Epidemiology
Prevalence of 25-100%
Ambulation
- walking decreases incidence
Age
- worse with young onset
Aetiology
Exact biomechanical explanation of origin & progression of curves unclear
Associated with
- weakness
- poor muscle control
- no proprioception
Classification
1. Neuropathic
A. UMN
- CP
- Friedrich's
- cord tumour / trauma
- CMT
B. LMN
- Polio
- Spinal muscle atrophy
- Spina Bifida
2. Myopathic
- Arthrogryposis
- Muscular Dystrophy
- Myotonia Dystrophica
NHx compared with Idiopathic
Onset younger
More rapid progression
Progression after skeletal maturity / throughout life
Longer curve
Cervical involvement
Pelvic obliquity
Pulmonary complications common
Curve
Long C shaped curve
- compensatory curve uncommon but possible
Curve associated with
- pelvic obliquity
- hip contractures / dislocation
- cervical involvement
Other problems
Lung disease common (decreased FVC, LRTI)
Poor nutrition
Pressure areas
CRF in Spina bifida
Management
Aims
Maintain cardiorespiratory function
Promote mobility & ambulation
Preserve sitting balance
Improve cosmesis
Principles
Brace till 12 years then fuse
Earlier if
- lose control with rapid progression
- large curve
Nonoperative
Indications
Small curves < 30°
Large curves in patients with very poor prognosis
Orthoses
Best overall initial treatment
- rate of progression slowed
- allows further spinal growth before definitive treatment
TLSO
- 2 piece custom moulded
- used to control & correct scoliosis or kyphosis in growing years
- preferable to Milwaukee brace in NM conditions
- easier to make and wear with reduced incidence of press sores
- worn during day while child is upright
- off at night
Seating
- very important
- aims to give trunk & spine control
- able to correct postural curves
- no effect on structural curves
- significantly decreases nursing & handling time
1. Tumbleform Seat
- moulded seat for infants
- 3 sizes
2. Commercial Chairs
- pelvic support, abduction pillow, thoracic support, head support
3. Moulded Sitting Support Orthosis
- AKA SSO
- custom fitted support made from patient mould
- provides maximum sitting support with padded supports & belts
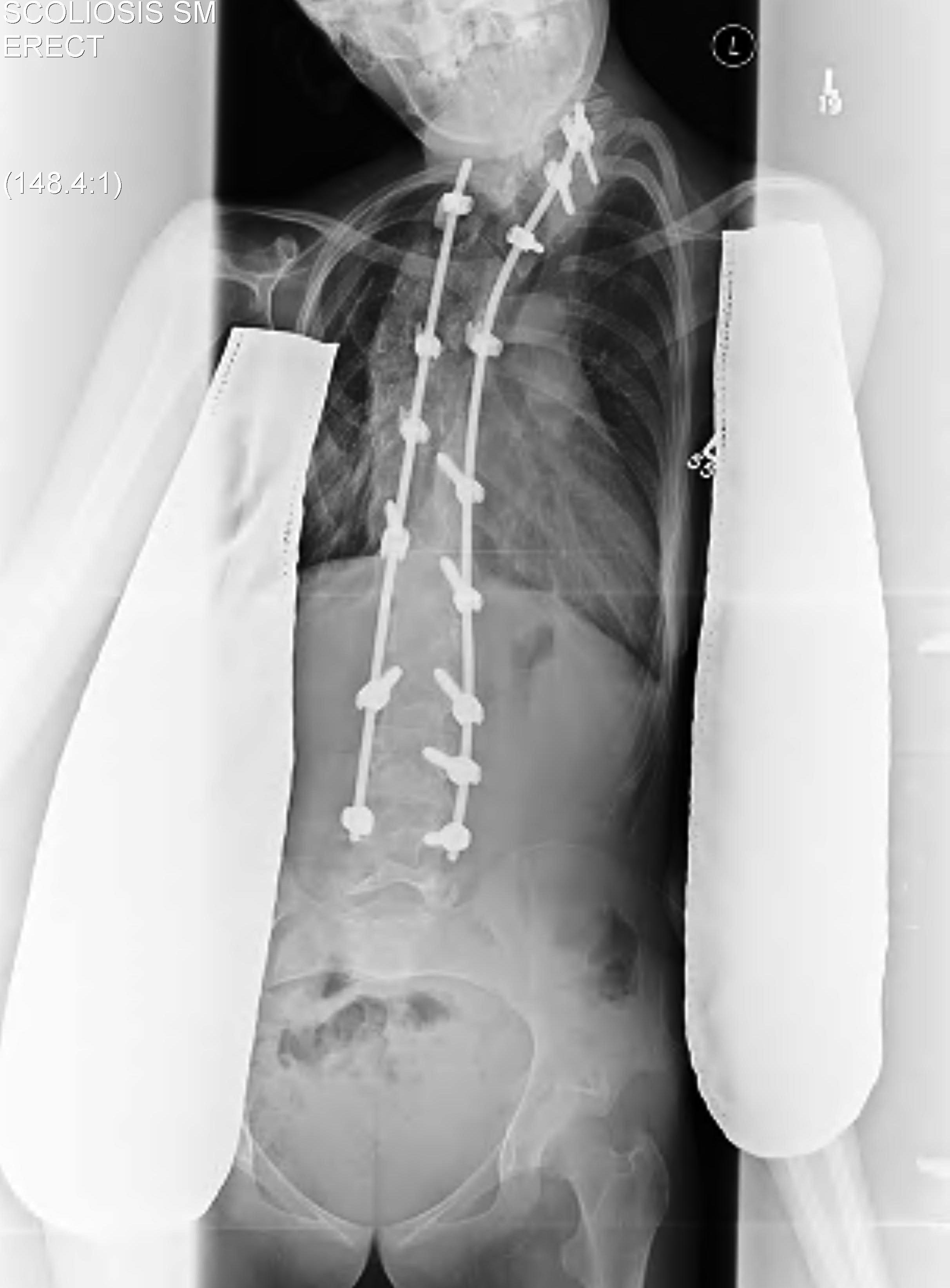
Surgery
Aim
Solid arthrodesis of balanced spine over level pelvis
Requirements
Long, solid fusion from upper thoracic to lower lumbar
Rigid instrumentation & massive bone grafting
Issues
Increased bleeding
Osteopenic bone / Poor hold
Fusion to pelvis
High pseudarthrosis rate
Poor medical state
Ambulation
- fusion may eliminate ability to ambulate
- trunk movement may be important for ambulation
- obviously lose any spinal movement with flexion
- should test in brace first
- may need to limit extent of surgery
Preoperative
General medical workup
