1. EUA
Compare both shoulders
- ROM
- anterior and posterior draw
- load and shift
- sulcus sign
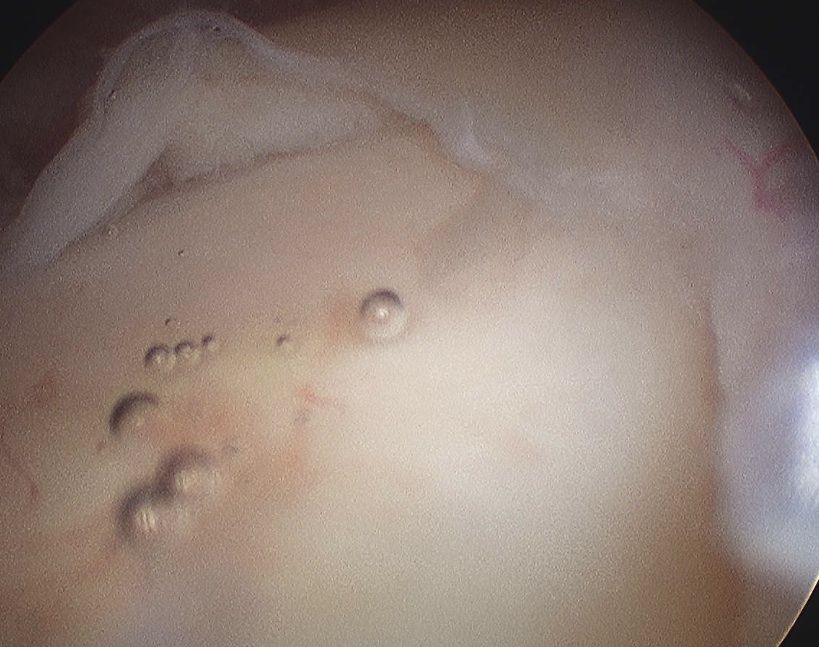
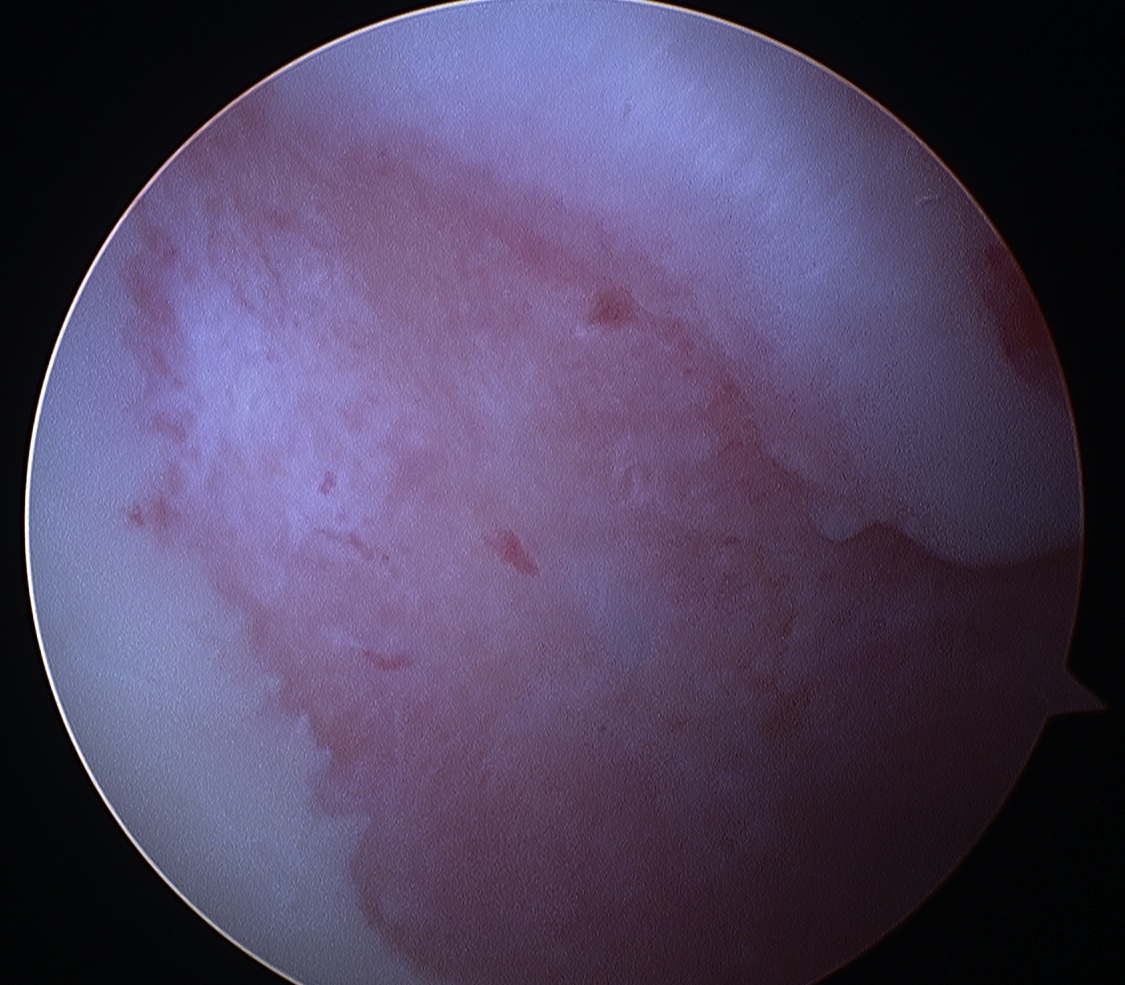
2. Labral Assessment
A. Above equator
Labral detachments here not uncommon
- degenerative tear in throwing athlete
- likely a SLAP constributes to instability
Beware normal variations in this area
Rao JBJS Am 2003
- variations in the antero-superior labrum
- found in 13% of patients
- 3 main types
1. Sublabral foramen


2. Sublabral foramen with cord like MGHL
3. Absence of AS labrum with cord like MGHL
- Buford complex
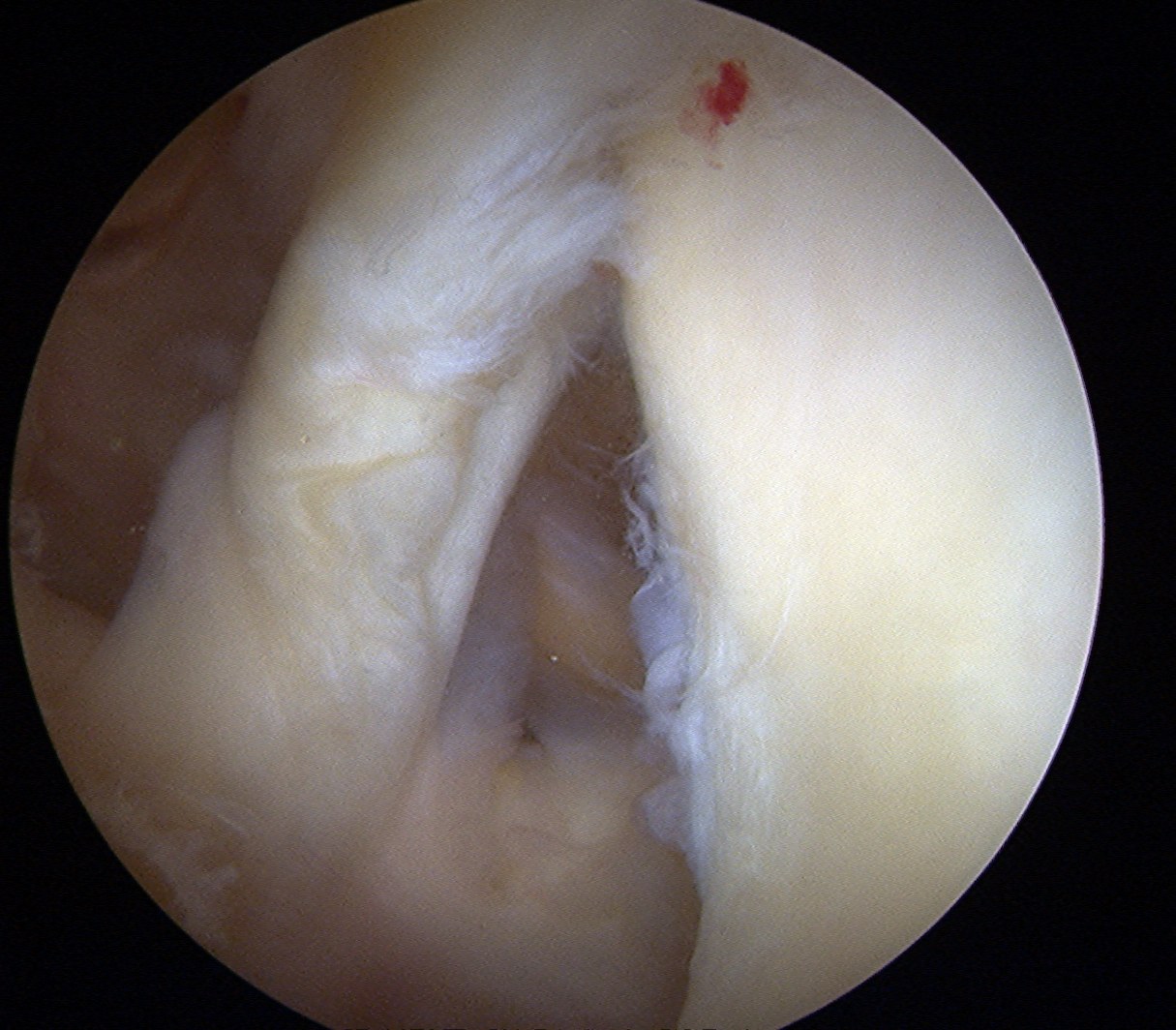
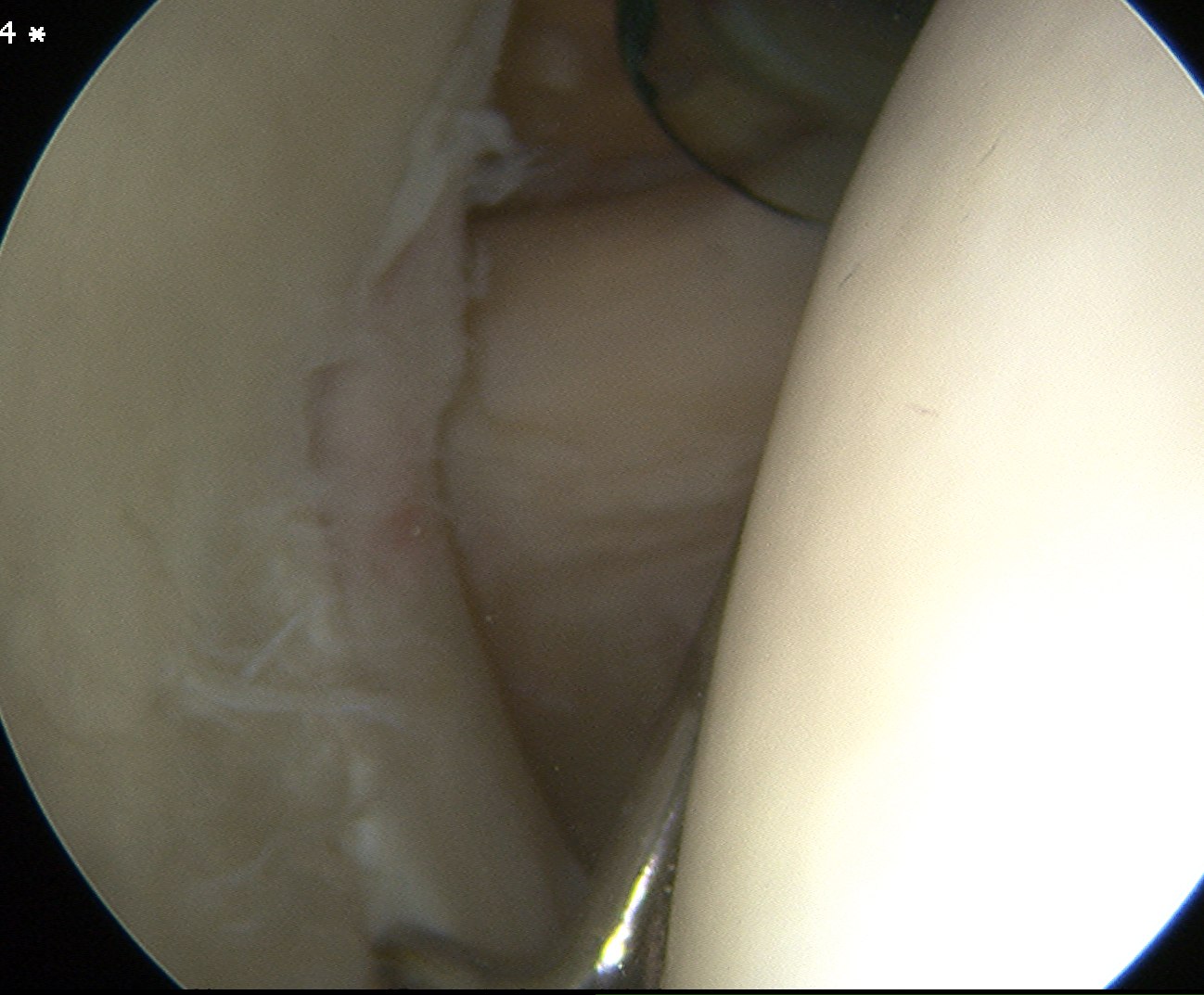
B. Below equator
