Observation
Curves < 20o observation only at 3-6 month intervals depending on growth rate
Non Operative Management / Bracing
Never brace curves if patient Risser 4 or 5
Indications
1. Risser 0-2 (growth potential)
2. Curve >30o adolescent
3. Curve >25o with progression (5o in six months)
4. < 10 years old
- very young with high progression potential
- high risk crankshaft if operate
5. Willingness to comply
Guidelines
Angle High Growth Potential Lowth Growth Potential
<20° observe observe or DC
20°-30° observe/brace observe
30°-45° brace observe
>45° surgical surgical / observe
Effect
Will control curve only
- end result is initial curve + 5o
Brace should be customised to patients curve
- designed to prevent progression NOT to achieve correction
- generally see a moderate amount of correction when using the brace
- then slow steady progression of curve back to original magnitude during weaning
- best curves to brace are those < 40o
Bracing complications
Failure to prevent progression
Skin irritation
Pressure areas
Abdominal discomfort, eating habit disruption
Cast syndrome - SMA / duodenal obstruction
Psychological
Milwaukee Brace / CTLSO
Best for curves with apex above T8
- three point fixation technique
- less efficacious for curves > 40o
Consists of
- well moulded pelvic piece above the iliac crests (most important)
- two posterior uprights and one anterior upright
- neck piece with plastic throat mould anteriorly and two occipital pads posteriorly
- thoracic pad placed over the apex of convexity of curve
- lumbar pad over TP between lowest rib and iliac crest on concave side
- active correction by muscle contraction pulling body away from pads
Protocol
23 out of 24 hours a day
- result dependant on time in brace
Need to check regularly and readjust after 1-2 weeks
- Xray on 6 month basis
- if progresses > 45o then surgery
Aim for 30-50% correction in first 6 months
- if not achieved consider surgery
Weaning
Once skeletal maturity / Risser 4 / full height
Wean
- 20 hours for 4 months
- 16 hours for 4 months
- 12 hours for 4 months
- night time only for 4 months
TLSO (Under arm or Boston Brace)
If apex < T8
Higher compliance
May not be as efficacious in holding correction
Made from cast
Operative Management
Indications
1. Immature / Risser 1 /2
- Cobb > 40o with documented progression
- peak height velocity
- will progress 1o per month
- need to stabilise early
2. Mature
- T > 45 - 50o
- TL or L > 30o with marked rotation
- double major > 50o
- significant coronal imbalance
- cosmetic deformity
- failure bracing
This curve will progress slowly
- patient has time to make up mind
Goals
Solid arthrodesis that prevents progression
Balanced spine
Correction of deformity
Prevent respiratory compromise
Options
1. Most curves
- posterior instrumented fusion
2. Lumbar curves
- anterior instrumented fusion
3. Large curves > 70o / young patients
- anterior and posterior surgery
Principle
Fuse the structural curve with minimum segments
- to stable vertebra
