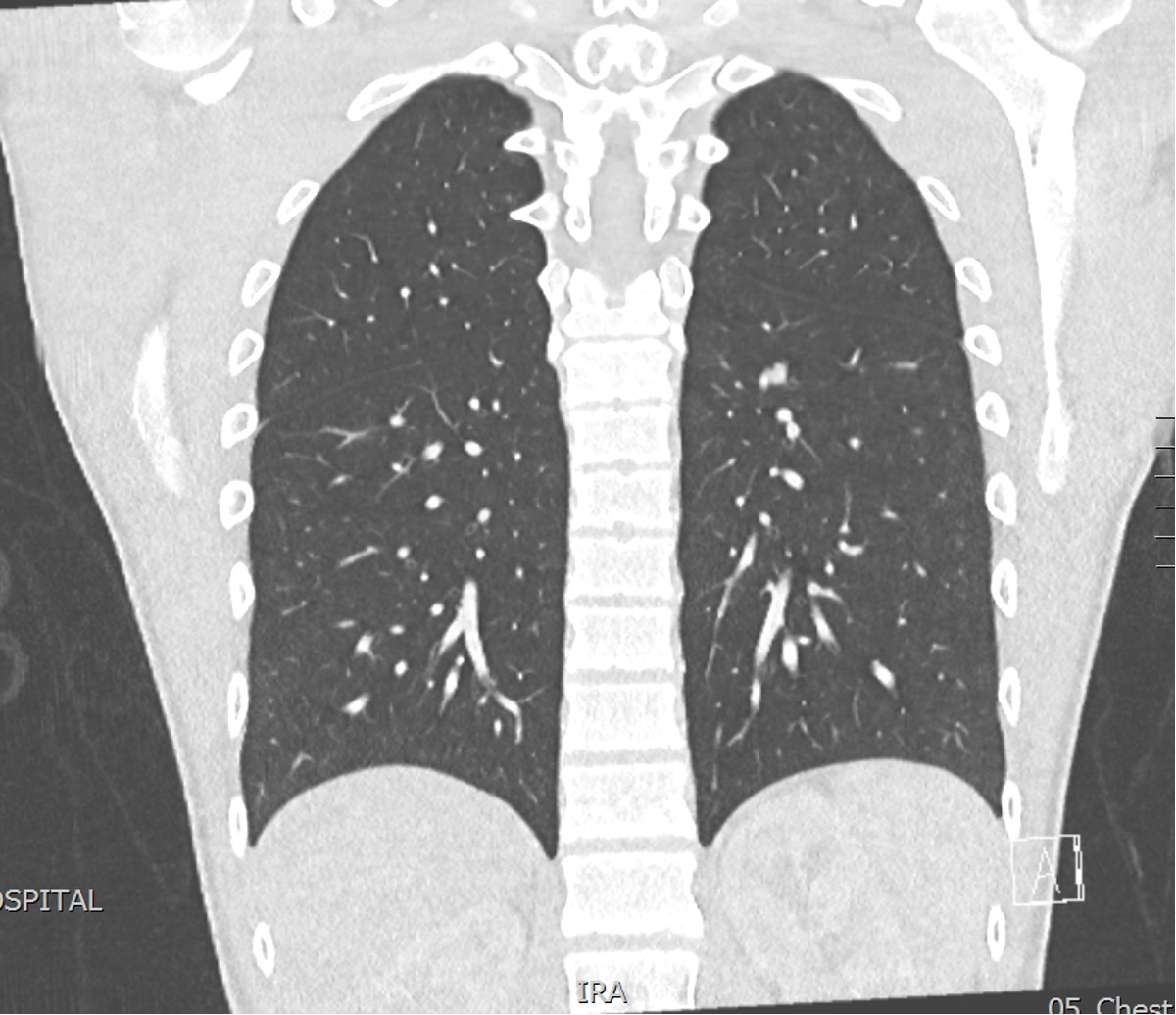
Pulmonary metastasis
Biopsy
Options
- incisional biopsy
- image guided fine needle aspirate
- image guided core needle biopsy
Results
Dirks et al World J Surg Oncol 2023
- incisional biopsy of 332 malignant musculoskeletal tumours
- sensitivity 100%, specificity 97.6%
Tsukushi et al Arch Orthop Trauma Surg 2010
- CT guided needle biopsy in 207 patients with musculoskeletal lesions
- diagnostic accuracy 90%
- systematic review of 21 articles
- accuracy incisional biopsy > core needle > fine needle
- increased risk of contamination with incisional biopsy
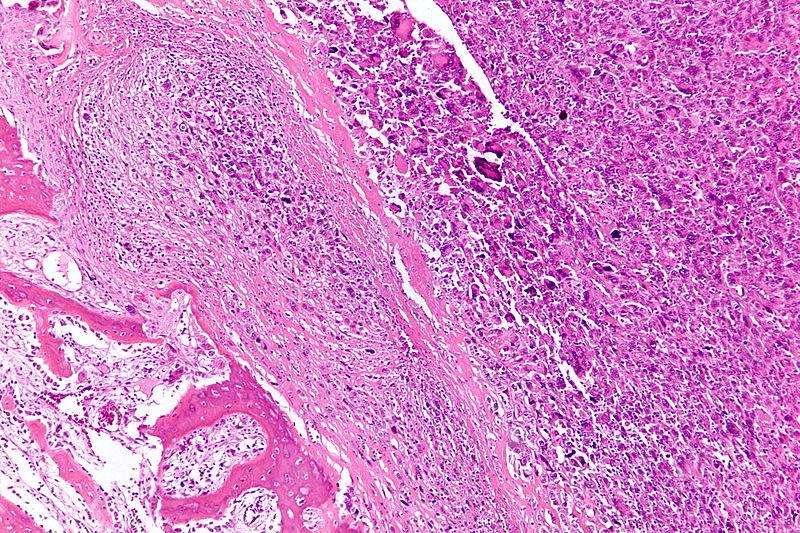
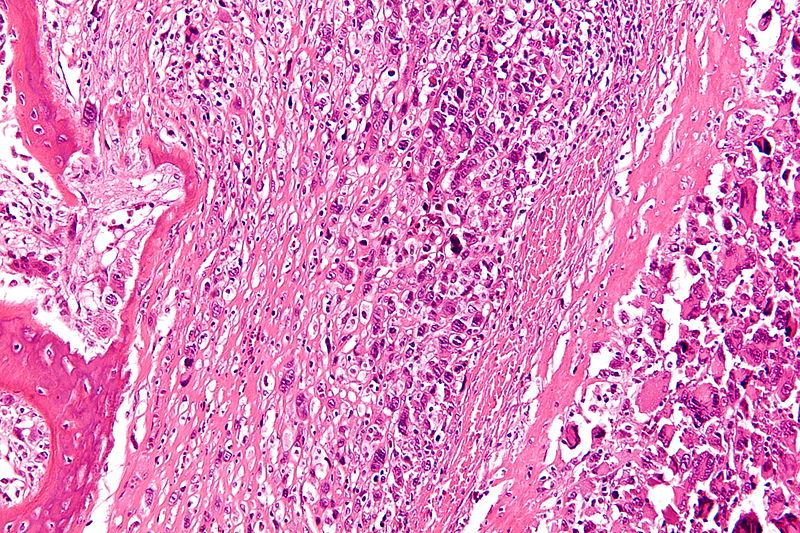
Histology
Must see malignant spindle cell stroma producing osteoid
Pleomorphic spindle cells
- hyperchromatic nuclei
- atypical mitotic figures
Osteoid
- can be difficult to find
- adequate sampling essential
Staging
Enneking / Musculosketal tumour society
Stage I: Low grade
Stage II: High grade
Stage III: Metastasis
A: intra-compartmental
B: Extra-compartmental
Most osteosarcomas are stage IIB
Management
Algorithm
1. Accurate clinical staging
- local (cross sectional imaging - CT / MRI)
- systemic (bone scan & CT chest / abdomen)
- biopsy
2. Neoadjuvant chemotherapy
3. Restage
- locally and systemic (MRI / CT Chest)
4. Wide resection
5. Post operative chemotherapy +/- radiotherapy if positive margins
Prognosis
Single most predictive factor is the presence or absence of detectable metastasis at presentation
Factors
Age
Localised disease
