Epidemiology
< 1% of all fractures
Etiology
Fall from height
Dorsiflexion injury - neck of talus strikes the anterior tibia
Supination injury - neck of talus strikes medial malleolus
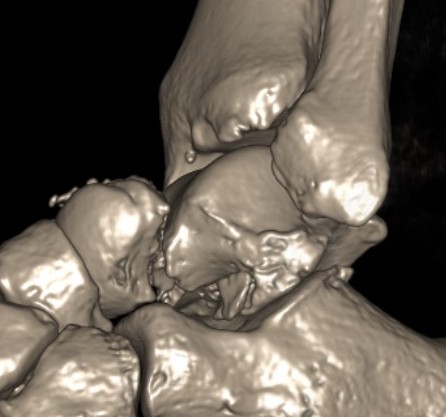
Anatomy
No muscular attachments
60% covered by articular cartilage
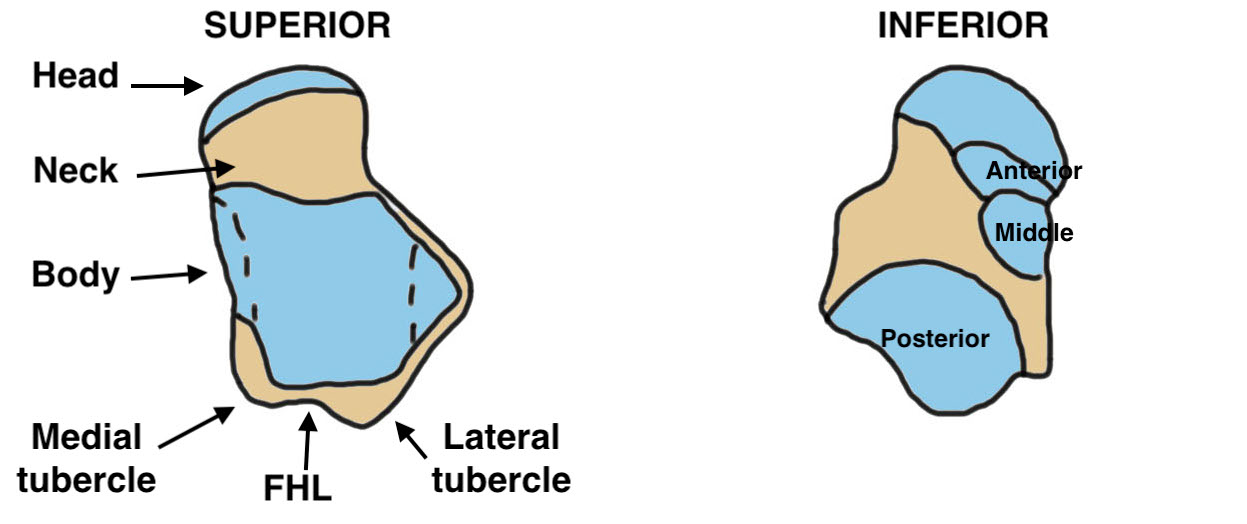
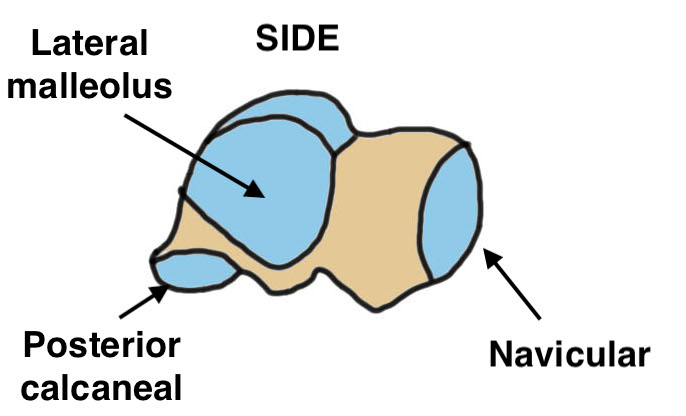
| Body | Neck | Head | Inferior facets |
|---|---|---|---|
|
Superior cartilage for tibia |
Angles medially 10 - 44 Angles plantar 5 - 50 |
Articulates with navicular
|
Posterior / middle / anterior |
| Articulate with medial & lateral malleolus | Conduit for blood supply to body | Supported by spring ligament | Articulate with calcaneal facets below |
Blood Supply
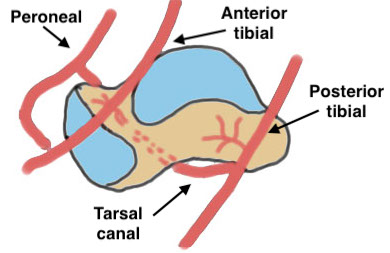
| Posterior tibial artery | Anterior tibial artery | Peroneal artery |
|---|---|---|
| A. Artery of tarsal canal - body | Dorsalis pedis | Artery of sinus tarsi |
| B. Deltoid branch - medial body | Head and neck of talus | Head and neck of talus |
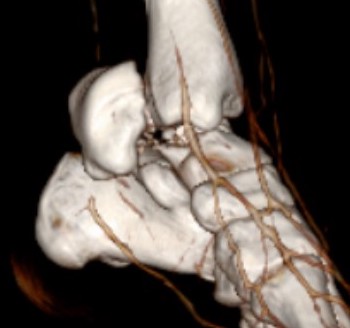
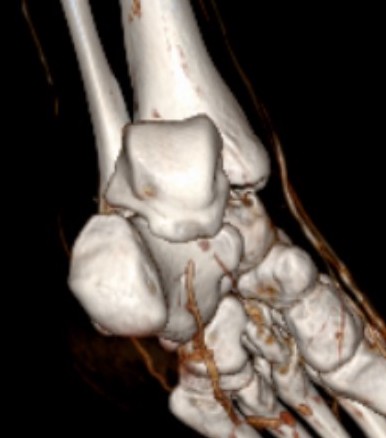
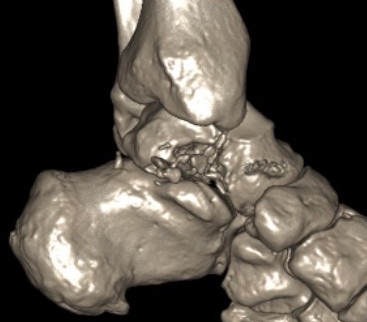
Hawkins classification
Progressive injury
| Type I | Type II | Type III | Type IV | |
|---|---|---|---|---|
| Definition |
Fracture of neck Undisplaced |
Fracture displaces Subluxation / dislocation of the subtalar joint |
Talar body dislocates from ankle joint posteromedially | Talar head dislocates from navicular joint |
| Incidence | 21% | 43% | 31% | 5% |
Type I: Minimally displaced