- cardiopulmonary status
- especially Friedreich's & Duchenne MD
- FVC1, FEV, ABG's
Book ICU bed
Approach
Posterior
- most common especially in CP
- moderate curve
Staged Anterior / Posterior
- severe kyphosis / severe rigid scoliosis (> 45°)
- posterior fixation compromised (SB)
- < 9 years to stop crankshaft deformity
Technique
Require
- spinal cord monitoring if indicated
- cell saver
- post op ICU bed or HDU
- IDC
Instrumented fusion
- proximally from T3 or T4 to prevent later subsequent deformities
- caudally to pelvis if >15° pelvic obliquity
- to L4 or L5 if balanced
- often need sublaminar wires for large C shaped curve
- place in midcurve to pull spine to the rods
- large fusions require allograft
Blood Loss
- issue because extensive approach / small blood volume / osteopenic bone bleeds+++
- addressed with meticulous haemostasis / hypotensive anesthesia / haemodilution / cell saver
Complications
Pulmonary complications
- most common cause of death
- nearly all CP patients get pneumonia post op
Neurological injury
- especially if correcting curve > 90°
- spinal monitoring
- if damaged when wake up, remove metalwork
SIADH
- careful fluid balance
Infection
- bacteraemia from remote sites especially UTI
- increased incidence of wound infection
Loss of ability to ambulate
- due to loss of trunk flexion and extension
Cerebral Palsy
Most common neuromuscular cause of scoliosis in western world
Principles
Professor Bruce McPhee, Royal Brisbane Hospital
- key is that they all continue to progress past maturity
- says as general rule all need operation so can pick your timing
- try not to fuse too early as get very short trunk
- no longer goes to pelvis
- feels that stopping at L5 is adequate and pelvis is not worth the morbidity
- insists CP patients have their operation at 50o
- if families decline he won't operative at 70-80o because then they need 2 stage
- high associated morbidity
- follow up every 6 or 12 months
Incidence
10% in ambulatory patients
70% spastic quadraplegics
Lonstein Classification
Group 1 curves (A&B) have level pelvis
- double thoracic curve
- little pelvic obliquity
- fuse as for idiopathic
Group 2 curves (C&D) have pelvic obliquity
- large lumbar or thoracolumbar curve
- marked pelvic obliquity
- fuse long (T4) to pelvis
Algorithm
Observation
- curves up to 30˚ in the growing child
- curves up to 50˚ in skeletally mature
Orthoses
- often only postpones arthrodesis until puberty
- seating most common form of non-operative treatment instituted
- TLSO effective in ambulatory patient
Surgery
Fusion to sacrum essential with pelvic obliquity
- Galveston technique (iliac wing rod fixation)
- pedicle screws only viable in S1, not S2
Spina bifida
Incidence