Response to chemotherapy
Pathological fracture
O'Kane et al Clin Sarcoma Res 2015
- 81 patients with localized disease
- overall survival 70% 7 years
- patients <40 74% 5 year survival
- patients <40 42% 5 year suvival
Chemotherapy
Preoperative chemotherapy
Four chemotherapy agents
- methotrexate with leucovorin rescue, doxorubicin (AKA adriamycin), cisplatin, and ifosfamide.
Rosen in vivo response dictates outcome
Grade 1: No cell death
Grade 2: Partial <90%
Grade 3: Necrosis >90%
Grade 4: Complete necrosis
O'Kane et al Clin Sarcoma Res 2015
- 81 patients with localized disease
- overall survival 70% 7 years
- >90% necrosis, survival 82% 5 year
- < 90% necrosis, survival 68% 5 year
- 232 patient < 40 years with localized disease
- treated with MAP (methotrexate, adriamycin, cisplatin)
- overall survival 74% 5 years
- chemotherapy induced necrosis associated with survival
- 72% necrosis cut off for optimal 5 year survival in this study
Postoperative chemotherapy
- 703 patients with osteosarcoma
- investigated timing of resumption of chemotherapy post surgery and survival
- overall survival poorer for those with chemotherapy commenced > 21 days post surgery
Surgery
Options
Amputatation
Limb Salvage Surgery
Mei et al Arch Orthop Trauma Surg 2014
- meta-analysis of 6 studies comparing limb salvage to amputation for osteosarcoma
- similar functional outcomes and quality of life in both groups
Timing
Usually 2 weeks after end neoadjuvant chemotherapy
Goal
Bony resection with wide margins
- 5 - 7 cm
