
Definition
Expansile pseudotumor of reactive hemorrhagic tissue arising in bone
Characterised by blood filled spaces separated by fibrous tissue
Site
Metaphysis of long bones
- proximal humerus
- femur
- tibia
Posterior elements of vertebra
Epidemiology
Teenagers
- 80% occur in 10-20 year range
- mean age 14 years
Female >Male
Symptoms
Pain
Mass
Pathological fracture
Natural history
Pathological fracture rare
May resolve with fracture or skeletal maturity
Types
Primary 50%
- arise de novo
Oliveira et al Am J Pathol 2004
- rearrangements of USP6 and/or CDH11 genes in 70% of cases
- absent in secondary ABC
Secondary / ABC like areas in other tumors 50%
- probably secondary to haemorrhage into primary tumour
- Giant cell tumour / chondroblastoma / osteoblastoma / osteosarcoma
- treat as underlying primary tumor
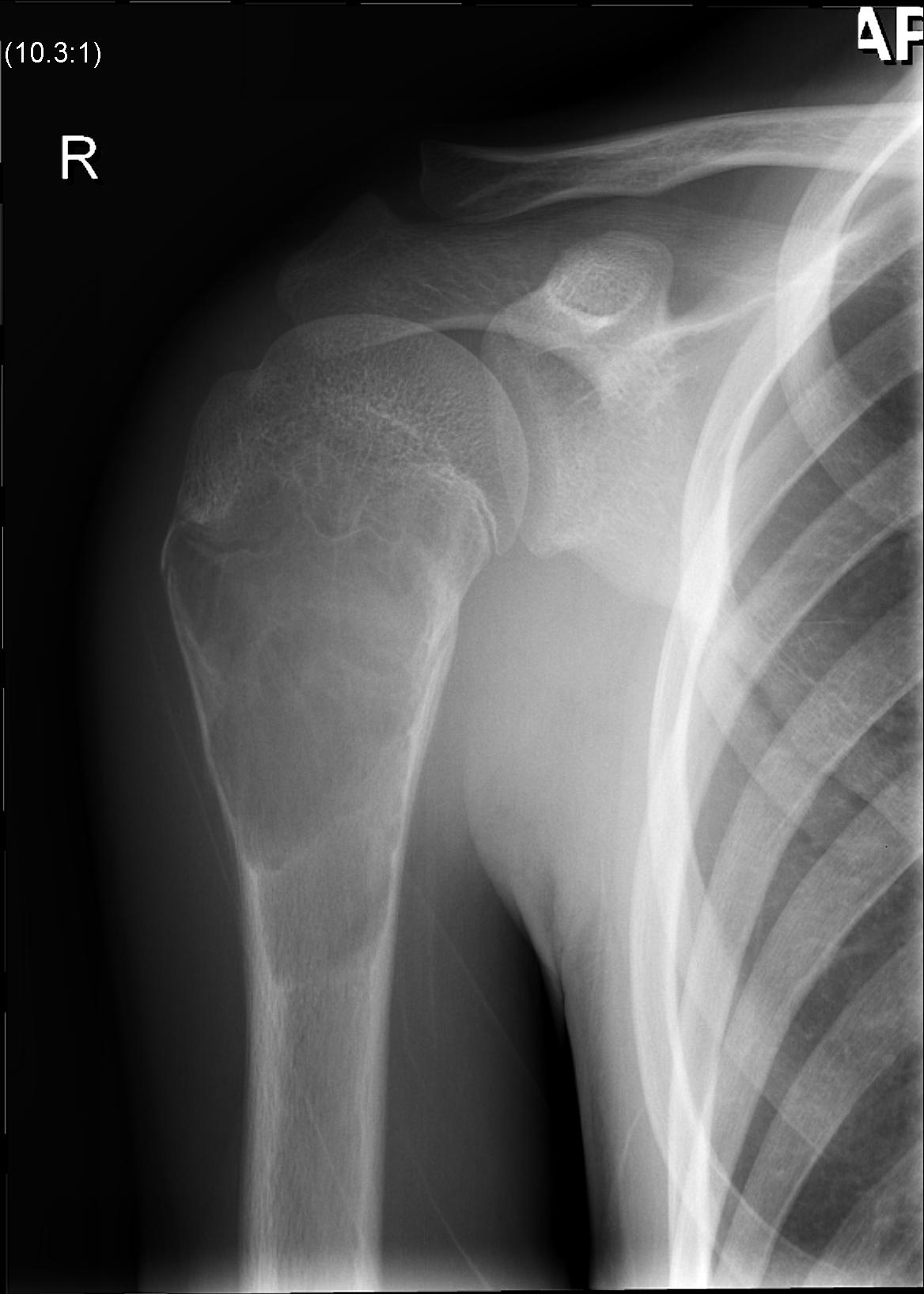
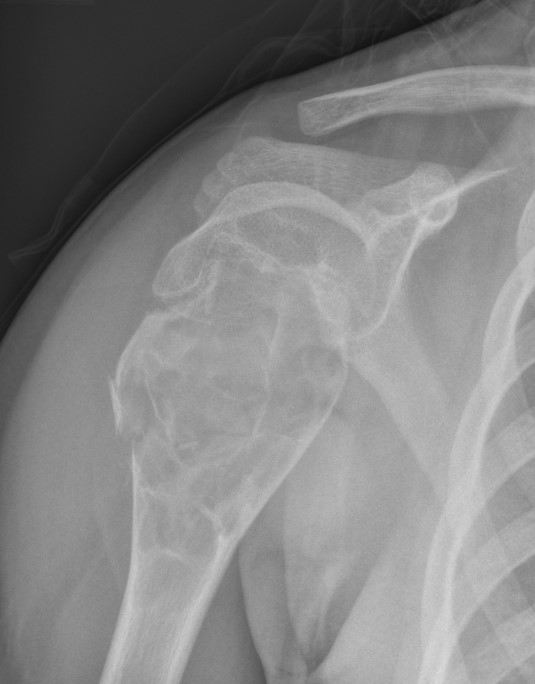
X-ray
Multi-loculated expansile lesion with cortical thickening
Often fail to make definitive diagnosis on xray