Labral detachments / Bankart
- cause of instability
- 3 to 6 o'clock
- tear of anterior IGHL with labrum
- can be variants (ALPSA, GLAD, Perthes)
C. Exclude HAGL
Assess anterior IGHL attachment to humeral neck
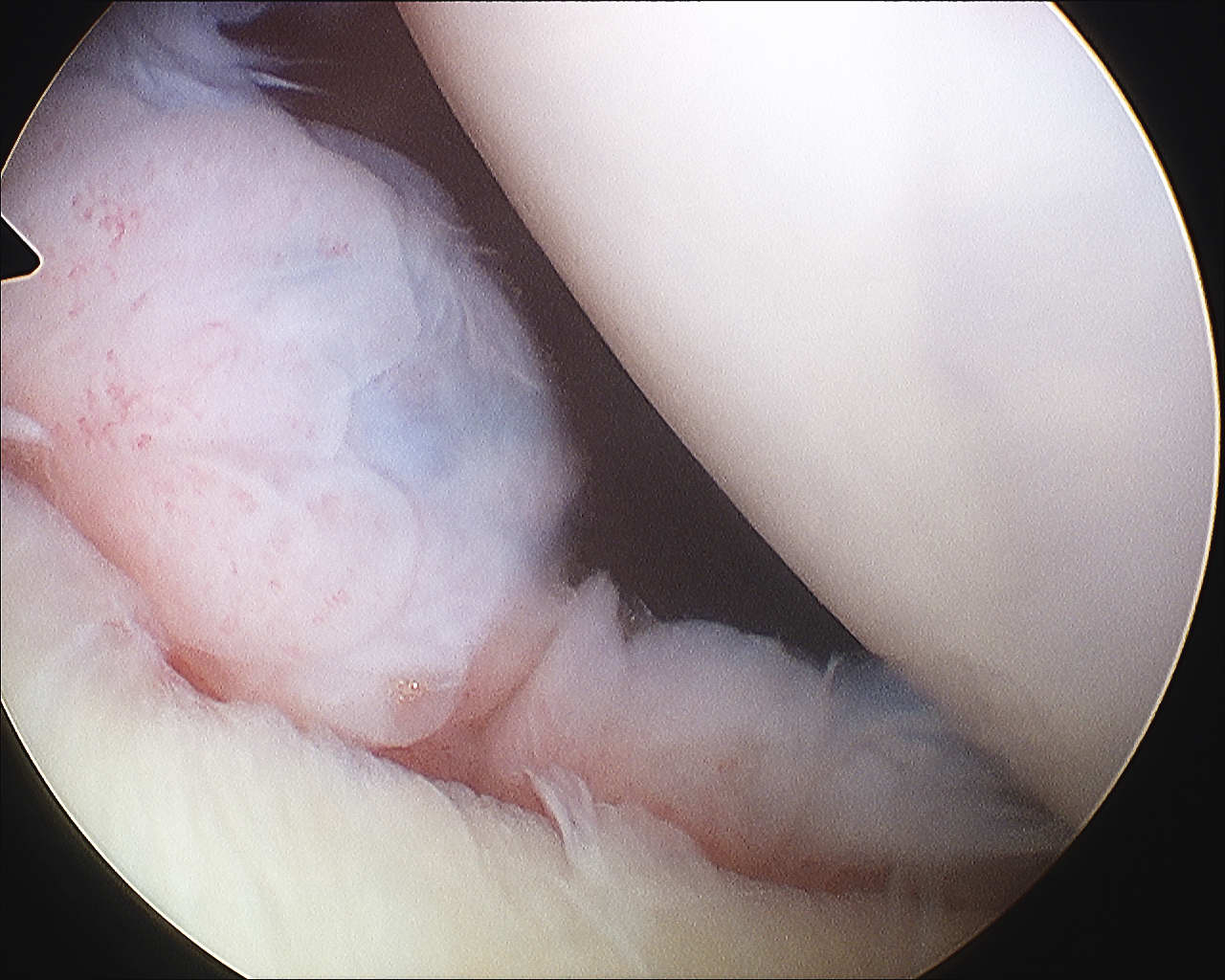
D. Posterior Labrum
Always assess
- place camera through anterior portal
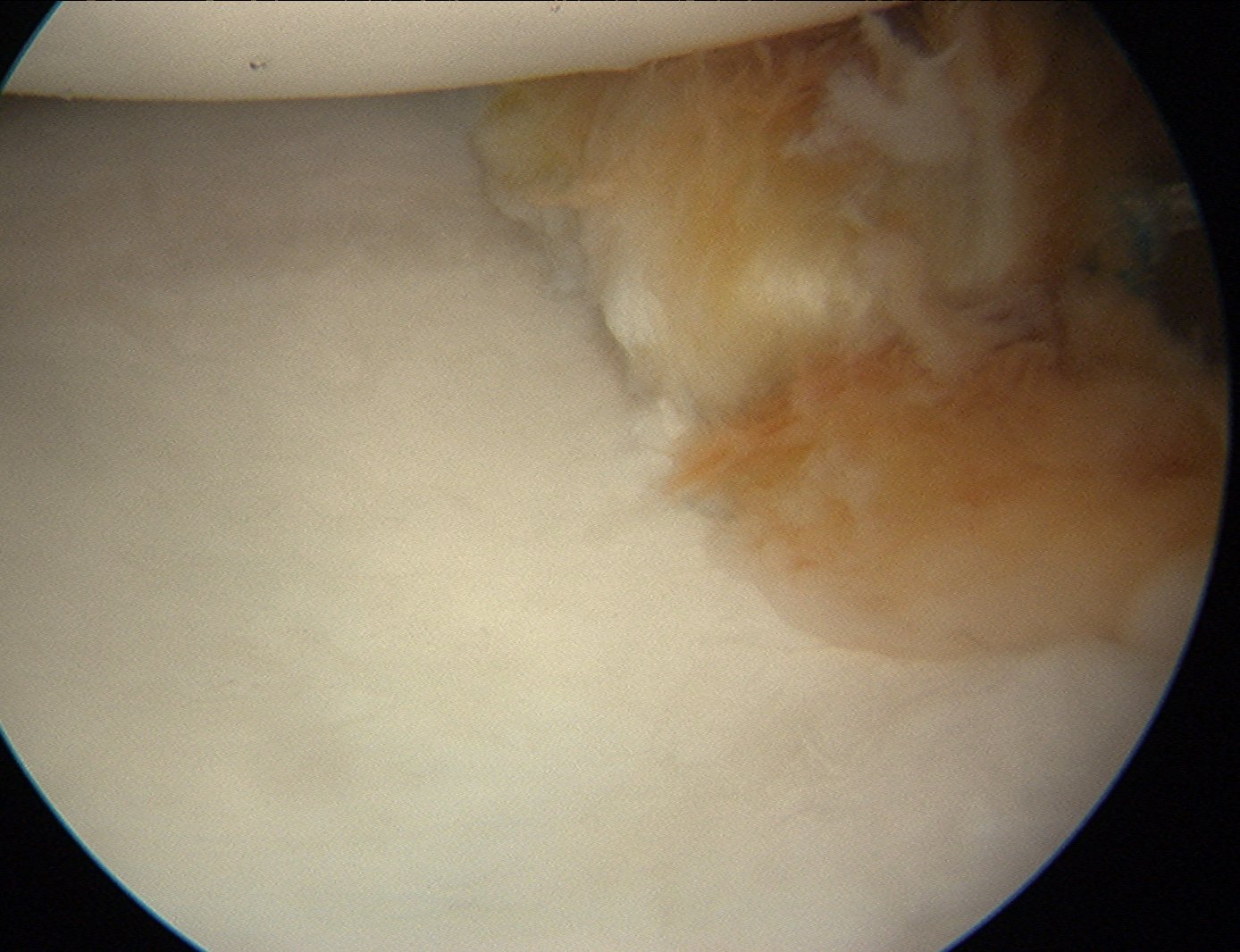
3. Bony Assessment
A. Anterior Glenoid
- measure bone anterior to bare area in centre of glenoid
- compare to bone posterior to bare area
- beware > 4 mm difference
- look for pear shaped glenoid
- is there sufficent bone for ST surgery alone?
Solution
- anterior bony procedure
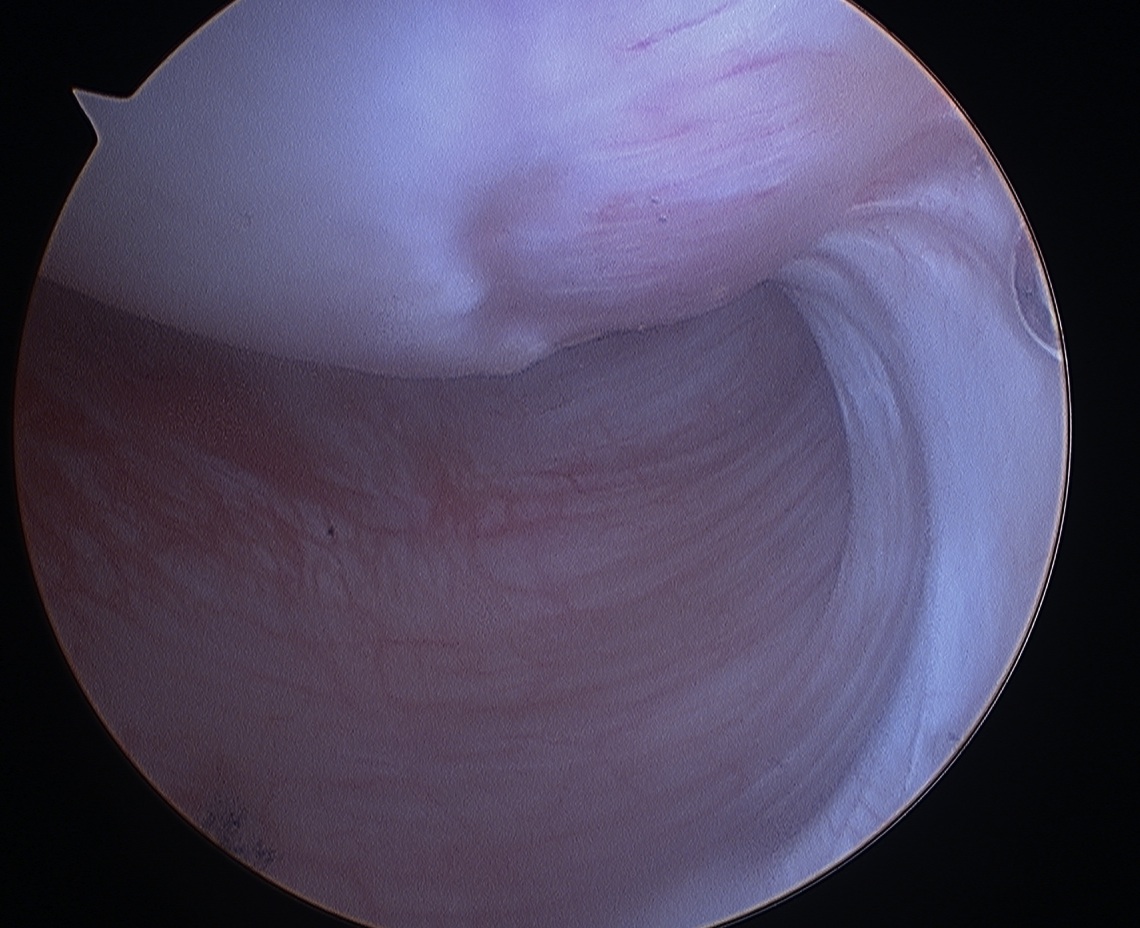
B. Hill Sachs
- posterolateral with anterior dislocation