Limb Salvage Surgery
80% patients can have limb salvage
Contraindications / PIN LEG
1. Pathological fracture
2. Infection
3. Neurovascular involvement
4. Immature skeletal age if LLD >6-8cm
5. Extensive muscle involvement
6. Poor biopsy (instead of well performed biopsy)
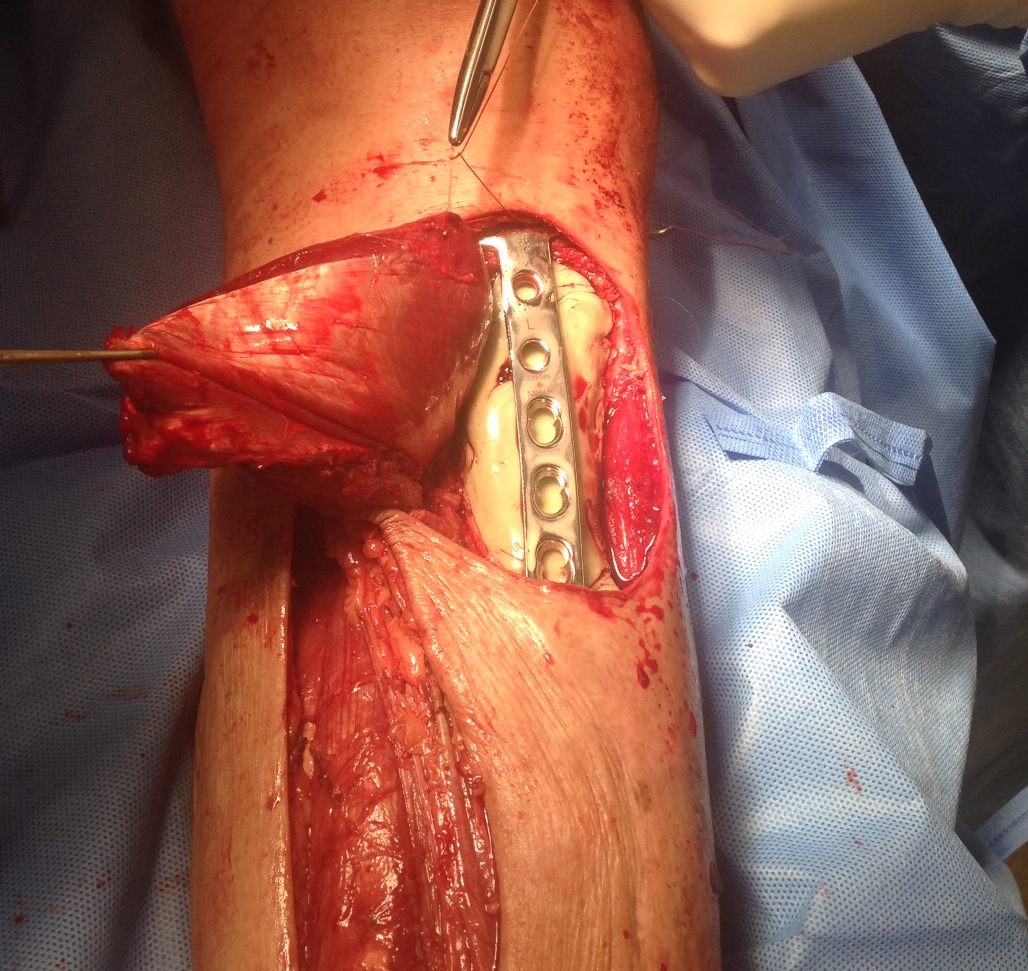
Technique
Vumedi resection distal femur osteosarcoma and insertion megaprosthesis
Vumedi resection proximal tibia osteosarcoma and insertion megaprosthesis
1. Resection of tumor and biopsy tract
2. Skeletal reconstruction
3. Soft tissue cover
Resection of tumor & biopsy tract
Major neurovascular bundle must be free of tumor
- wide resection of affected bone
- normal muscle cuff in all planes
- biopsy tract removed en bloc
- adjacent joint and capsule should be resected
- extra-articular resection preferred
- articular resection mandatory if effusion present
- use tourniquet --> if site contaminated at histology allows amputation to be performed above tourniquet level
Skeletal reconstruction
Options for 15 - 20 cm defect
- megaprothesis
- massive allografts
Megaprosthesis
Modular, silver coated titanium megaprosthesis
Design
Gosheger et al J Arthroplasty 2008
- 197 patients treated with megaprosthesis
- infection rate cobalt chrome 31%
- infection rate titanium 14%
Fiore et al Eur J Orthop Traumatol 2021
- meta-analysis of 19 studies using megaprosthesis
- infection rate with silver coating 9% versus 11% without
- infection rate with revisions with silver coating 14% versus 29% without


