

Incidence
van Erp et al Arch Orthop Trauma Surg 2022
- systematic review of 174 studies and 5 million THA
- overall incidence of dislocation 1.7%
- reducing over time
- dislocation rate 2010 - 2020 0.7%
Factors
Kunutsor et al Lancet Rheum 2019
- meta-analysis of risk factors for dislocation
- 125 studies and 4.5 million THA
| Patient factors | Surgical factors |
|---|---|
| AVN / RA / neck of femur fractures | Surgeon experience |
| Revision THA | Surgical approach |
|
Females Elevated BMI Medical co-morbidities (ASA 3) Neurological conditions Psychiatric disorders |
Implant factors - component position - femoral head size - elevated liners - dual mobility |
| Abnormal spinopelvic motion |
Soft tissue balancing - offset and LLD |
| Impingement |
Surgical factors
1. Surgeon Experience
- 4000 THA at once centre
- dislocation rate 2 x with < 30 THA per year
2. Approach
Koster et al J Orthop Trauma Rehab 2023
- meta-analysis of 11 studies and 2,000 patients undergoing THA
- overall dislocation rates 0.8%
- posterior 1.4% / anterior 0.4% / lateral 0% (non-significant differences)
Steenbergen et al Hip Int 2023
- Dutch registry of 270,000 THA
- posterior 1.4% / anterior 0.4% / lateral 0.6%
3. Component position

Acetabular safe zones
- inclination 40 +/- 10o
- anteversion 15 - 30o
- 9800 hips
- evaluated Lewinnek safe zone
- cup inclination 40+/-10
- cup anteversion 15+/-10