- minimise the levels (preserve motion segments)
- avoid to L5 and above T1 (may increase pain)
- if fuse to L5, only 1 motion segment left, risk LBP
Correct curve in sagittal and coronal planes
Best to wait til 10 - 12 years to avoid crankshaft
Structural Curve
1. Largest curve
2. One to which trunk shifted
3. Least correction on AP lateral bending Xray
4. Pedicles rotated
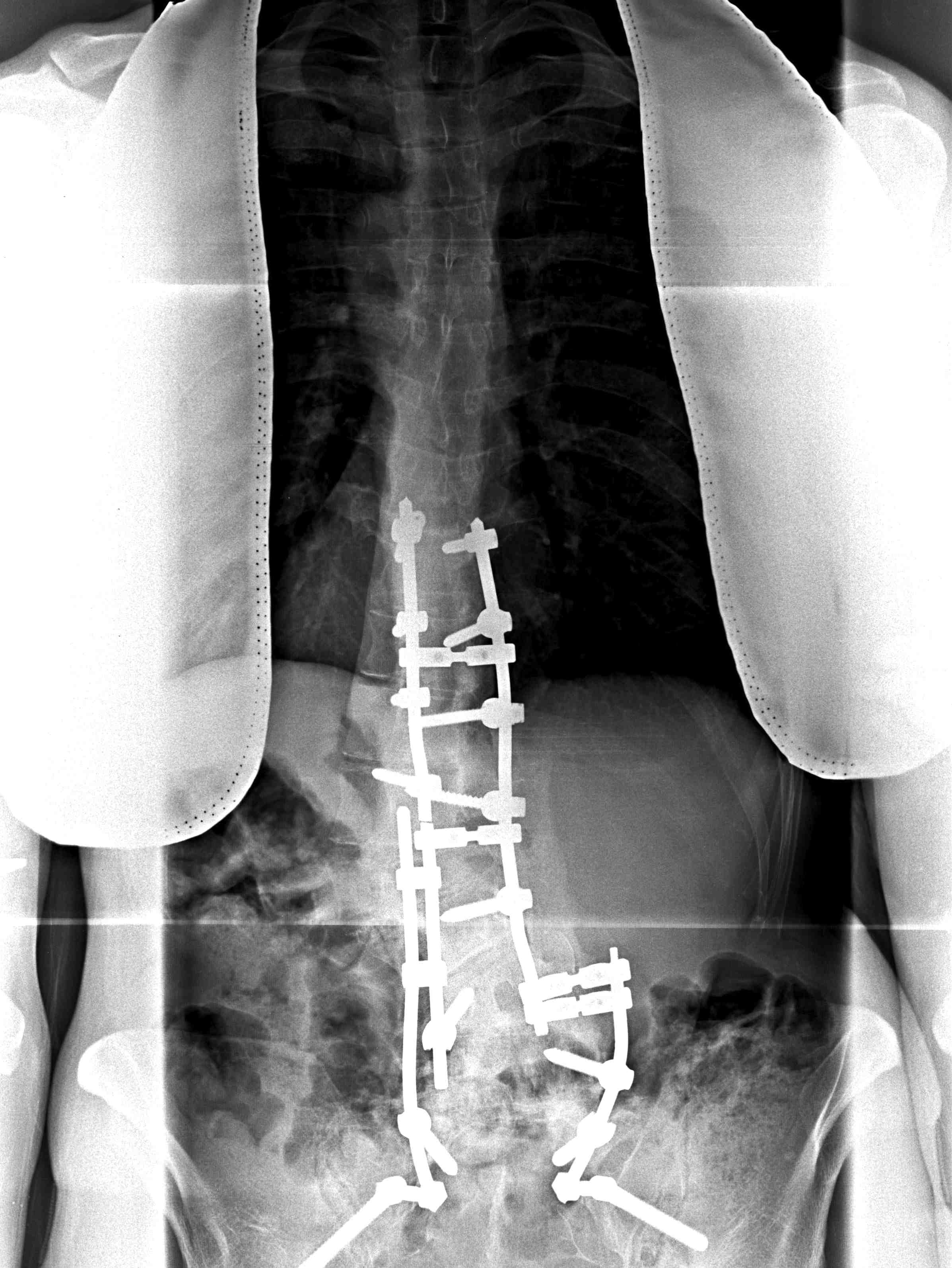
Posterior Instrumented fusion
Multisegmental Hook and Pedicle screw systems
- allows for correction via Compression / Rotation / Distraction
Crankshaft phenomenon
Concept
- seen in young child with high growth potential
- pre PHV surgery or with open triradiates
- pivot on posterior fusion
- vertebral bodies and discs bulge towards convexity
Problem
- get loss of correction, increase in rotation, recurrence of rib hump
At risk
- Risser 0
- girls < 10
- boys < 13
Specific Surgery
Lenke Type 1
- main thoracic
- posterior stabilisation
- usually limit to T4 as shoulders equal

Lenke Type 2
- double thoracic / MT and PT
- need to instrument to T2
- equalise shoulders
Lenke Type 3
- double major / MT and TL/L
- long posterior instrumented fusion
Lenke Type 4
- triple major
- very long posterior instrumented fusion
Lenke Type 5
- thoracolumbar / lumbar curve
- can fuse short curve this through bed of T9 / T10 rib
- otherwise posterior instrumented fusion
Lenke Type 6
- TL > MT structural
- long posterior instrumented fusion
Technique Posterior Instrumented Fusion
Pre-operative
Consent
Cell saver
- accumulate large blood loss
- often large exposure
Xmatch blood
2 x milled femoral head allograft
Spinal monitoring / SSEP's
- needles scalp / hands / feet
- begin pre-op once asleep as baseline
IDC
Pedicle screws / TP hooks / rods available
Post op ICU bed especially neuromuscular
Position
4 Poster Bed
Protect eyes, knees, elbows
No pressure on abdomen / reduce venous bleeding
Dissection
Posterior approach
- betadine pack buttocks
- midline incision
- divide thoracolumbar fascia midline
- split apophysis with knife (if present)
- subperiosteal elevation strap muscles
- use diathermy, cobb
- sequentially pack with rolled up packs to control bleeding
Lumbar spine
- expose facet joints and transverse processes
- don't go between transverse processes laterally as nerve roots here
- pedicle screws inserted bilaterally bottom 3 pedicles
Thoracic
- TP hooks above
- pedicle hooks below
- compress
2 x rods prebent in sagittal plane
- correct coronal malignement and rotation as able
- may use sublaminar wires if large long curve
- midsection of curve in concavity
- tie over rod and tighten to correct
Decorticate lamina, add bone graft along each side
Closure
Technique Anterior Fusion
Indications
Large lumbar curve in young patients
- skeletally immature patient to achieve growth arrest and prevent crankshaft
Any lumbar curve to decrease fusion length
- this is debatable
Large / rigid curve to achieve mobility
- severe curves >70o
- supplement posterior fusion
Advantages
Fewer levels instrumented
