Distal Tibial Fractures
Distal Tibial Fractures
Definition
Metaphyseal
Extra-articular
Intra-articular Extension
Metaphyseal
Extra-articular

Direct blow
- most common
Indirect
- forced knee flexion with foot fixed / maximally contracted quadriceps
1. Vertical

2. Transverse
I. Lateral Spilt
- seen in young patient
- lateral meniscus can be incarcerated in fracture
II. Lateral Split Depression
- often seen in young patients with high energy injuries
- vary in severity
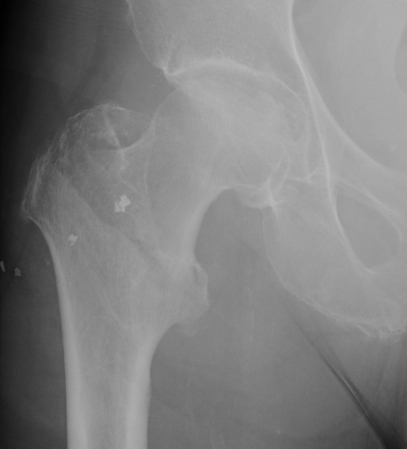
Fracture which extends between the trochanters of the proximal femur
- lower limit is inferior border of lesser tuberosity
Extra capsular / well vascularized
The key to stability is the posteromedial cortex
Largely related to degree of displacement
Hawkins Type I
- 0% to 13%

Hawkins Type II
- 20% to 50%
- usually only patchy and not a problem (rarely collapses)
Able to achieve relatively high level of function after STJ fusion
- previously believed that isolated STJ fusion should not be performed
- believed that triple arthrodesis was operation of choice for hindfoot
- STJ fusion has superior result with less stress on AJ
Average loss of DF 30% / PF 10%
Position of hindfoot determines flexibility of transverse tarsal (CCJ & TNJ) joints
- imperative that fusion be positioned in ~ 5o valgus

Usually a direct blow
- less commonly a fall on the outstretched hand
RTA / sporting accidents commonest causes
Can be pathological as a result of radionecrosis
- eg following radiotherapy for breast cancer.
Fractures of the clavicle are common
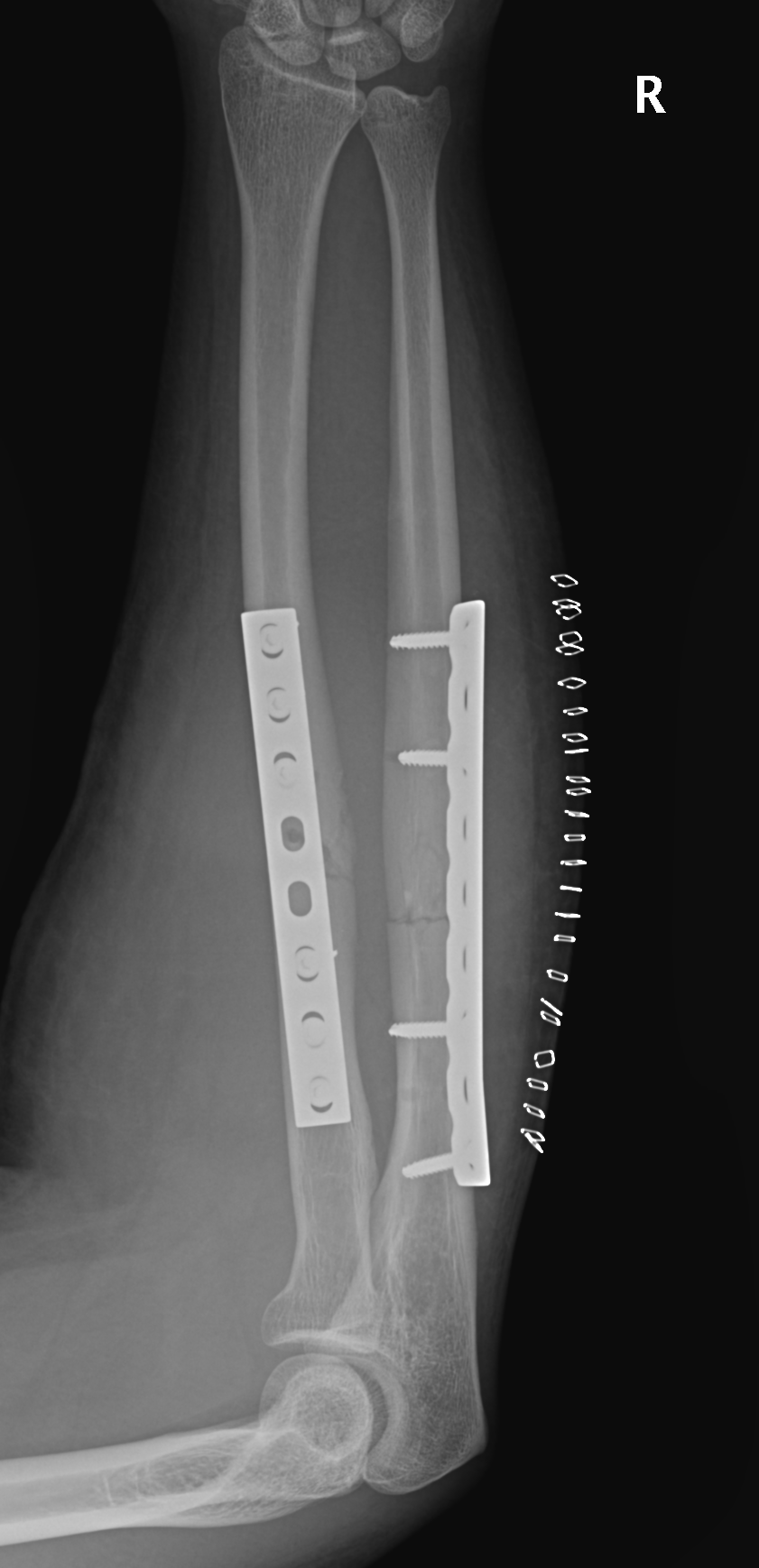
Radial bow radius
- important for rotation
Interosseous membrane
- Z pattern
- proximal radius to distal ulna
Direct blow
- ulna / night stick

Type I: Undisplaced avulsion fracture
Type II: Anterior portion displaced & hinged

Type IIIA: Displaced
Type IIIB: Displaced & Rotated