- 58% of dislocations had cup position within safe zone
4. Component design
A. Increased head size
Increased size increases head-neck ratio
- reduces impingement / increases arc of motion
- increased jump distance
Zijlstra et al Acta Orthop 2017
- Dutch Registry of 166,000 hips
- dislocation rates higher with 22 - 28 mm heads compared to 32 mm heads
- 36 mm heads reduced dislocation rates with posterolateral approach
B. Acetabular liners

Stryker elevated liner
Posteriorly elevated profiles
- i.e. neutral liners v 10o elevated rim liners
- ? more common in posterior approach
- 213 THRs on UK registry
- asymmetric liners have lower revision rate
- both overall revision, and revision specifically for dislocation
- 5000 THA
- elevated liners reduced dislocation rate
C. Dual mobility
Romagnoli et al Int Orthop 2019
- systematic review of 15 studies and 2400 patients
- comparison of dual mobility with standard THA
- reduced risk of dislocation with dual mobility
5. Soft tissue tension
A. Restore LLD and offset
- reduced offset associated with increased dislocation
- reduces soft tissue tension
- increases risk of impingement
B. Capsular Management
Kobayashi et al Arch Orthop Trauma Surg 2023
- systematic review of capsular resection versus capsular repair
- lower dislocation and better HHS with capsular repair
6. Impingement
- remove osteophytes
- restore LLD and offset
- always put hip through ROM