>60% of patients with myelomeningocoele develop scoliosis
Principles
The higher the level the more severe
- T12 - 100%
- L1 - 90%
- L2 - 80%
- L3 - 70%
- L4 - 60%
- L5 - 25%
- S1 - 10%
40% incidence of spinal dysraphism
- may cause scoliosis progression
- hydrocephalus, syringomyelia, tethered cord, Arnold Chiari
20% have congenital component
Most require surgery
Why fuse wheelchair bound Spina Bifida children?
Physiological
RFT's
Feeding
- often use peg
- tends to disappear into skin folds
- hygiene & technical difficulties
Acid reflux when hunched over
Only tolerate small feeds
Physical
Pressure areas
Ability to nurse
Takes arm off chair so can do ADL's
Allows stable sitting
Pelvic obliquity
Allows coverage of hips
Psychosocial
Self-esteem both patient & carer
Allows better interaction with environment
Poor prognostic signs
Early age of onset
Asymmetrical motor paralysis
Presence of spasticity
10% - 20% have congenital scoliosis
Algorithm
Curve 20-40˚
- TLSO
- but bracing complicated by pressure sores
Curve > 40˚
- anterior and posterior fusion
- need anterior as posterior elements deficient
- pelvis may be deficient
- attempt to preserve lumbosacral segments to aid wheelchair transfers
Duchenne's muscular dystrophy
Incidence
Usually lose ability to walk during age 9-12 years
- due to progressive weakness
- 80 - 100% develop severe collapsing scoliosis
May progress rapidly (2-3˚/ month)
- can progress to 100o
- 10o per year once in chair
Issues
Affects ability to sit
Scoliosis is life threatening
- progressive respiratory compromise
- due to respiratory muscle weakness and curve
- with curve > 35˚, vital capacity 40% of predicted
- further compromises respiratory problems
- death occurs in late teens to early twenties
- may be delayed by curve correction
Bracing
Orthotic use little success
- almost all progress
- slows progression (15˚ / year comparted with 30˚ / year)
Surgery Indications
Curve greater than 30o
FVC < 30% predicted
Life expectancy > 2 years
Surgery
Only posterior
- anterior compromises respiratory function too much
Spinal muscular atrophy
Most patients develop scolioses
- onset by age 7
- usually progressive
- consider surgical treatment when curve reaches 40o
- large C shaped curves
- T2 to sacrum
Friedreich's ataxia
All have scoliosis
- 50% have hyperkyphosis
- curve patterns resemble idiopathic rather than neuromuscular
- curves appear later
- late teens or early 20's
- consider surgical treatment when curve reaches 40o
Paraplegia and quadriplegia
Incidence
Age related with risk of spinal deformity
- 90% if cord injury preadolescent
- due to loss of sensory / proprioceptive / motor functions supporting the spinal column
Posttraumatic angular deformities related to crush fractures
