

Complications
Infection
Nonunion
Malunion
Osteoarthritis
Avascular necrosis
Infection
Halvorsen et al J Foot Ankle Surg 2013
- systematic review
- overall incidence 21%
- increased with open fractures
Nonunion

Incidence
Alley et al J Orthop Trauma 2024
- 800 talar neck fractures
- 9% nonunion
Management
No collapse, AVN, or OA - bone graft +/- revision ORIF
Collapse, AVN or OA - arthrodesis +/- arthroplasty
Results
- 8 patients with talar neck nonunion
- ORIF + bone graft
- 5 patients also underwent subtalar fusion
- 7/8 united
- 1/8 progressive collapse - pantalar fusion
Mal-union
Varus malunion
Shortening of medial neck with varus secondary to medial comminution
Cavo-varus foot
- creates cavus foot with supination
- walk on lateral border of foot
- predispose to premature osteoarthritis
Options
No collapse or OA - medial opening wedge talus osteotomy
Collapse or OA - arthrodesis / arthroplasty
Results
- 7 patients with varus malunion
- talus medial opening wedge osteotomy for malunion technique
- one osteotomy nonunion treated with fusion
Osteoarthritis
Incidence
Most common complication
Jordan et al J Foot Ankle Surg 2017
- systematic review of incidence of subtalar OA
- Type I: 0%
- Type II: 54%
- Type III: 46%
- Type IV: 45%
Management
Subtalar fusion +/- pan talar fusion depending on location of OA
Avascular necrosis
Incidence
Jordan et al J Foot Ankle Surg 2017
- systematic review of incidence of AVN
- Type I: 0%
- Type II: 16%
- Type III: 39%
- Type IV: 55%
Risk factors
Alley et al J Orthop Trauma 2024
- 800 talar neck fractures
- increased risk of AVN with increasing severity of fracture / smoking / age / BMI / dual approaches
Hawkin's sign
Subchondral lucency under medial talar dome on xray
- appears 6 - 12 weeks post injury
- indicates vascularity
- presence excludes AVN
Natural history
Some AVN will revascularize without collapse over 2 years
Many patients asymptomatic
Xray





CT


MRI

AVN without collapse
Options
Non weight bearing - unclear if affects outcome
Shock wave therapy
Bisphosphonates
AVN with collapse and OA
Issue
Necrotic talus with collapse and bone loss
- fusion difficult
- total ankle replacement likely contra-indicated due to poor talus bone stock
Options
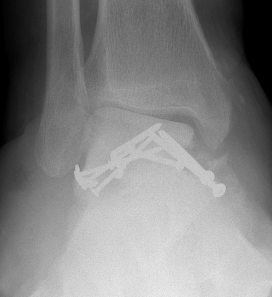
Arthrodesis
- Blair fusion - sliding tibial bone graft and tibio-talar fusion
- tibio-talar-calcaneal (pantalar) fusion with hindfoot nail
- talar excision + tibio-calcaneal fusion with Ilizarov frame and tibial lengthening
Arthroplasty
- partial talus replacement
- total talus replacement
- combined total talus replacement and total ankle replacement
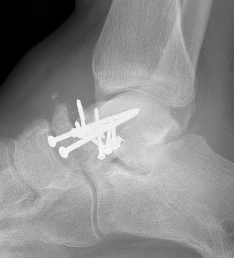
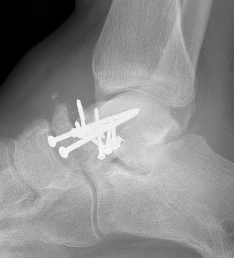
Pantalar fusion with hindfoot nail



Blair fusion
Concept
- excise necrotic talar body
- preserve talar neck
- sliding anterior tibial bone graft
- fill void with bone graft




Ilizarov Tibio-Calcaneal Fusion
Concept
- excise talus
- tibio-calcaneal fusion
- leg 3 cm short
- Ilizarov frame
- proximal corticotomy and lengthening
Total talar replacement
Issues
Dislocation
Instability
Degenerative joint changes of ankle and subtalar joint
Technique
Custom prosthesis based on CT of contralateral talus
JBJS Total talar replacement video
Results
Bischoff et al Foot Ankle Spec 2023
- systematic review of total talar replacement
- 20 articles and 160 cases
- average follow up 3 years
- complication 9%
- some improvement in functional outcomes
- mild improvement in ROM
- one amputation for pain and deformity
