Definition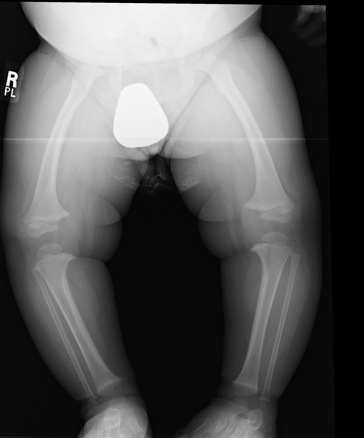
Progressive varus deformity of knees
- secondary to abnormality of medial upper tibial physis
- localised varus & internal rotation deformity
Infantile form
- onset 1-3 years / bilateral
Adolescent form
- onset > 6 years / unilateral
- 5 times less common
- M:F
- presents 8 - 14 years
Epidemiology
Africans / African Americans / West Indians
Associations
Female
Obesity
FHx
Early walking
Aetiology
Unknown / Multifactorial
Familial
- no consistent inheritance pattern
- ? related to tendency to obesity
Mechanical
- most likely due to abnormal compression on medial side of proximal tibial physis
- causes retardation of growth
- ? traumatic role
Pathology
Posteromedial disordered endochondral ossification
- dense islands of hypertrophied chondrocytes
- acellular areas of dense fibrocartilage in resting zone
- abnormal groups of capillaries
Fragmented physis
Clinical
Infantile presents at 12-36/12
Bilateral & symmetrical
- bowing noted when commence walking
- associated internal tibial torsion due to fibular tethering normal ER of tibia with growth
- continuum between physiological vara & Blount's (infantile may be severe physiological vara)
- varus should resolve by the age of 2
Examination
Milestones / height & weight percentiles
Knee ROM
Measure of Genu Varum & Tibial torsion
Ligamentous Laxity
X-ray
Indications
- severe genu varum
- rapidly worsening
- height < 25th percentile
- marked asymmetry
- FHx
Findings
- localised deformity at proximal tibia
Metaphyseal - Diaphyseal Angle
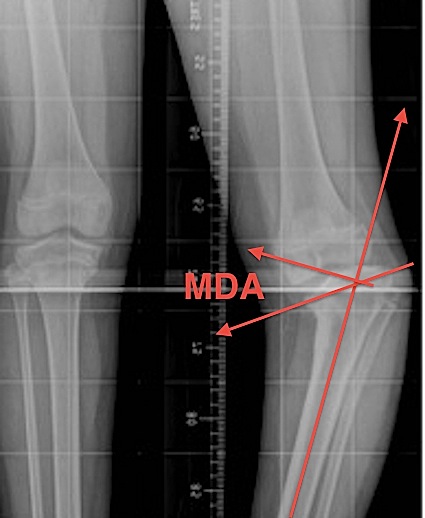
Technique
- line drawn perpendicular to axis of tibia
- line drawn through medial & lateral beaks of metaphysis
- Blount's > 11°
- physiologic bow legs < 11°
Measurements
- 11° is arbitrary cut off where Blount's is more likely
- 16o definite
Medial Physeal Slope
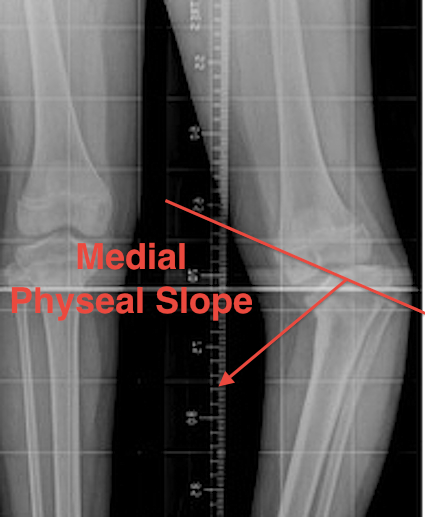
Technique
- line through medial physis & line through lateral physis
Measurements
- significant if > 60°
- prognostic of progression
CT
Used to identify presense of physeal bar
Langenskiold Classification
Stage I: Beak 2-3 years
- irregular metaphyseal ossification
- medial metaphyseal beaking
Stage II: Saucer 2-4 years
- saucer shaped defect in medial metaphyseal beak
- medial epiphyseal wedging
Stage III: Step 4-6 years
- saucer deepens into step
- medial epiphysis irregular
Stage IV: Bent plate 5-10 years
- growth plate inclined distally at medial side
- i.e. epiphysis extends down over meta beak
Stage V: Double epiphysis 9-11 years
- Xray appearance of severe posteromedial depression
Stage VI: Medial physis ossified 10-13 year
- medial physeal closure

DDx
Physiological varus
Metaphyseal dysplasia / achondroplasia
Ricket's
Trauma / Tumour / Infection
OI
JRA
Physiological Varus
- symmetrical involvement
- normal growth plate
- medial bowing of proximal tibia & distal femur
- metaphyseal-diaphyseal angle < 11°
Rickets
- short stature, osteopaenic
- widened physes / cupped metaphyses
- distal Femur Flared too
- may have coxa vara
- hypophosphataemic most common
Renal Osteodystrophy