Better correction of rotation
Large surface for fusion
Fusion under compression
Use rib as bone graft
Disadvantages
Requires anterior approach
Does not produce lumbar lordosis
Respiratory problems (need chest drain)
Need to divide segmental vessels
Technique
Supine, rolled
- curved right sided approach
- remove 9th rib (save for bone graft)
- through bed of rib
- identify peritoneum, stay outside
- take down diaphragmatic crura
- divide segmental vessels, remove discs
- unilateral screws and rod
- repair diaphragm, close over ICC
Endoscopic Anterior Instrumentation
Advantages
- reduced blood loss and pain
- better scars and cosmesis
Disadvantages
- technically difficult
- respiratory problems / deflate lung
Growing rods
Indications
Growing children / open triradiate cartilage
- avoid fusion / crankshaft phenomen
- biannual surgery
- high complication rate 50%
- hook dislocation
- rod breakage
Costoplasty / Thoracoplasty
Technique
Partial excision of 5 or 6 ribs from the TP to posterior axillary line
Advantage
Corrects the rib hump
Cosmetic procedure
Good source of graft
Does not affect the post op morbidity or pulmonary function
Complications G. Coe SRS Report 2006
Early
Neurological
0.32% in posterior corrections (SRS) in adolescents
- 2% in adults
- highest in congenital curves
Prevention
- SSEP's monitoring in all idiopathic and congenital curves
- wake - up test in suitable patients (difficult in children)
SSEP's
- stimulate in legs, readings in cortex
- avoid inhalation anaesthetics
- time delay as must average amplitudes and reduce background noise
- issue if lose > 50% amplitudes
If lose SSEP's
- avoid hypotension
- transfuse Hb if low
- check electrodes
- wake up test
- give steroids
- reverse correction
- remove instrumentation
Infection 1.35%
Prophylaxis warranted
Late chronic infection with Proponiobacterium acnes
Respiratory 1.6%
- PTX
- atelectasis
PE 0.02%
Death 0.03%
Ileus - very common
Blood Loss
Avoided with
- autologous blood
- cell savers
- hypotensive anaesthesia
- autotransfusion
- often blood loss that contributes to neurological compromise
Incorrect fusion levels / wrong level surgery
SIADH secretion
- decrease UO night of surgery
- steady improvement 2-3/7
Late
Pseudoarthrosis
- 1% overall
- instrument failure
Crank shaft Phenomena
In rapidly growing child after posterior fusion
- spine will rotate as the bodies grow anteriorly
- thus if child with significant growth then add anterior discectomies and fusion
Other solutions
- posterior growing rods
- anterior staples / guided growth
Sagittal malalignment
- loss of lumbar lordosis
- flat back / loss of thoracic kyphosis
Back Pain
Related to fusion below L4 and loss of lumbar lordosis
Levels and back pain
- L5 - 80%, L4 - 60%
- L3 - 40%, L2 - 20%
Late infection - low virulence organism
Results
Gothenburg Sweden 1968
- 23 year follow-up post fusion with instrumentation
- preop Cobb 62°; postop 33°; last followup 37°
- same series had 127 patient braced
- prebrace 33°, best brace position 30°, last followup 38°