- assess ER
- only a problem if engages with head centred and ER < 30 - 40o
Solution
1. Latarjet / Bristow
- ensures no engagement on anterior glenoid
2. Wolf Remplissage
- mobilisation of capsule and infraspinatous into Hill sach's
- renders defect extra-capsular
3. Humeral head allograft
4. Humeral head osteotomy
Technique Anterior Bankart Repair
Set up
Beachchair / lateral (surgeon preference)
Pressure pump
- usually less pressure required than subacromial work
- 40 mmHg
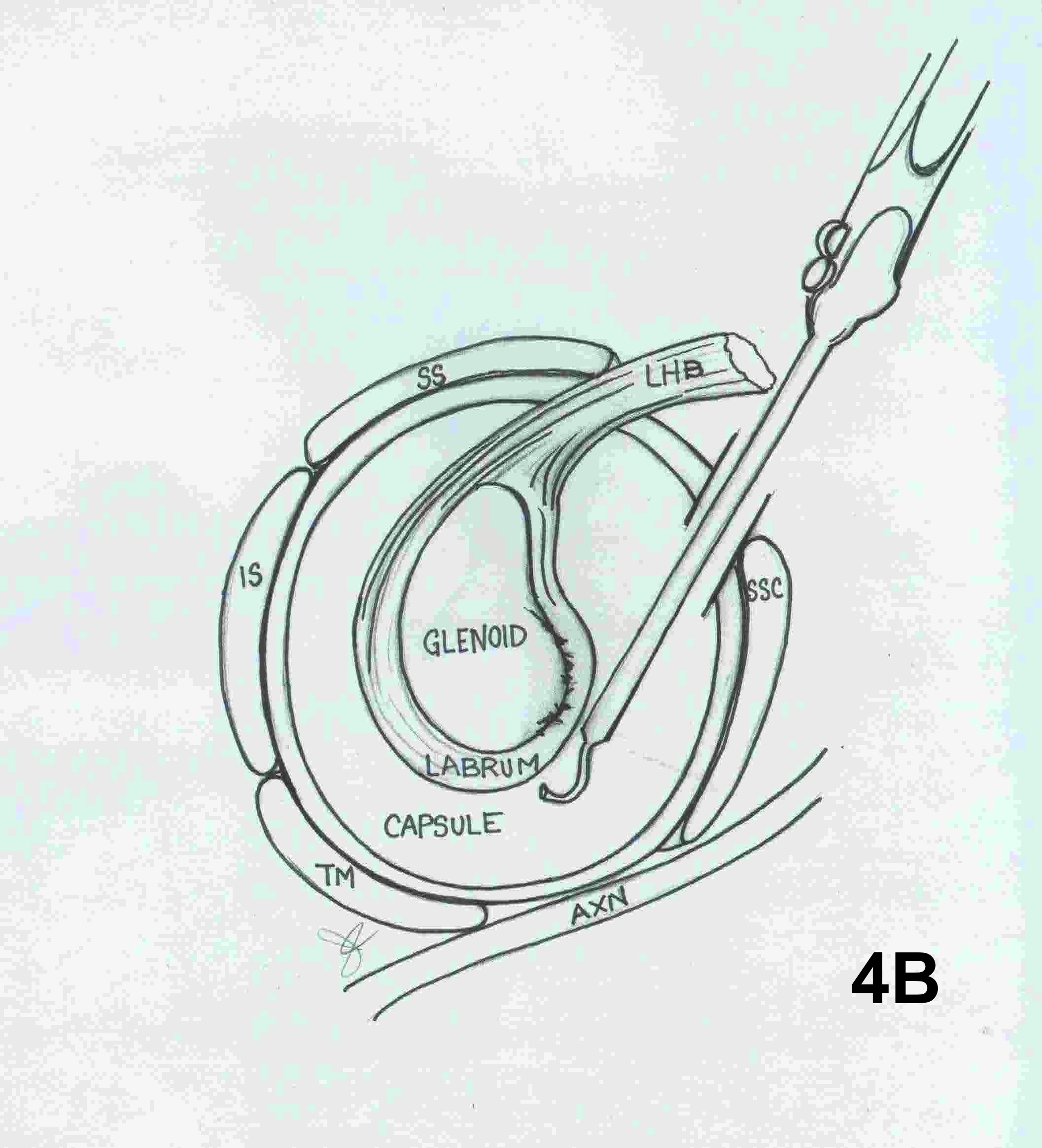
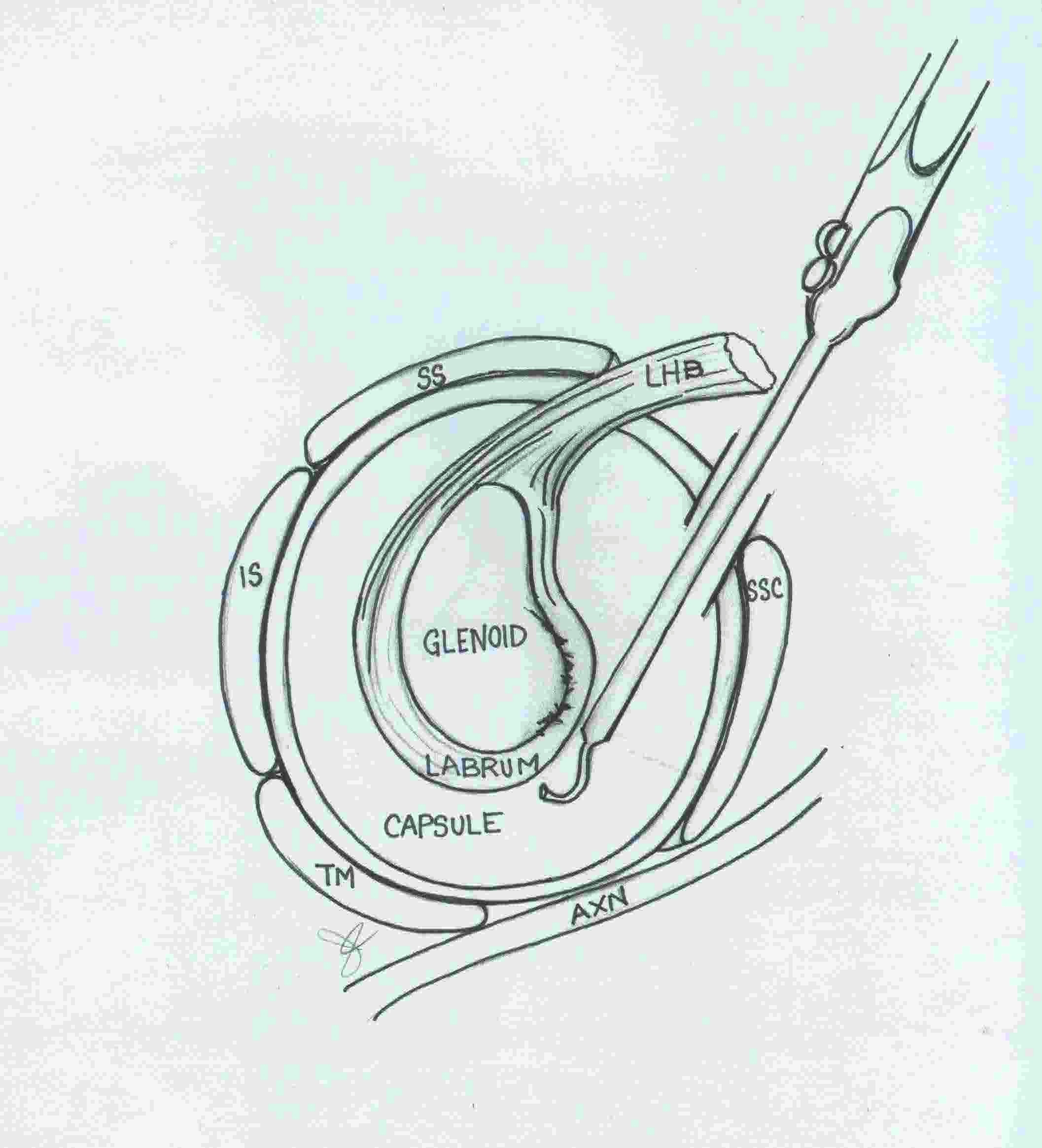
Portals
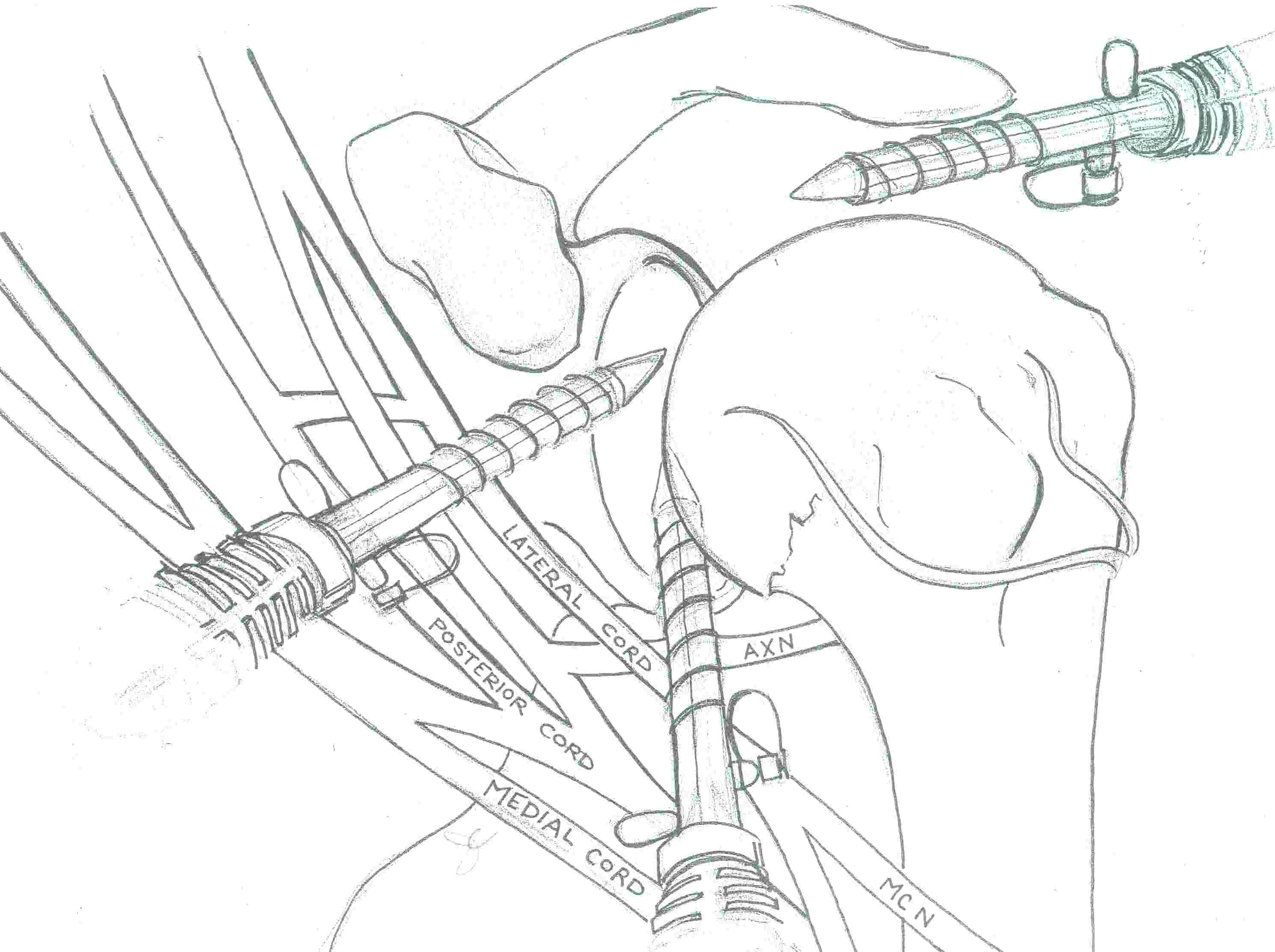
A. Standard posterior portal
- 2 cm below and 2 cm medial to PL acromion
- in soft spot