Post distal femoral osteosarcoma resection

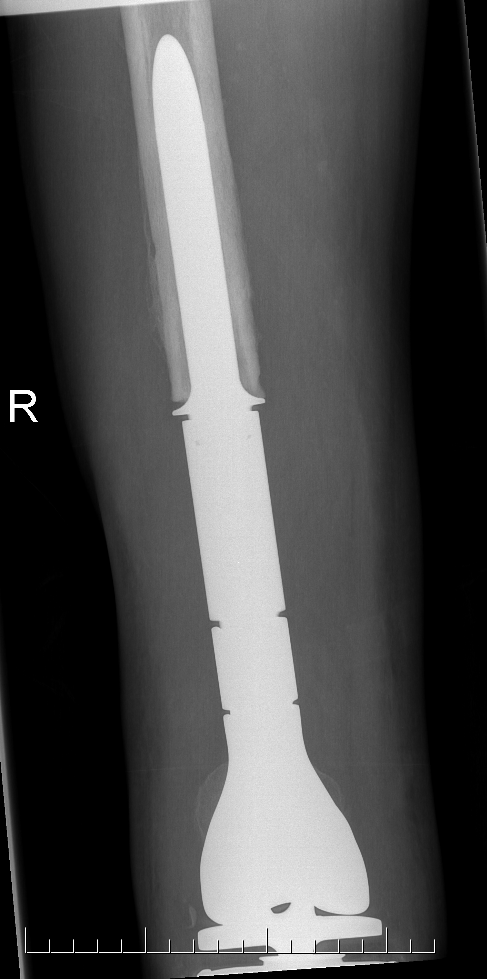
Post distal femoral osteosarcoma resection


Post proximal tibial osteosarcoma resection


Results
- cemented megaprosthesis for high grade osteosarcoma around the knee
- 108 patients with average age 25
- 5 year prosthesis survival 78%
- 8 year prosthesis survival 55%
Sadek et al Ann Surg Oncol 2023
- modular endoprosthesis for osteosarcoma of the distal femur
- 82 patients
- 5 year prosthesis survival 68%
- 10 year prosthesis survival 52%
- aseptic loosening commonest complication 19.5%
- deep infection 15.9%
Ebeid et al Ann Surg Oncol 2023
- modular endoprosthesis for osteosarcoma of the proximal tibia
- 55 patients
- 5 year prosthesis survival 82%
- 10 year prosthesis survival 62%
- aseptic loosening commonest complication 14.5%
- deep infection 14.5%
- periprosthetic fractures 16%


Megaprosthesis aseptic loosening
Massive osteochondral allografts
- 20 year follow up of 26 patients treated with massive osteochondral allograft
- 53% graft failure
- recommended against their use
Local soft tissue and muscle transfers

Pathological fracture and osteosarcoma


Summary
Poorer prognosis likely related to higher incidence distant disease
Limb salvage not precluded
Adults have poorer prognosis than pediatric population
Results
Salunke et al Bone Joint J 2014
- systematic review and meta-analysis
- pathological fracture 303/1713 (18%)
- local recurrence with fracture 14% versus without fracture 11%
- five year survival with fracture 49% versus without fracture 67%
- no difference between amputation and limb salvage
Zhong et al Am J Transl Research
- systematic review
- pathological fracture associated with poorer prognosis
- likely related to increased association of distant metastasis
- no significant difference between amputation and limb salvage
Kelley et al J Clin Oncol 2020
- cohort of 2,200 patients with OS
- incidence pathological fracture 11%
- no difference in overall survival in pediatric population
- 5 year survival adults with fracture 46% versus without 69%
Metastasis
Mettman et al, Cancer Med 2023
- Retrospective RV of 219 osteosarcoma patients who relapsed with a single pulmonary nodule
- 94.9% achieved successful resection of nodule
- 5y survival post complete resection was 51%, compared to 0% if incomplete
- resection technique (thoracotomy vs thoroscopy), chemo, radiation made no difference