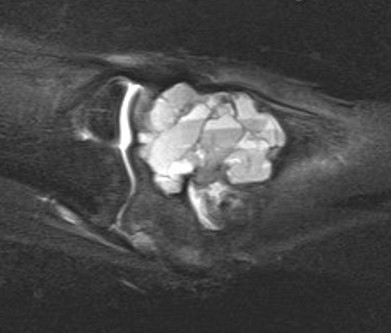
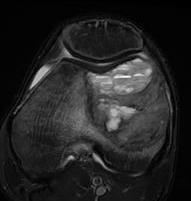
MRI
Usually difficult to determine UBC from ABC
- cystic lesions
- haemosiderin content - low to intermediate signal on T1 and T2
- borders and septae enhance with contrast
Gruenewald et al Br J Radiol 2023
- 36 patients with UBC or ABC
- fluid fluid levels / septation seen in both on MRI
- arterial feeders on MRA helped differentiate some ABC's


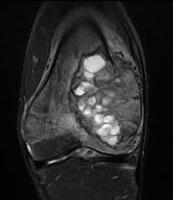
Fluid - Fluid levels
- due to sedimentation of RBC's & serum within the cavities
- patient must remain motionless for 10 minutes prior to the scan being performed
- allows time for sedimentation
- can also be seen in UBC
CT