- ensure in full extension and ER, no posterior impingement between neck an
- ensure in flexion 90o and IR, no anterior impingement
Patient factors
Spinopelvic mobility
Abnormal spinopelvic motion from lumbar pathology can lead to increased dislocation risk
- impingement from decreased pelvic motion
- impingement from compensatory femoral motion
- ongoing spinal degeneration can alter relative cup position
- spinal surgery can alter relative cup position
- spinal deformity on table can alter perceived pelvis landmarks
Gausden et al, J Arthroplasty 2018
- USA registry review of > 200,000 THRs
- strongest risk factor for dislocation was prior spinal fusion
- meta-analysis (n=69,438) comparing prior vs subsequent lumbar fusion
- lumbar fusion is risk factor for dislocation, regardless of timing (before or after)
Management
- not yet born out with clinical evidence
- functional imaging (EOS or XR) to compare pelvic parameters (pelvic tilt, sacral slope) sitting and standing
- CT navigation or robotics can be used to identify impingement / accurately place implants
- consideration of dual mobility
Positions
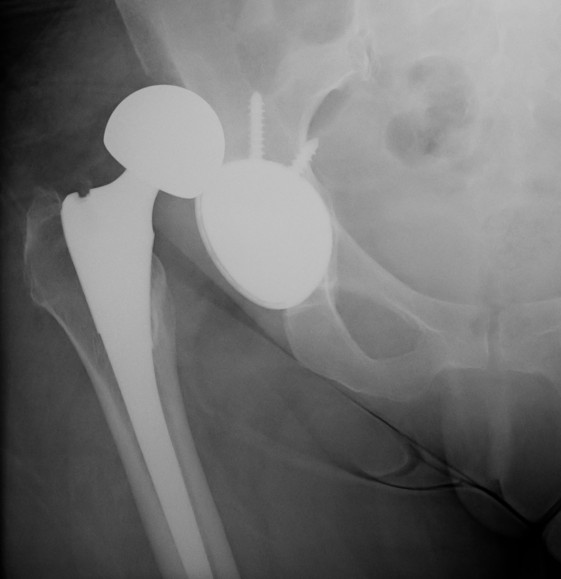
Posterior dislocation
- hip flexed, adducted, internally rotated
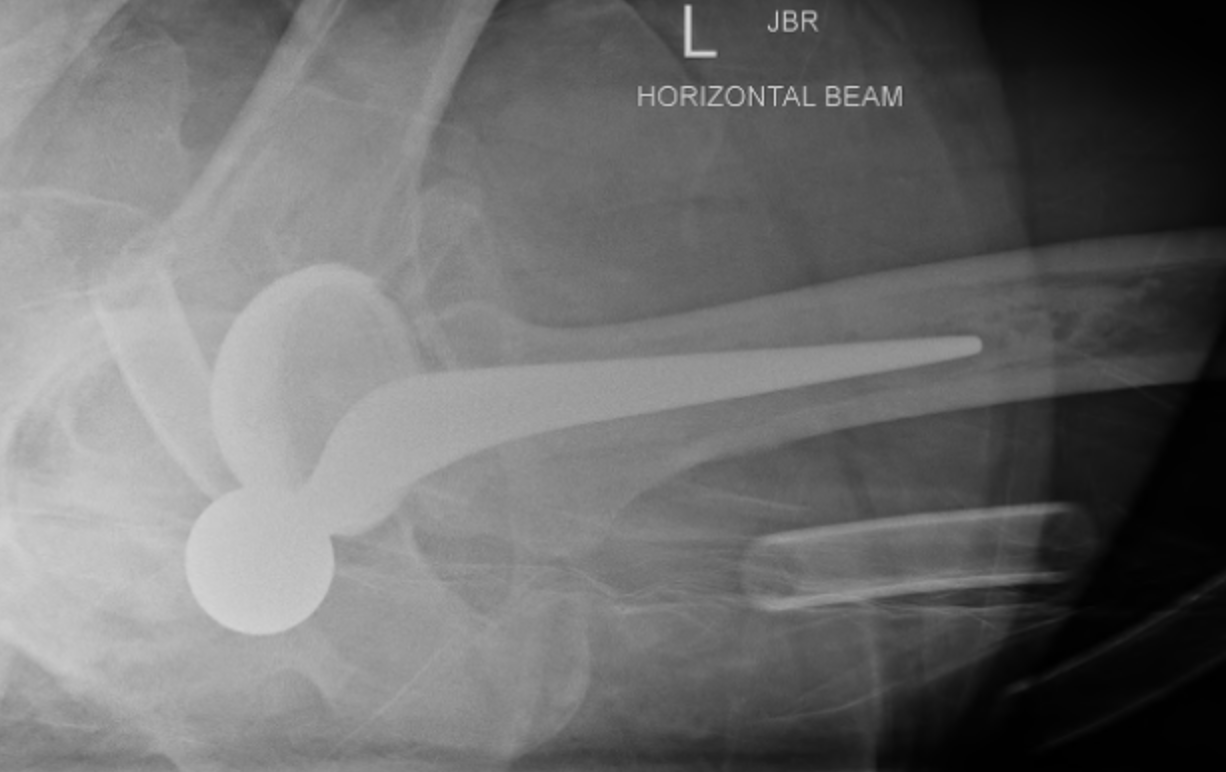
Posterior dislocation
Anterior dislocation
- hip extended, adducted, externally rotation
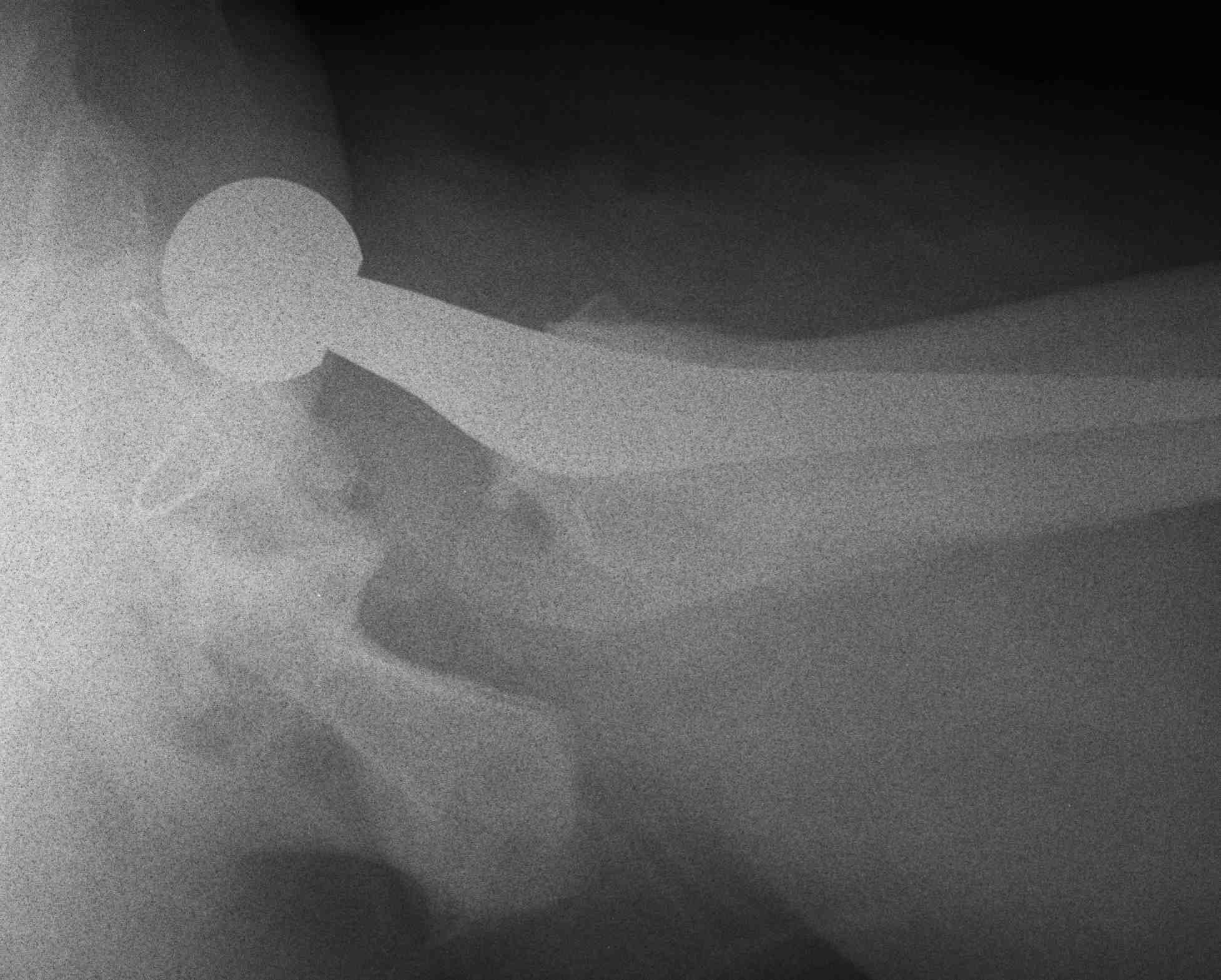
Anterior dislocation