- good angle for GHJ work
B. Anteroinferior Portal (AI)
- for anchor placement
- rotator interval just above SSC
- 1 cm lateral to glenoid
- establish with spinal needle
- need to access 3 - 6 o'clock
- 8 mm portal
Anterosuperior Portal (AS)
- for suture management
- 1 cm superior and 5 mm lateral
- spinal needle
- enters rotator interval at angle between biceps and glenoid
- 8 mm cannula

Problem
- can make rotator interval very crowded
- repair can be done through single portal
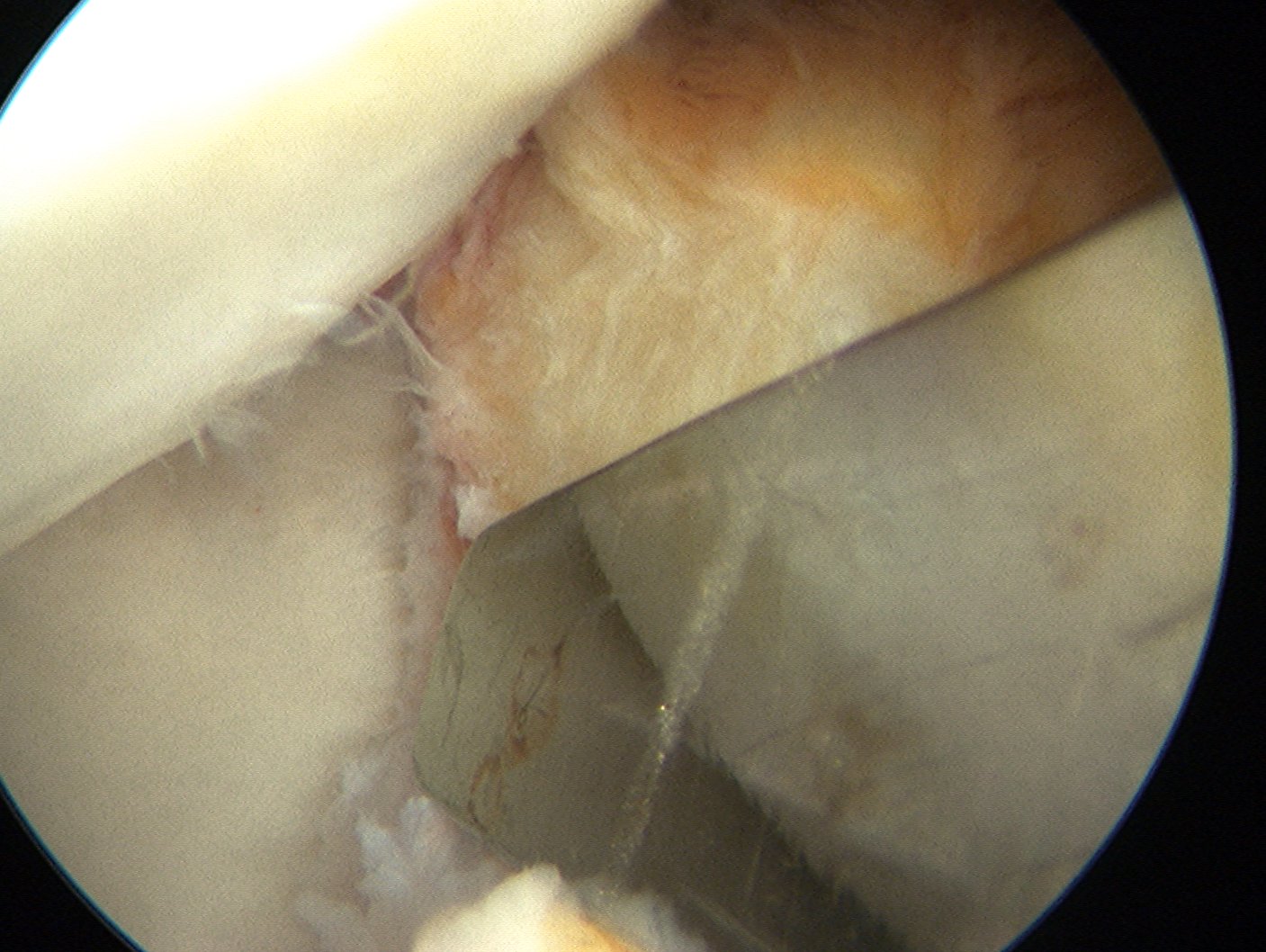
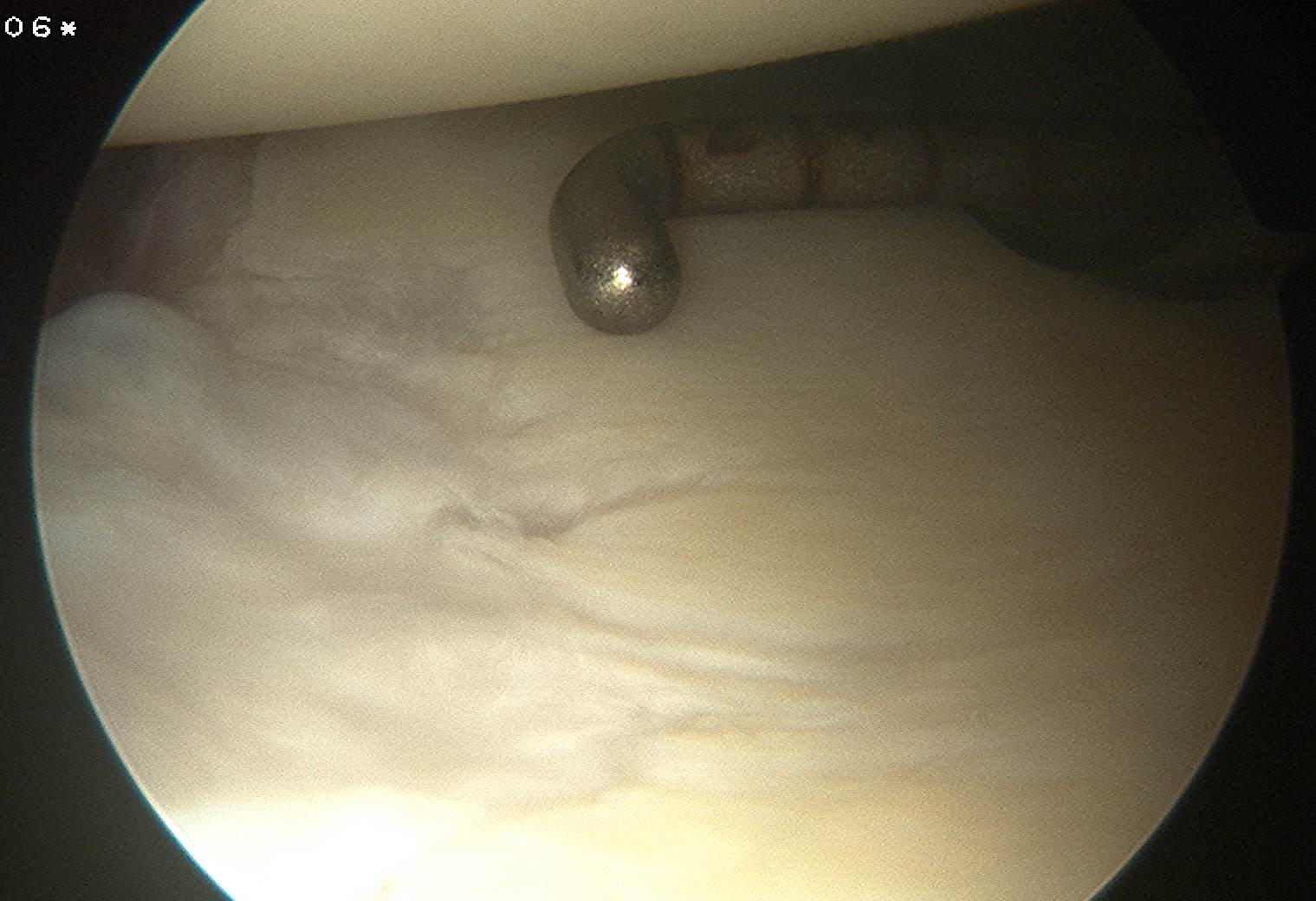
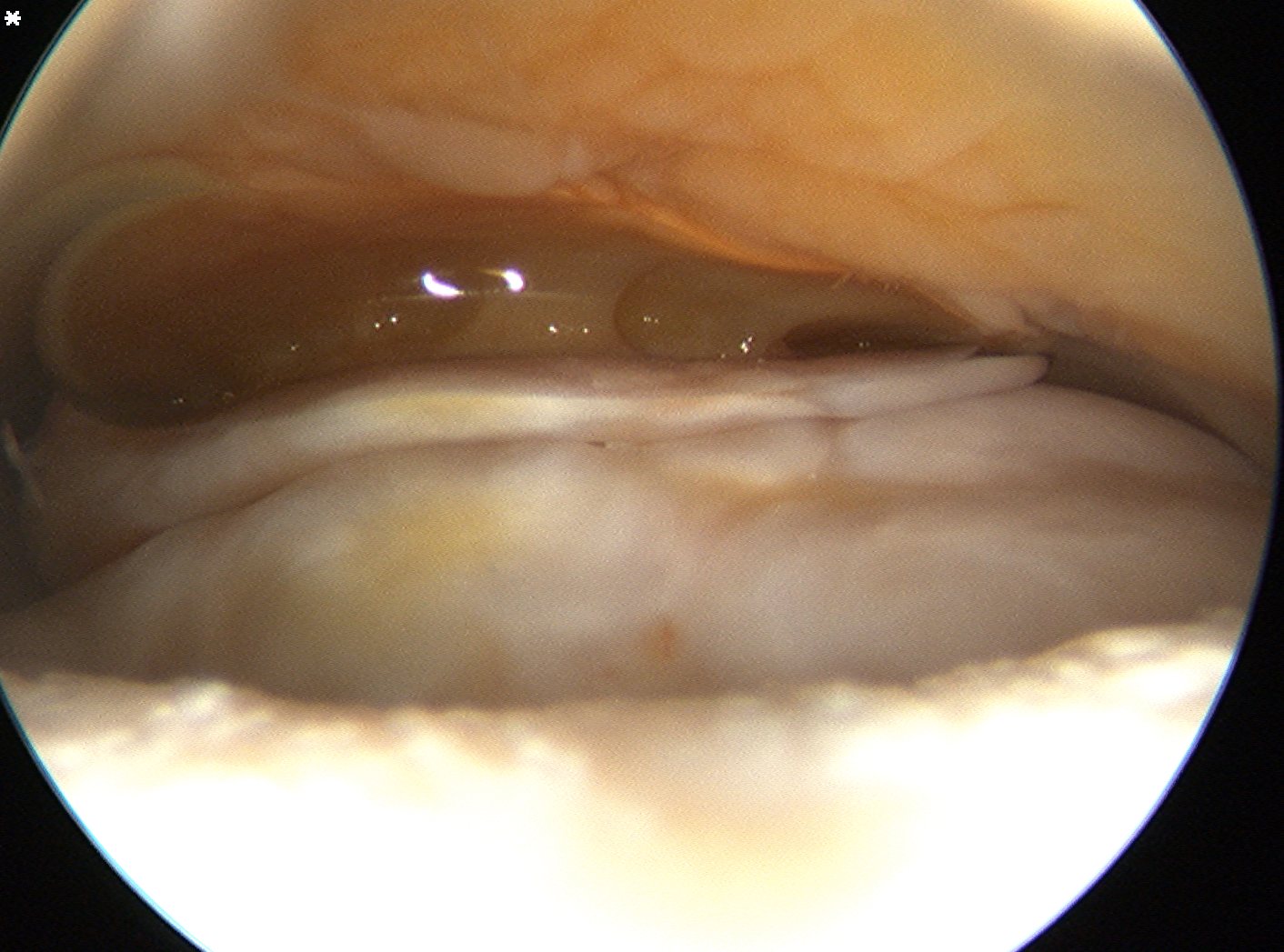
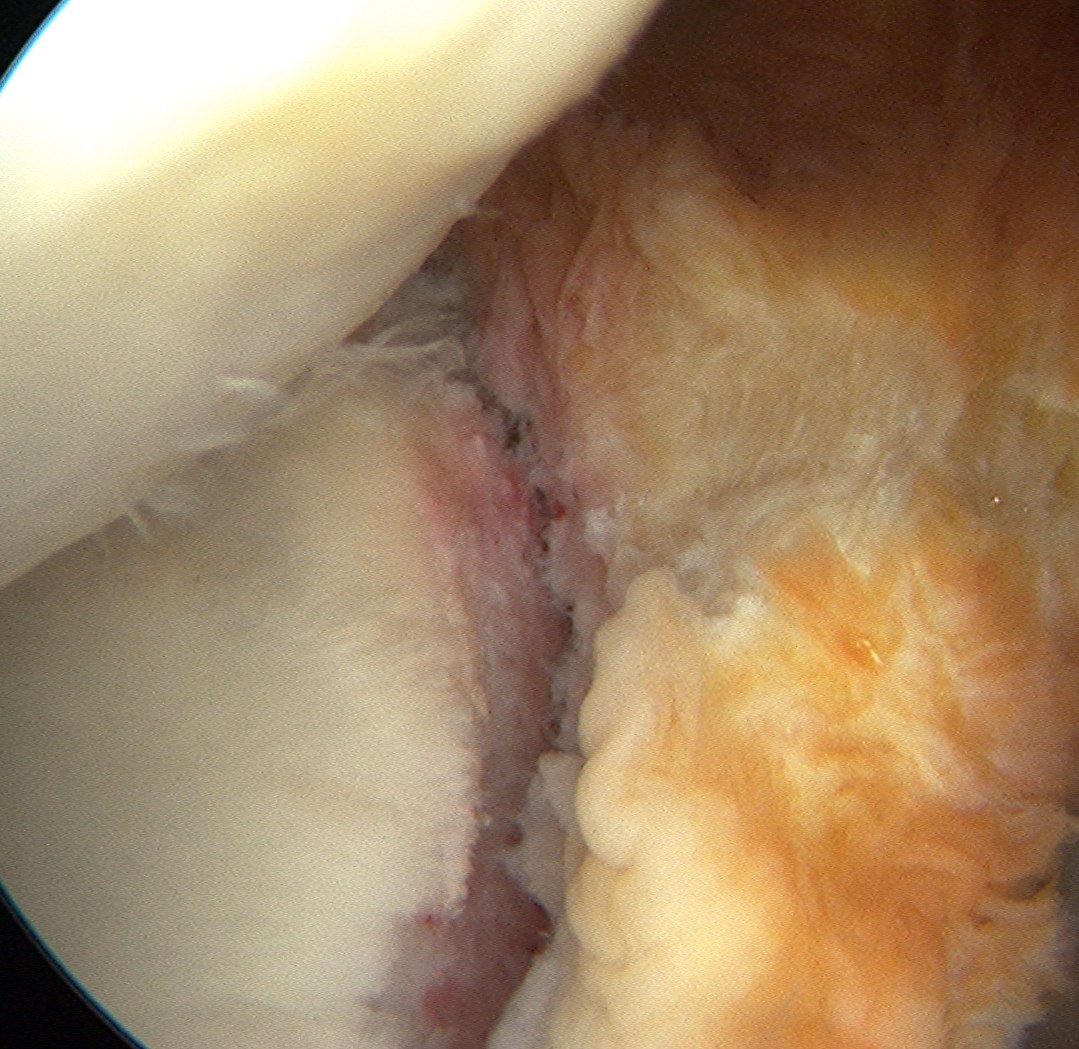
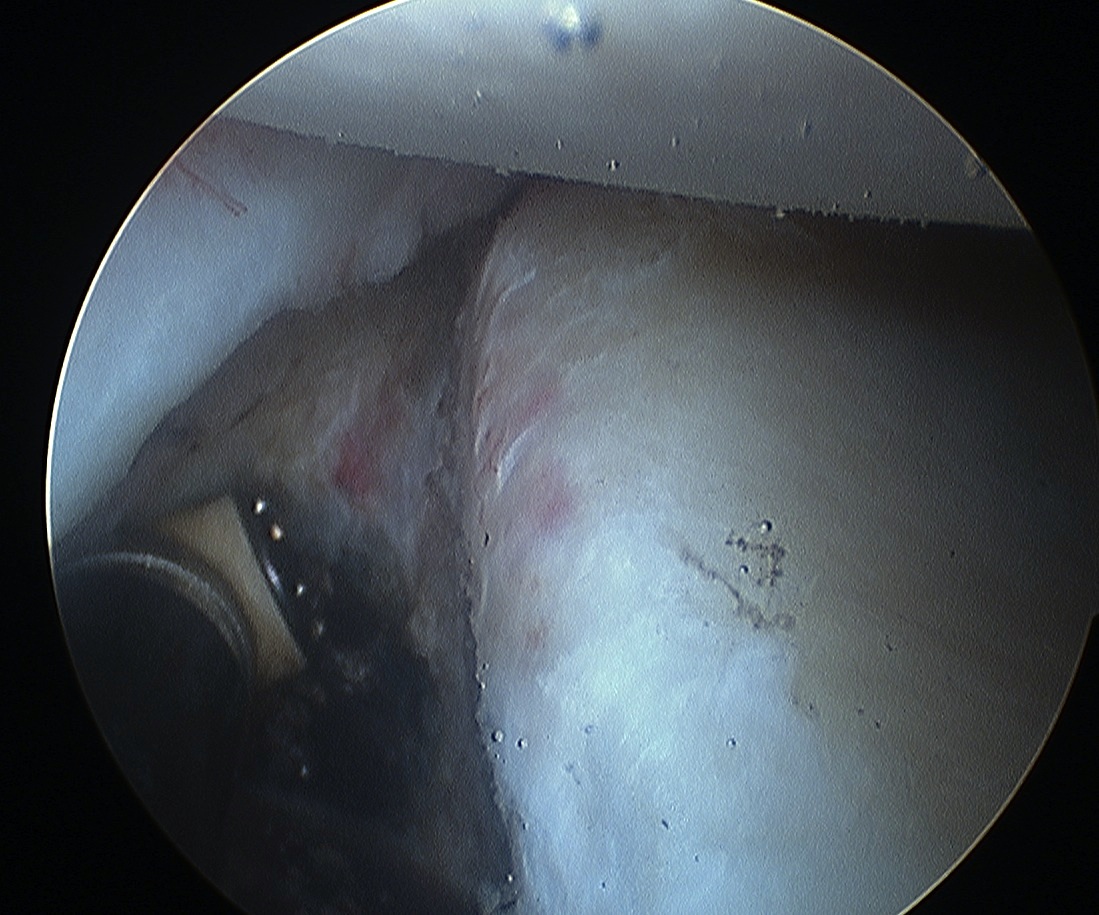
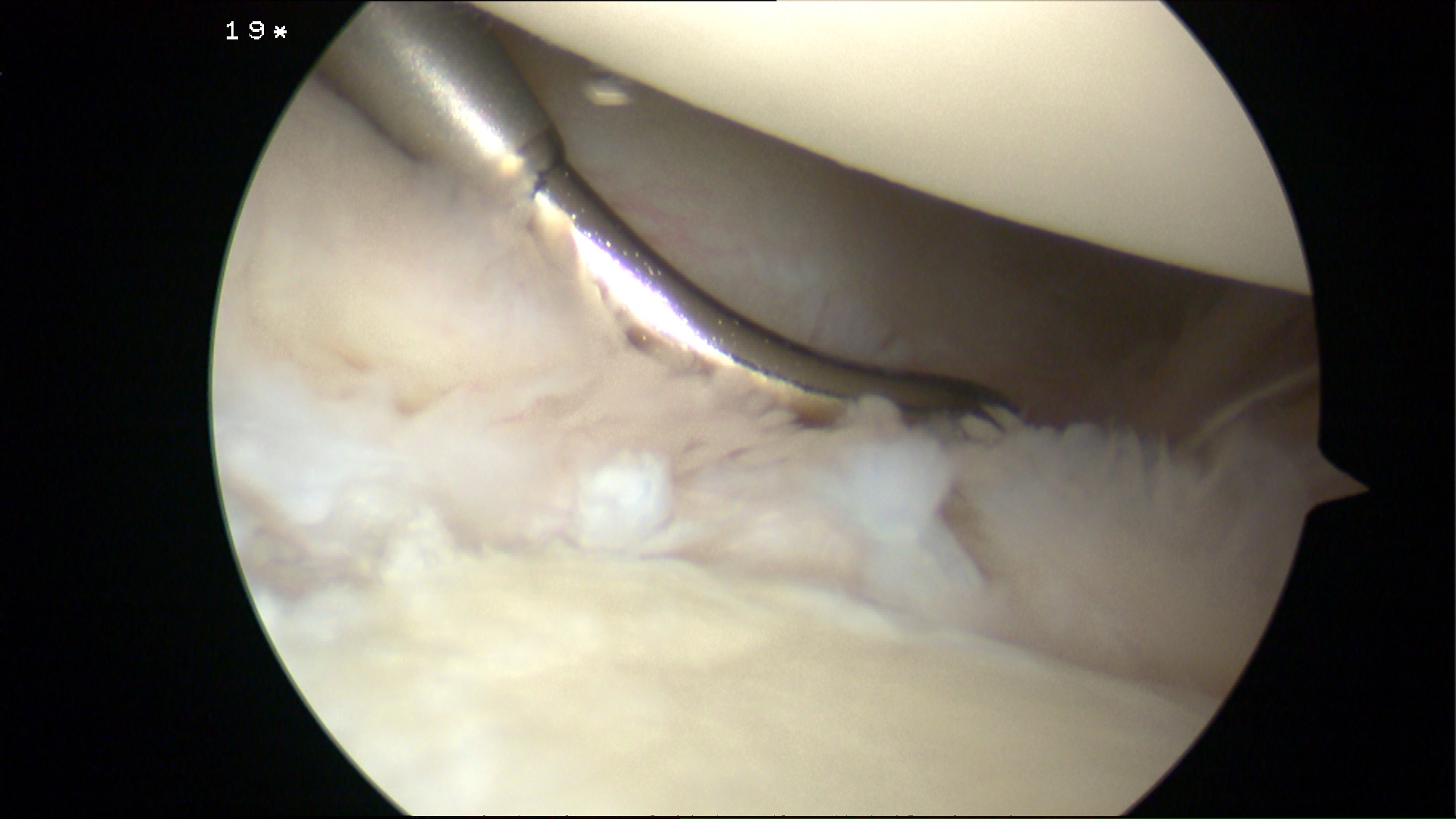