Type II: Disruption of subtalar joint

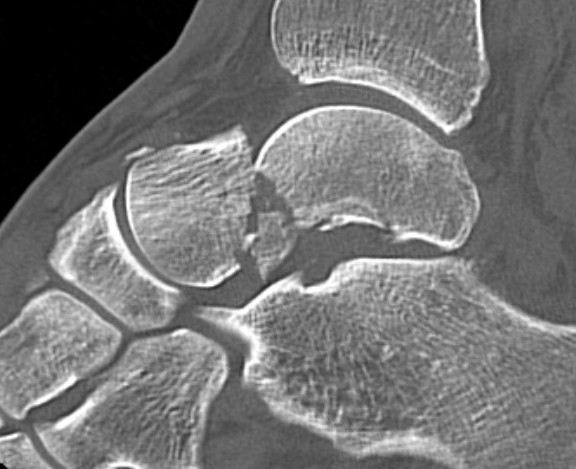
Type IIa: subtalar joint subluxed

Type IIb: subtalar joint dislocated
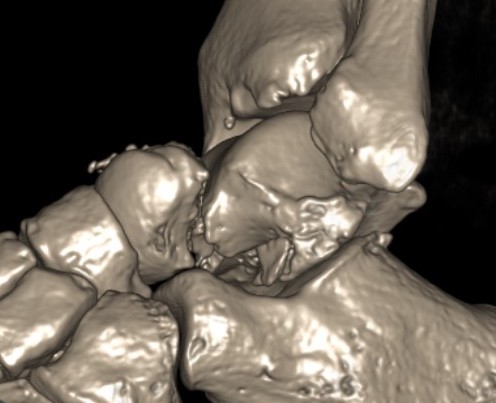
Type III: Talar body dislocated from ankle joint