Metaphyseal Chondrodysplasia
- widened metaphysis, cupped physis
- similar to rickets
- mild short stature
- may have coxa vara as well
Focal fibrocartilagenous dysplasia
- generalised abnormality or focal deformity in tibia
OI
Trauma
Infection
Tumor
NHx
Progresses to severe OA by early adulthood
- metaphyseal-diaphyseal angle >11° --> likely to progress
- medial-physeal slope >60° likely to progress
- Philadelphia sign: lateral subluxation of tibial epiphysis
- if restore normal valgus should have good outcome
Need to manage child before they develop a bar (i.e. end stage of growth plate injury)
Management Infantile Type
Algorithm
Depends on
- age of child
- stage of disease
1. <2 years
Observe
2. 2 - 3 years & Medial Physeal Angle < 60°
KAFO Single Medial upright
- free ankle with no knee hinge
- flexion limited
- knee cuff pulls it into valgus
Full-time bracing successful > 50%
3. Age > 3 years / Progression in Brace / Medial Physeal Angle > 60°
Aim
- correct varus and internal rotation deformity
Options
A. Lagenskiold I - IV
- osteotomy
- guide growith
B. Lagneskiold V / VI
- take down bar and osteotomy or
- epiphysiolysis + medial metaphseal osteotomy
Langenskiold Stages I-IV Surgical Management
1. Osteotomy
Aim
- restore alignment
- deformity reversible
- if restore physiological valgus (7o) then resolution is usual for I & II / possible for III & IV
Type of osteotomy
A. Opening / closing wedge
B. "Smiley" upside down dome
C. Oblique osteotomy
- Rab biplanar oblique osteotomy
- fix with single screw
Osteotomy Technique
Performed distal to TT
- closing wedge simplest but upside down dome has least shortening
- must osteotomise fibula
- usually want to correct IR deformity at same time
- must release anterior compartment to prevent compartment syndrome
- desired valgus & ER achieved
- fixation with K wires or screw
- POP post operatively
Recurrence after osteotomy
1. Obese
2. > Stage III
3. Medial physeal slope > 60°
4. Age
- > 5 y = 76%
- < 5 y = 31%
2. Guided growth / 8 plate
Now common mechanism of treating condition
3. Osteotomy and external fixation
Langenskiold Stages V & VI
Issue
Irreversible
- need to address physis as well as osteotomy
- usually total physiodesis
- overcorrection 10°
Surgery
- must do fibula osteotomy as well
- usually perform total physeodesis of ipsilateral side
- always perform fasciotomy
- may need to realign epiphysis in severe forms with large medial-physeal slope
- consider epiphysiodesis of other side to address LLD
Options
1. Medial Metaphyseal Elevation Osteotomy
Indications
- Grade V

2. Physeal Bridge Resection (physeolysis) + Osteotomy
Indications
- Grade VI
- bridge < 30% of physis
Technique
- excise bar where CT shows a bridge
- Insert fat into defect
3. Lateral Hemi-epiphysiodesis + osteotomy
Indications
- grade VI
- bridge > 30%
Technique
All need fibula osteotomy
All need prophylactic compartment release
Complications
Compartment syndrome - must prophylactic release
Recurrence of varus - usually secondary to physeal bar
LLD
OA
Adolescent Type
Management
Wait till skeletal maturity, then HTO