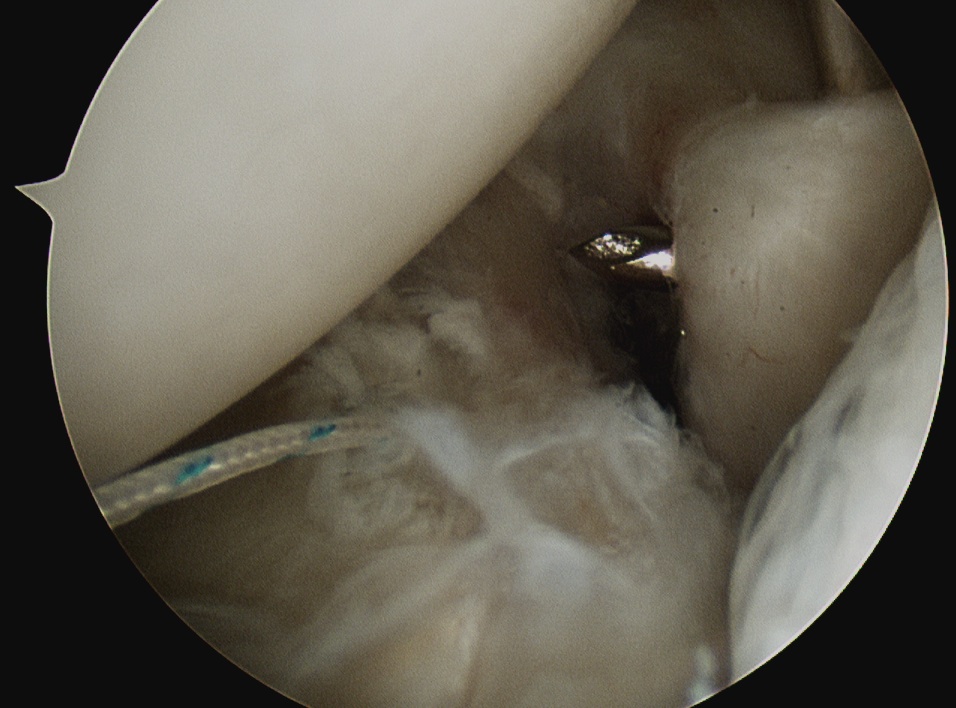
Mobilise labrum
Labral mobiliser / rasp / scissors
- labral tear can be obvious, but may have partially healed or healed medially
- mobilise until can see SSC muscle underneath
- change camera to ASL portal for better view
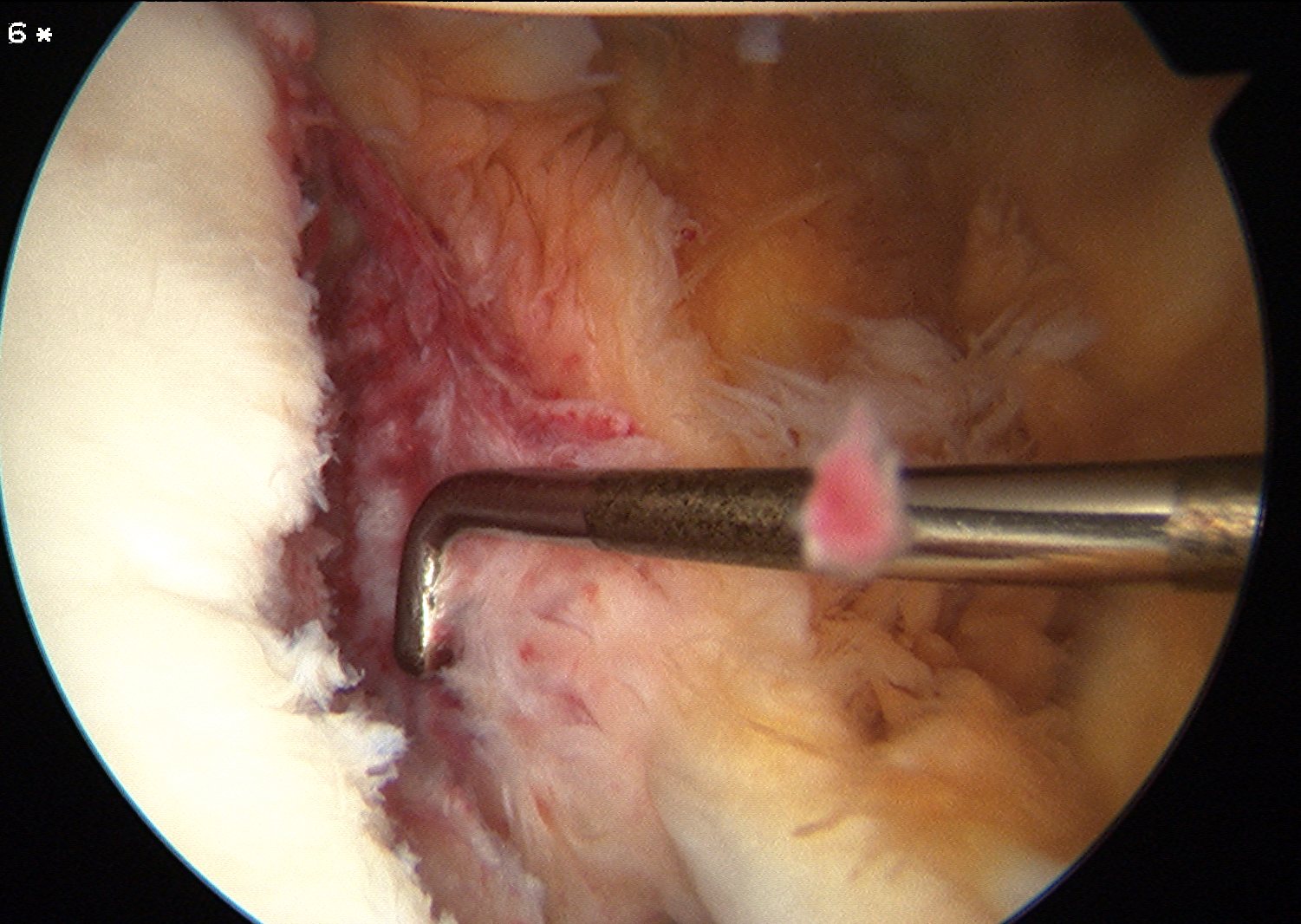
Bony Fragments
- important to recognise
Options
1. Incorporate in repair
- pass sutures medially to bony fragments
2. Remove / debride
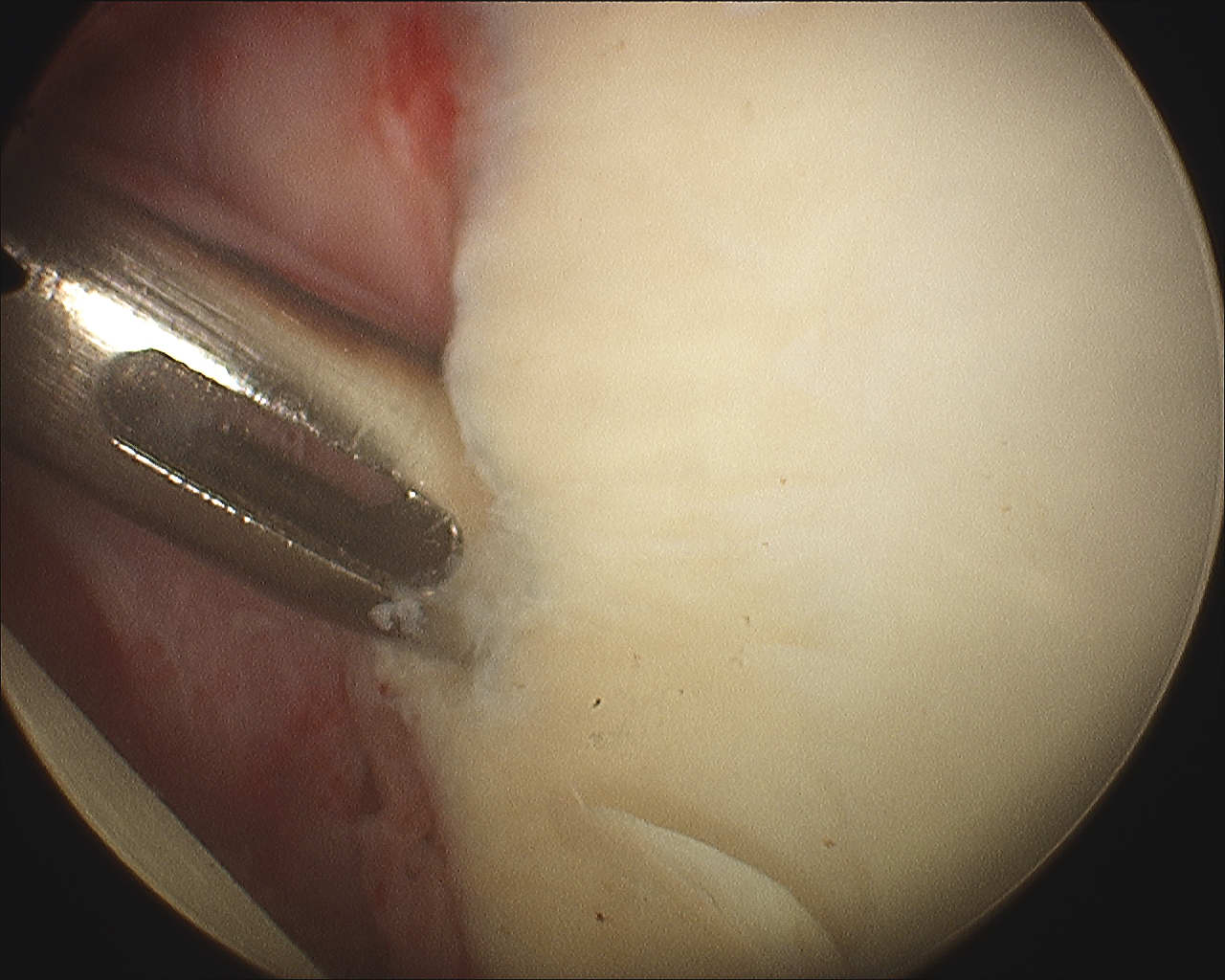
Debride bone to bleeding base
- tear is from 3 to 6 o'clock
- use shavers / burrs
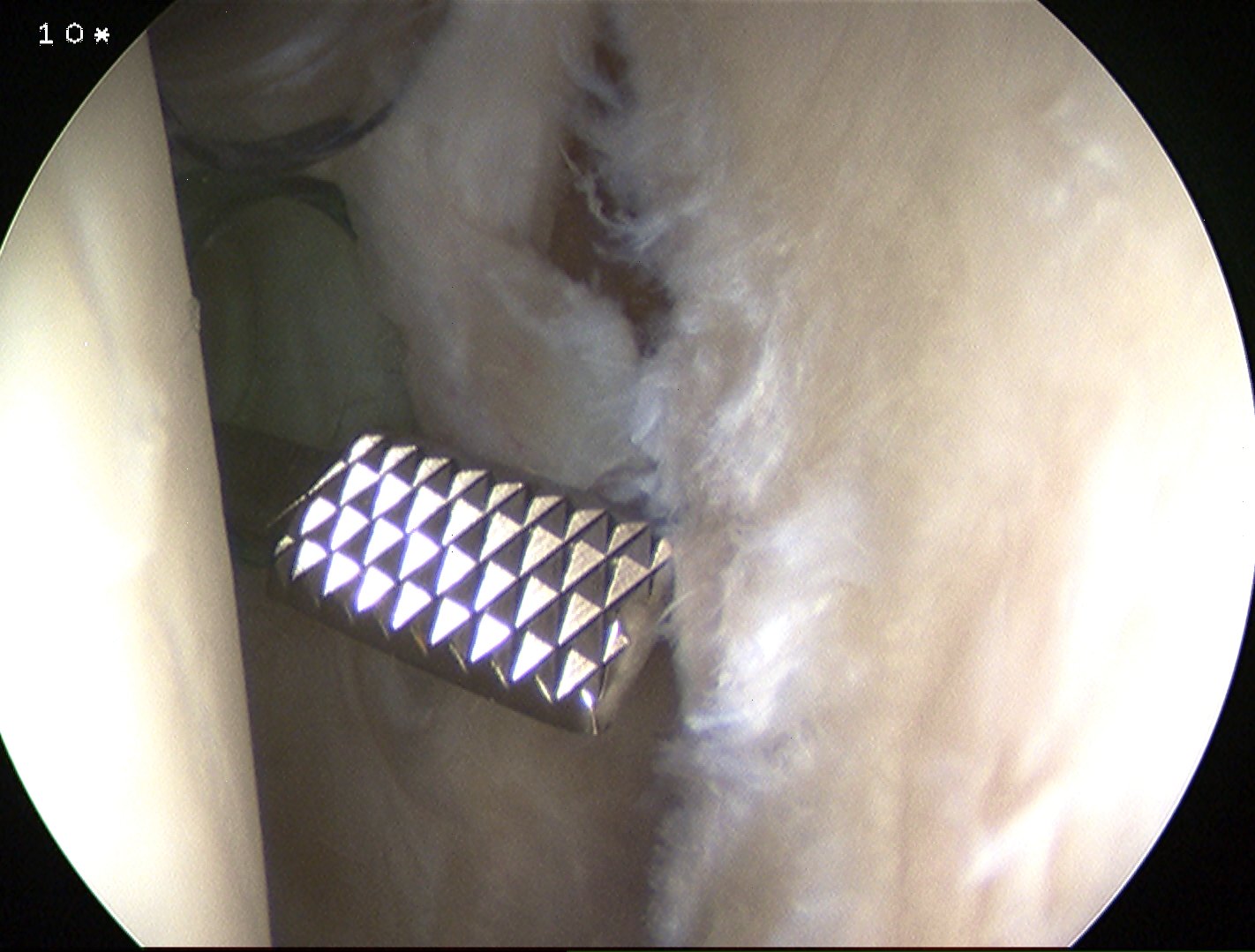
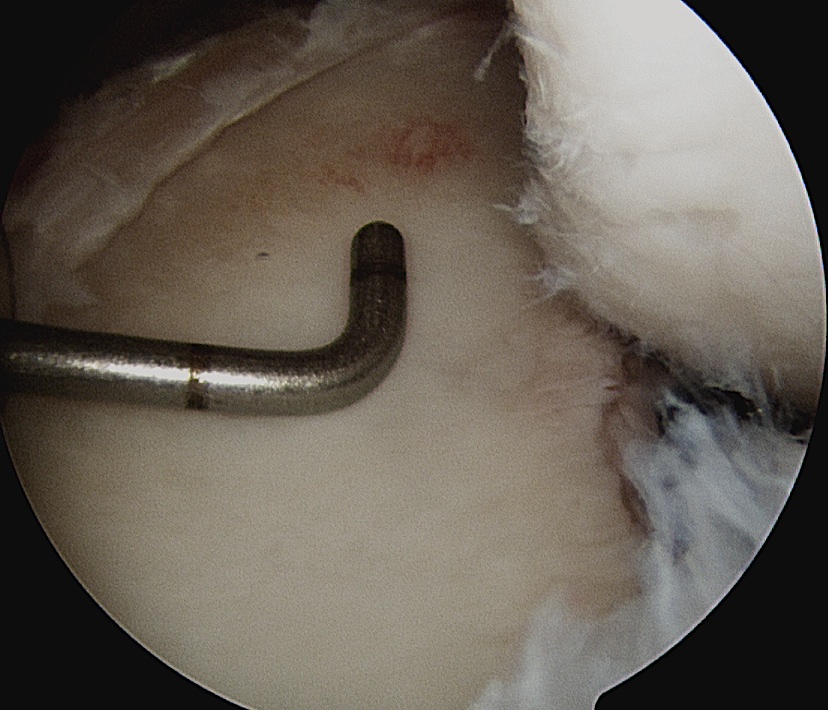
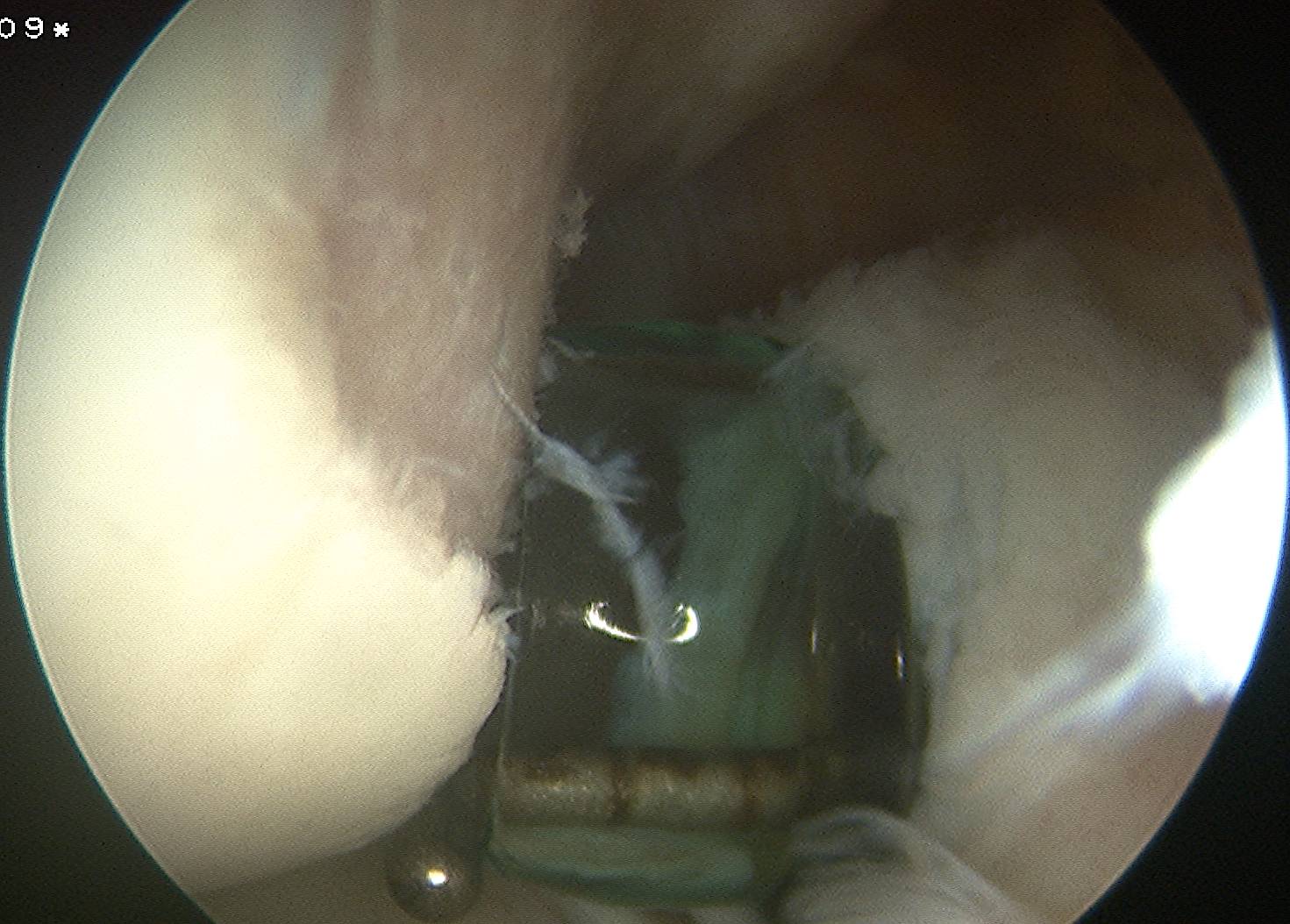