Type IV: Talar head dislocated from talonavicular joint


Immediate management
Reduce fractures



Closed reduction technique
- flex knee to relax gastrocnemius
- traction on plantarflexed foot to realign head and body
- varus / valgus correct as required
Irreducible fractures / Extruded Talus
Options
- anteromedial / anterolateral approach
- posteromedial approach


Posteromedial approach for open reduction of dislocated talar body
Non-operative Management
Indication
Type I
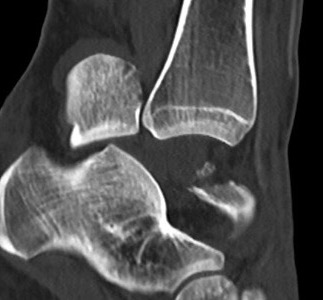
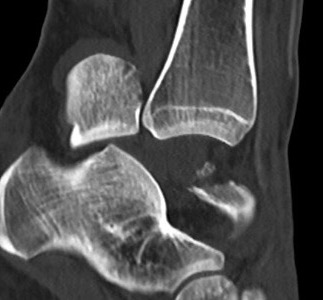
Xray / CT
Ensure no displacement / malalignment
Managment
6 - 8 weeks in cast NWB
Operative Management
Timing of Surgery
Does early reduction prevent AVN?
- 102 patients with ORIF talar neck fractures
- no evidence that surgical delay increased AVN
- AVN associated with neck comminution and open fractures
- recommendation to wait for swelling to subside
Best to delay to allow soft tissues to settle
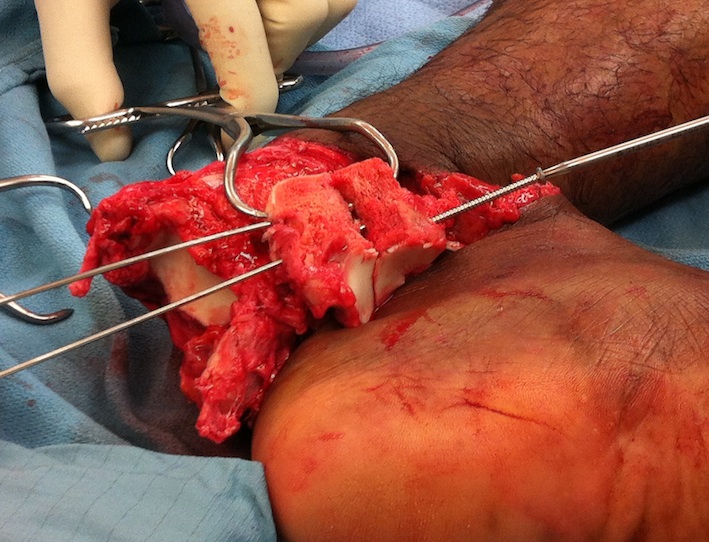
Approach
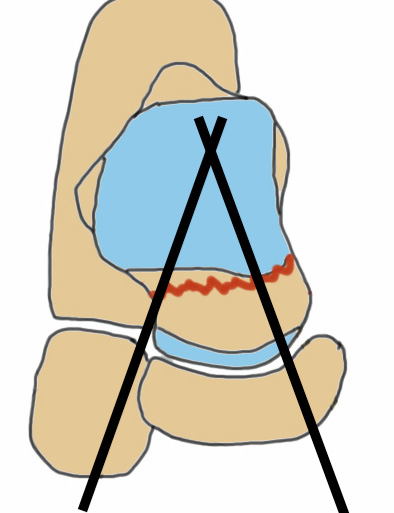
2 incision technique with > 7 cm skin bridge
1. Anteromedial approach
Technique
- from medial malleolus to talonavicular joint / base first metatarsal
- protect great saphenous vein and saphenous nerve
- between Tibialis anterior and tibialis posterior tendon
- preserve deep deltoid for blood supply
- +/- medial malleolar osteotomy to access talar dome
AO surgery reference anteromedial approach talus
2. Anterolateral approach
Technique
- based on 4th metatarsal
- anterolateral border fibular to 4th metatarsal
- protect branches superficial peroneal nerve
- mobilize extensor tendons medially
- divide and elevate EDB, retract laterally
- excise sinus tarsi fat pad
- 7 cm skin bridge from anteromedial approach
AO surgery reference anterolateral approach talus
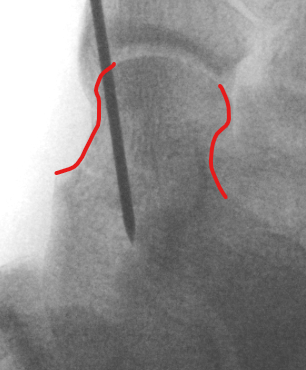
Anatomical reduction + fixation
1. Remove loose bodies from subtalar joint