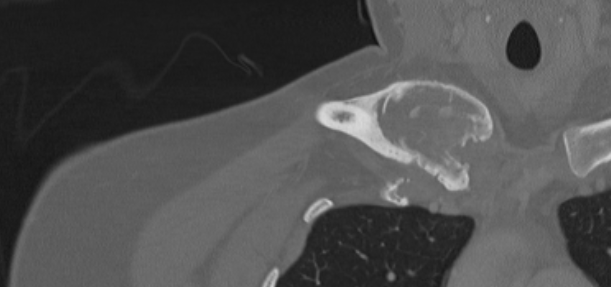
ABC medial clavicle
Bone Scan
Usually increased uptake
Exclude polyostotic disease
DDx
Fibrous dysplasia / GCT / Unicameral Bone Cyst / Infection / Osteosarcoma
Pathology
https://www.pathologyoutlines.com/topic/boneabc.html
Gross pathology
Blood filled spaces with fibrous septa
Histology
Cells
- haemosiderin-laden macrophages
- multinucleated giant cells
Septa
- fibrous stroma
- small amounts of osteoid
Genetics
- USP6 rearrangements
- no expression of H3G34W (GCT)
- no expression of H3K36M (chondroblastoma)
- no expression of SATB2 (osteosarcoma)
Management
Nonoperative Management
Observation
Avoid contact sports
Interventional radiology
Sclerotherapy
Embolization
Injection of demineralized bone matrix / bone marrow
Results
Cruz et al Eur J Orthop Surg Traumatol 2021
- systematic review comparing sclerotherapy to embolization
- 13 studies with 416 patients
- recurrence embolization 19%
- recurrence sclerotherapy 6%
Sclerotherapy
- injection of sequential intralesional percutaneous polidocanol in 43 patients
- complete resolution in 37/43 at one year, and 43/43 at two years
- 72 patients with ABC with mean age 15
- treated with percutaneous intralesional 3% polidocanol
- average number of injections of 3 (range, 1 - 5)
- 10/72 patients cured with single injection
- 2/72 (3%) had recurrence at 2 years, successfully treated again with sclerotherapy
Selective Arterial Embolisation
Indications
- difficult to reach locations
- spine / pubis / sacrum
Results
- 102 cases of ABC treated with arterial embolization with 7 years follow up
- feasible in 88 (86%) of patients with a feeding artery
- overall 82% success
- successful in 57% with one embolization, 19% two embolizations, 6% three embolizations
- 18% recur and require surgical intervention
Autogenous bone marrow / Demineralized bone matrix
- 13 aneurysmal bone cysts
- small incision
- injection of demineralized bone and autologous bone marrow
- healing in 11/13
Andreani et al Stem Cells Int 2020
- 42 ABCs treated with injection of BMC (bone marrow concentrate)
- 32/42 healed with 1 injection
- 7/10 healed with second injection
- 2/3 healed with third injection
Operative Management
Indications
Failure minimally invasive treatment
Joint space threatened
Weight bearing joints
Options
Currettage and bone graft
Currettage / bone graft / fixation
Allograft / Joint Replacement
Results
Strohm et al Eur J Trauma Emerg Surg 2023
- meta-analysis of 163 studies
- currettage had 91% healing and 22% recurrence
- currettage and autologous cancellous bone graft had 96% healing and 15% recurrence
- case series 53 patients
- closer to physis = higher recurrence rate
Currettage and bone grafting
Indication
Must be able to preserve articular surface
Technique
Full and careful curettage
- intra-lesional treatment
- need to burr away all of lesion
- must take care as bone very thin
- areas of fracture not uncommon
- must beware growth plates in skeletally immature
- supplement with bone graft / bone marrow aspirate / PMMA



Results
Cevolani et al J Tissue Eng Regen Med 2021
- 239 patients treated with curettage and bone graft
- healing in 177/239 (74%) at 42 months
Syvanen et al Scand J Surg 2018
- 18 cases treated with curettage and bioactive glass
- 2/18 (11%) recurrence
Currettage / Bone graft / Fixation




Resection and arthroplasty
Indications
Articular cartilage not salvageable