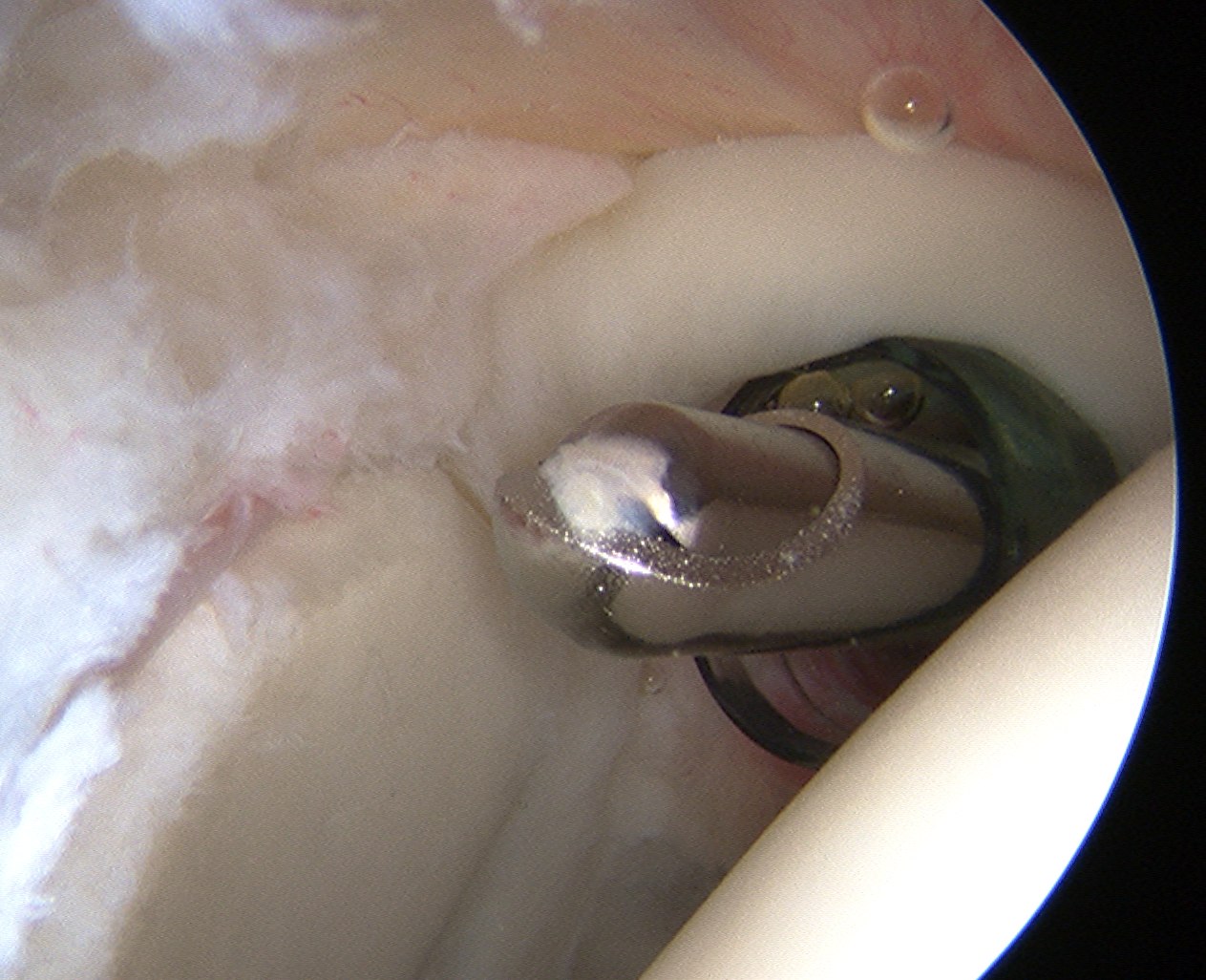
Labral Repair
Anchors
- 2.3 or 3.2 mm bioabsorbably anchors
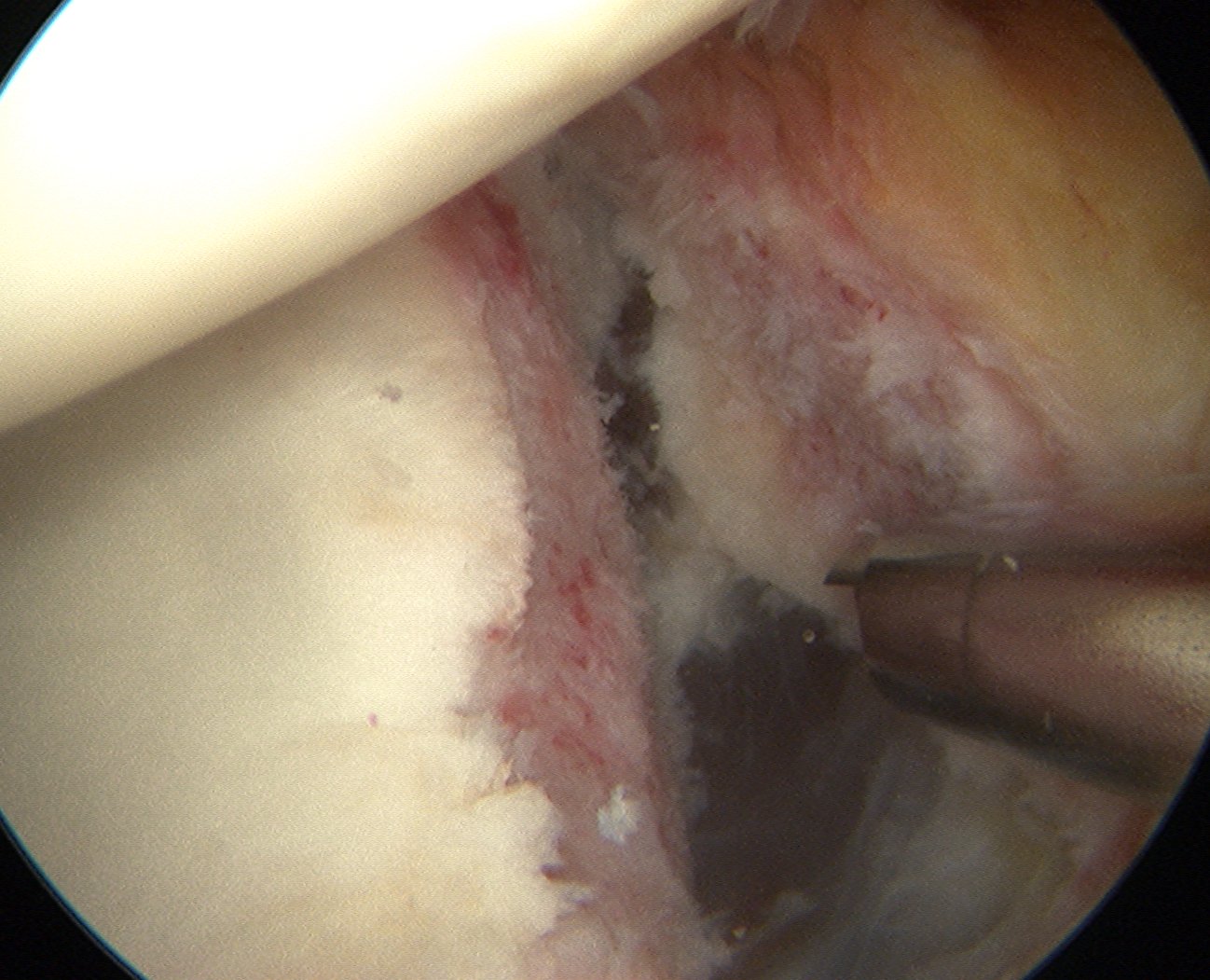
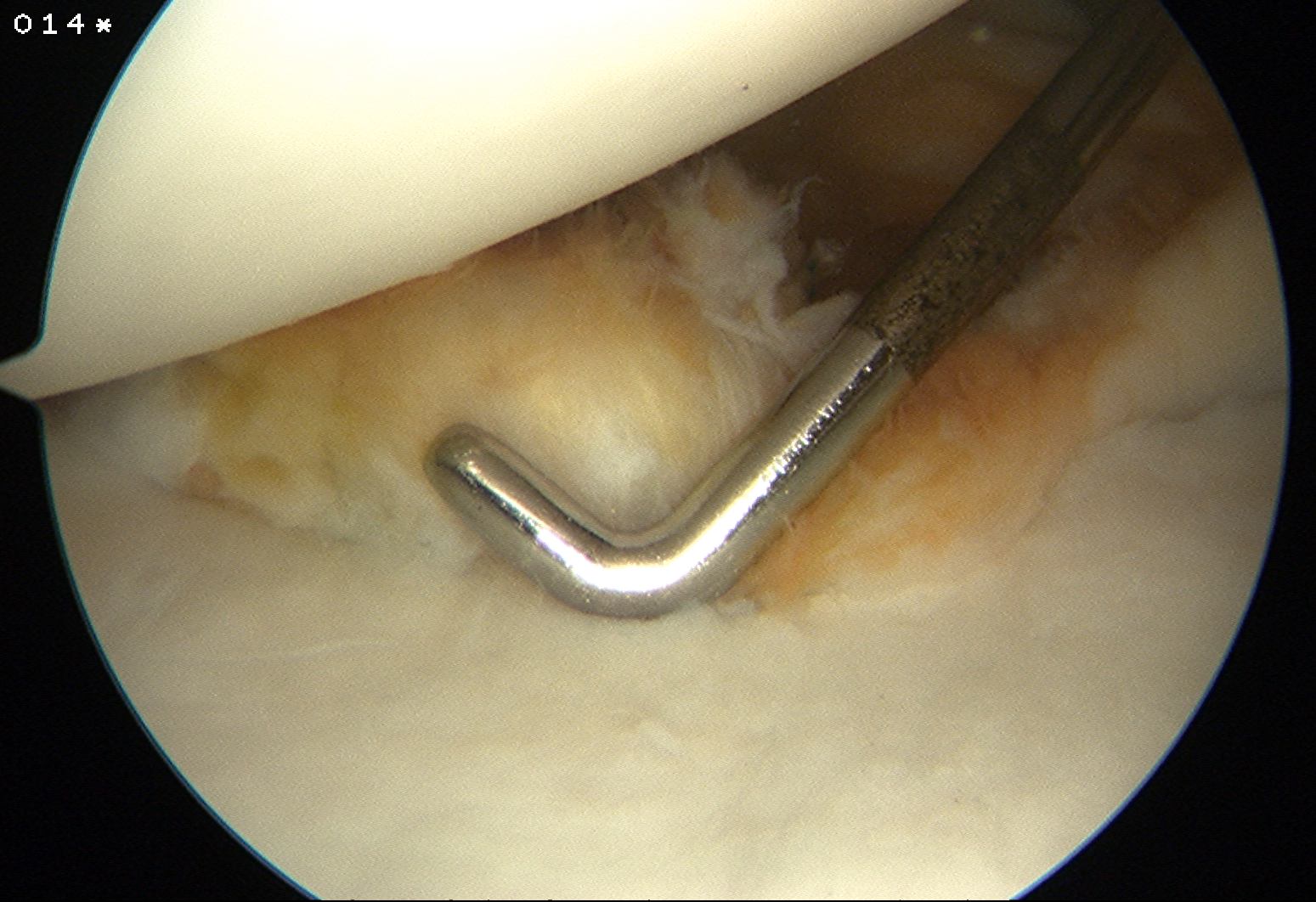
Insert inferior anchor
- most difficult and most important
- via anteriorinferior portal or via stab incision in SSC
- on anterior edge of glenoid cartilage
- want to recreate bumper effect
- inferior anchor first at 5.30
- insert drill guide, pass drill, insert anchor
- usefull to have assistant distract head laterally at this point
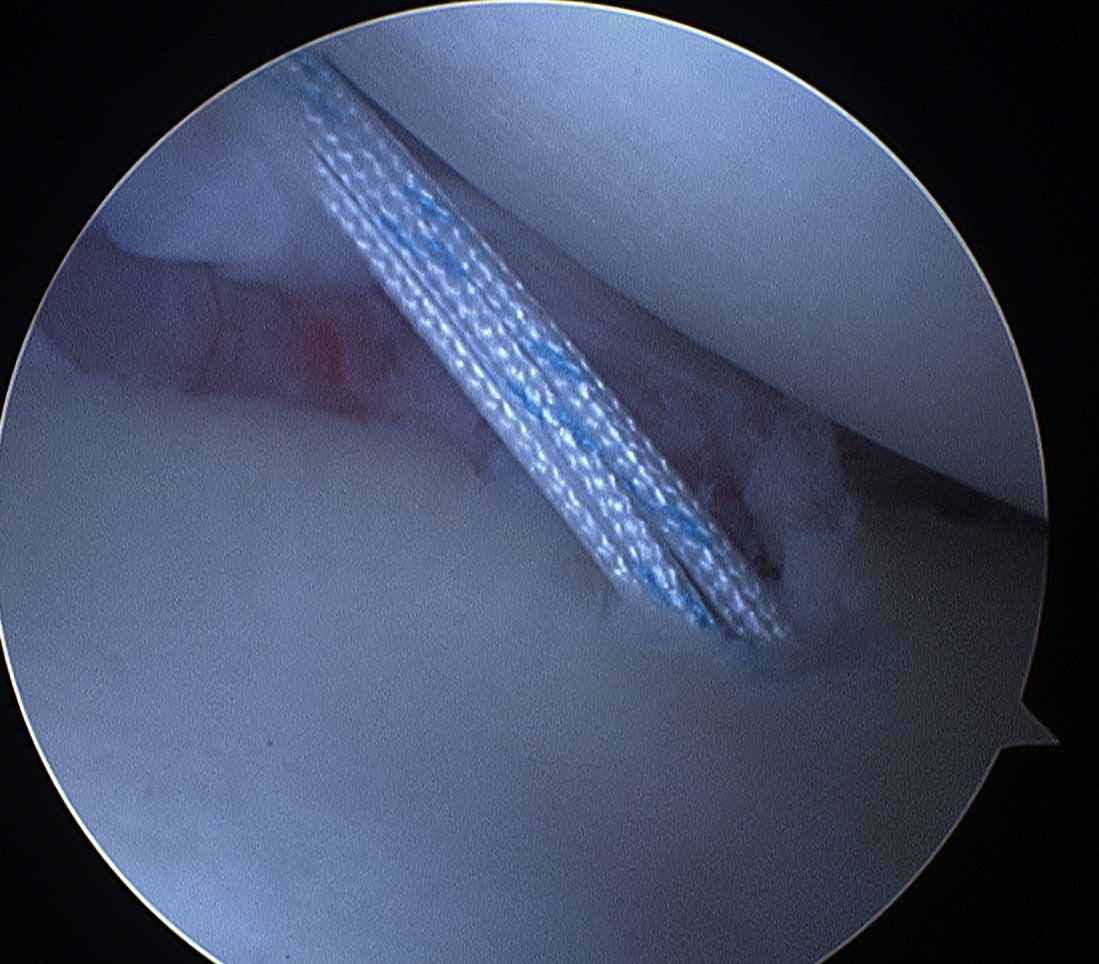
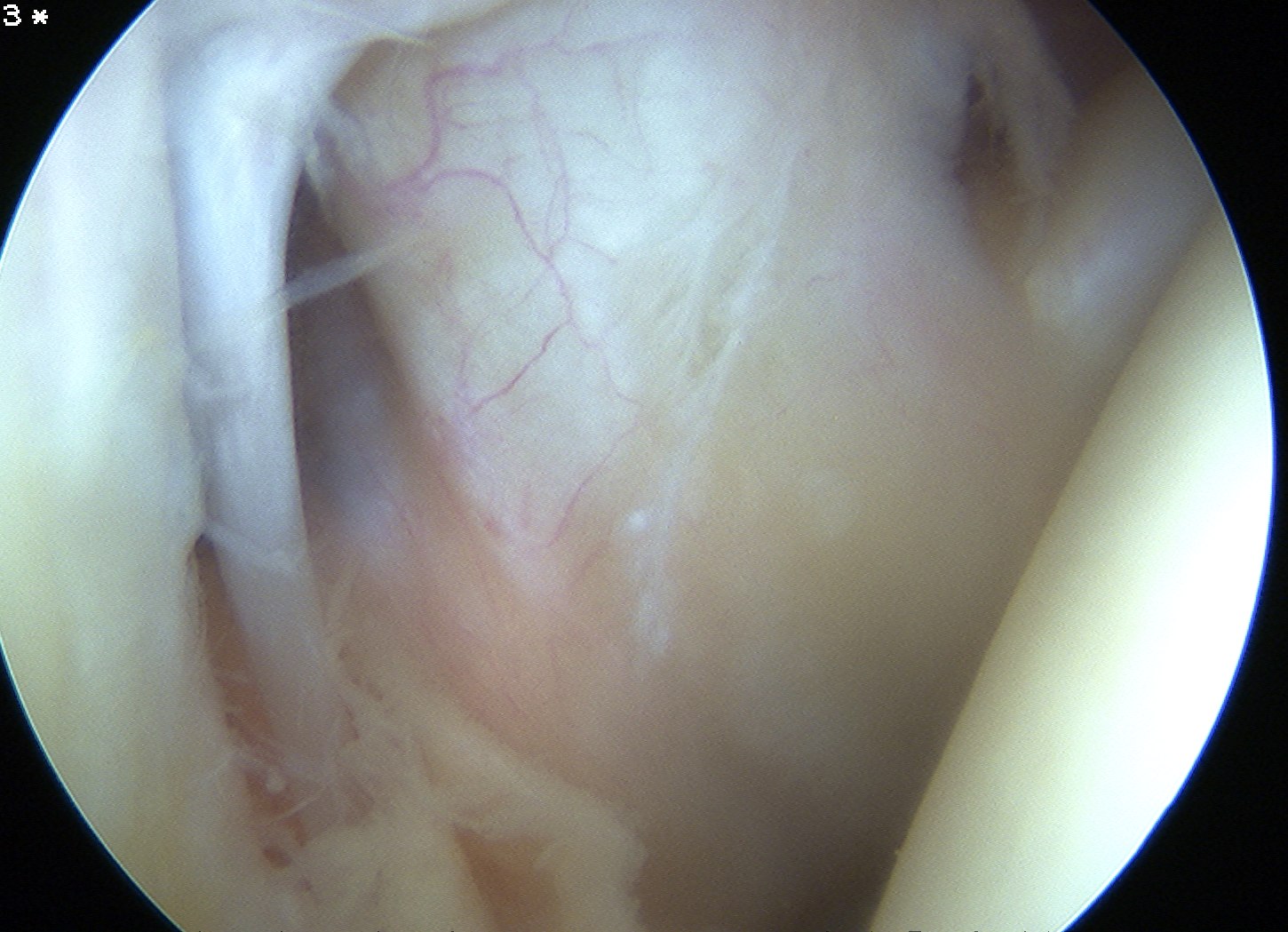
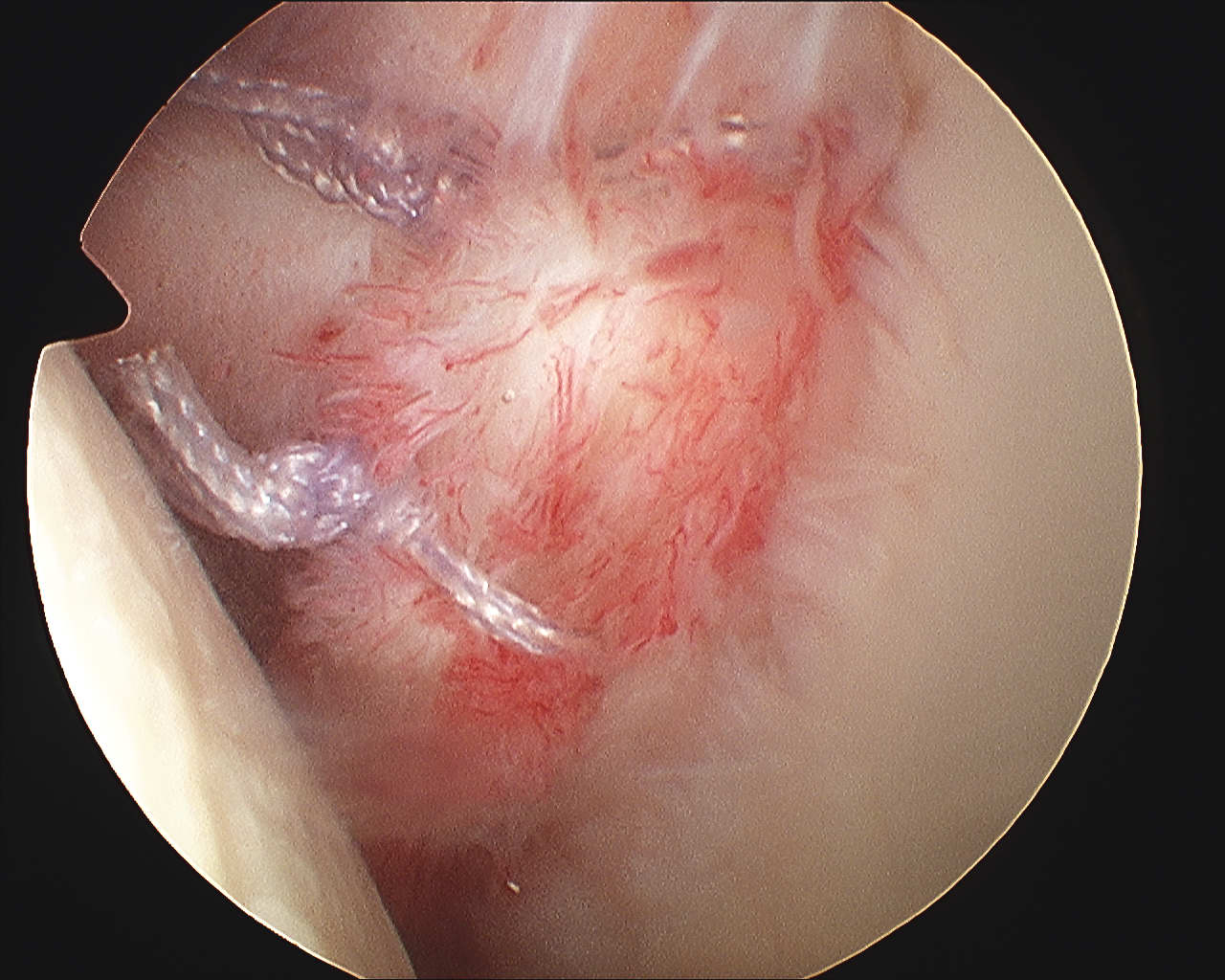
Suture passer
- again, assistant distracts shoulder