2. Reduction - avoid varus and shortening medial neck
- often medial comminution
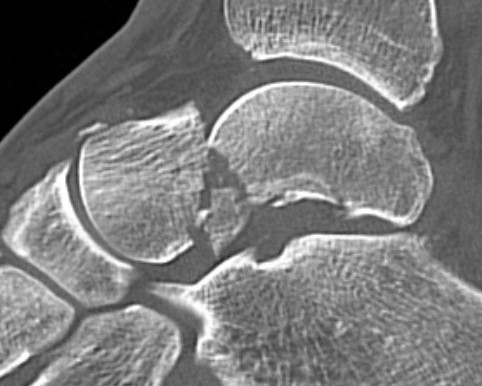
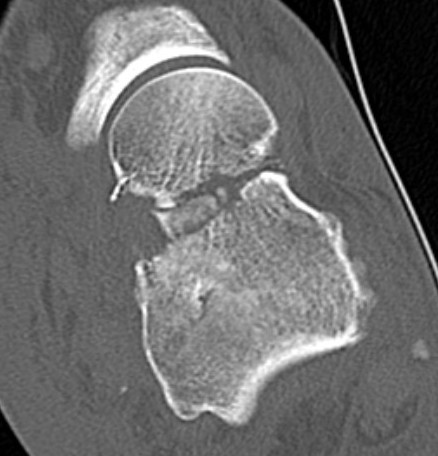
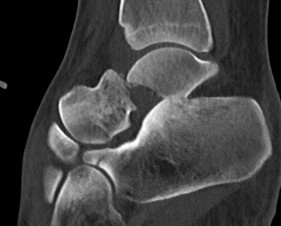
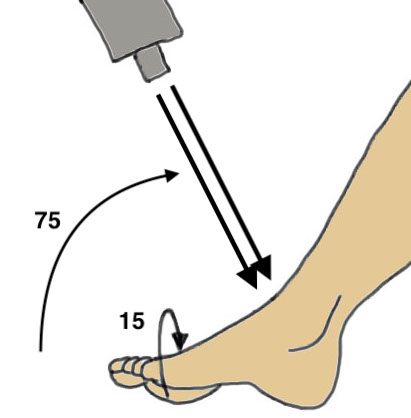
Canale view
- evaluates talar neck
-
- beam angled
- look for medial shortening / varus
ORIF
AO surgery foundation talar neck ORIF
Vumedi dual approach to talus video
Vumedi talar neck fixation techniques video
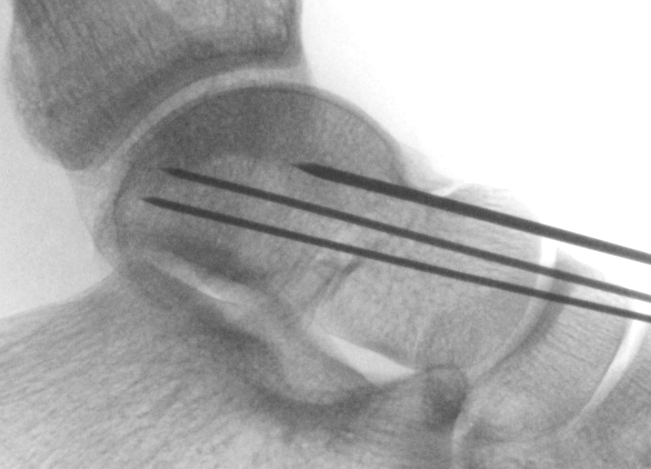
Cannulated screws
Xrays
| AP | Lateral | Canale View |
|---|---|---|
| Entry point of the screws |
Evaluate neck reduction
|
Evaluates the neck reduction |
|
Lateral off articular surface Medial through articular cartilage |
Depth of screws |
Beam angled 75o to foot Foot 15o pronated |
 |
 |
 |
 |
 |
  |
1. Retrograde (anterior to posterior) into posterior talus body
A. Lateral screw
- insert proximal to articular surface of head on lateral side
- bone is very curved here
- can lag screw as usually no comminution
B. Medial side
- insert through articular surface
- countersunk screws through articular surface
- avoid lag screw techniques medially as may compress comminution into varus

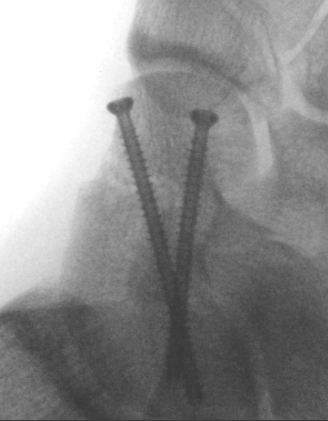
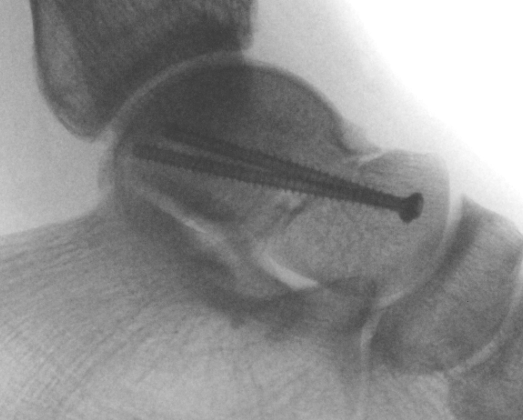
AP, Canale and Lateral xray



Retrograde screws
2. Antegrade (posterior to anterior) screws
- between FHL and peroneals
- entry point lateral tubercle talus
- bury to avoid posterior impingement


Antegrade screws
Plates
Options
- mini fragment plates
- anatomically contoured talar neck plates
- lateral talar neck very curved

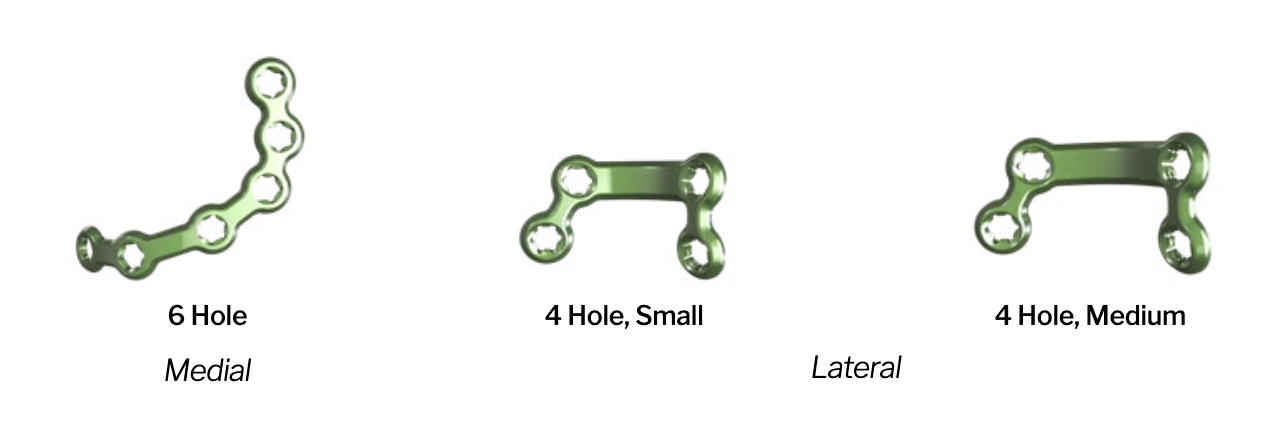
Paragon 28 talar neck plates pdf


Screw + plate
Devitalised Type 3 / 4 with compound wound
Option 1. Wash / lean / ORIF / reduce





Option 2: Discard / cement spacer / later fusion or total talar replacement