- right angled for right shoulder, left angled for left
- via the AI portal
- decide whether to take labrum only or capsule then labrum
- want to pull tissue superiorly and laterally
- suture passer with loop / single nylon in anterior to posterior direction
- retrieve through portal
- retrieve suture posterior to anterior through portal
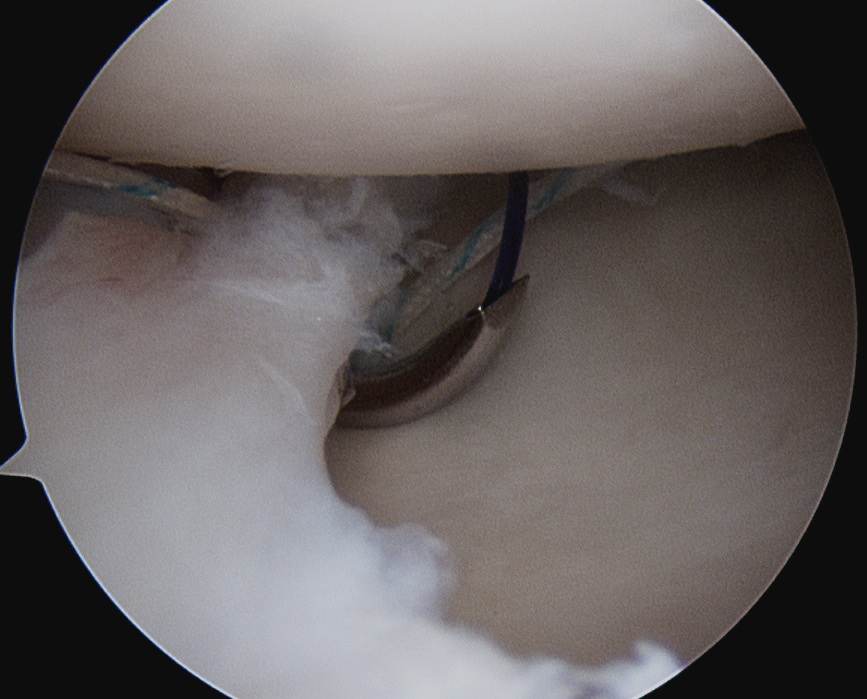
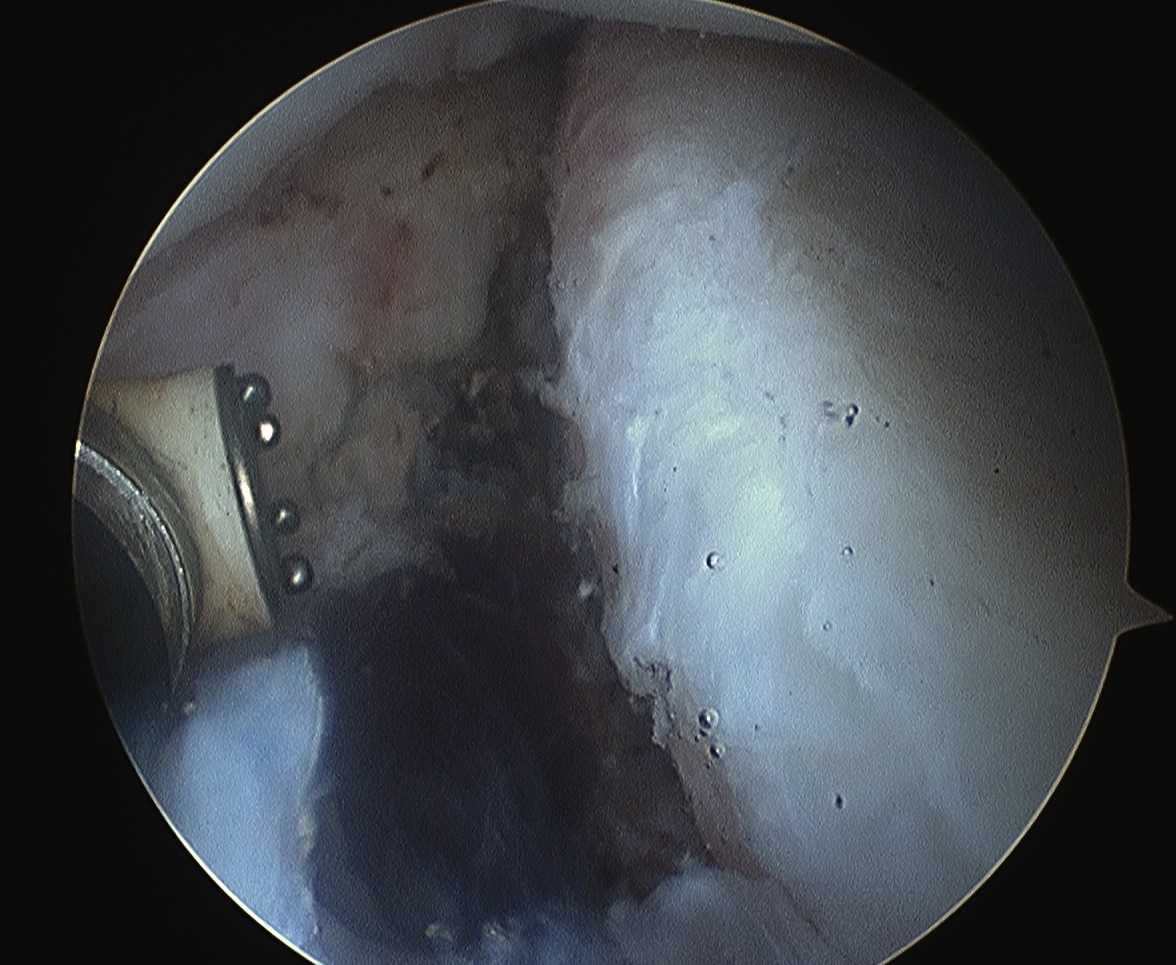
Tie knot
- simple knot / Duncan Ely / Modified Roeder
- ensure post / subsequent knot is anterior to labrum
- recreate bumper effect
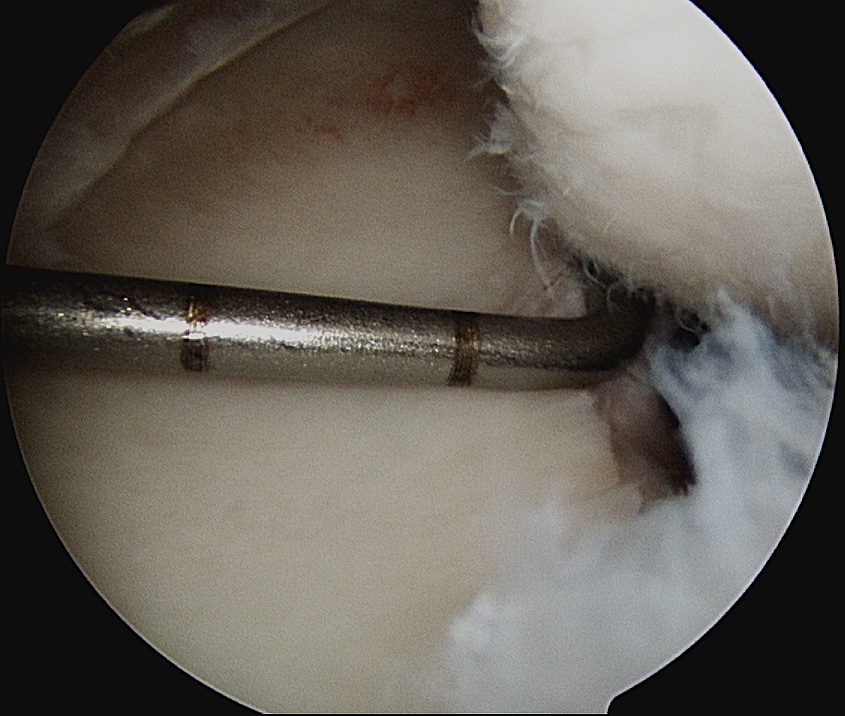
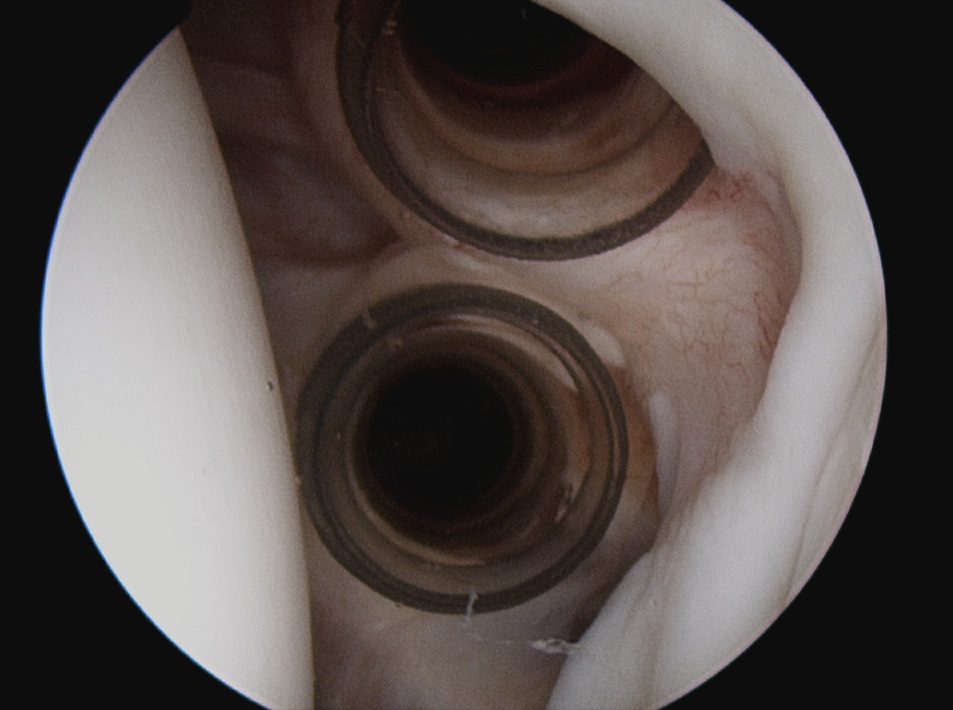
Remaining anchors
- 5 mm apart
- beware lysis and risk of anterior glenoid / postage stamp fracture
- up to glenoid equator
- usually three in total
Additional Issues / Continued Instability
Capsular Shift
- take bite of capsule with suture passer, then labrum
SLAP
- contributes to inferior instability
- requires repair
Rotator Interval
- can tighten with continued instability
- close capsule in this area with suture
- must do with arm at 30o ER
- do away from glenoid on humeral side or will make patient very stiff
- SGHL to MGHL
- must do last
Results
Primary Arthroscopic Stabilisation
Altchek et al Am J Sports Med 2010
- Hospital for Special Surgery New York
- prospective follow up 88 patients 2 years
- 18% recurrent instability episode / 3% revision
- identified patients < 25 / ligamentous laxity / Hill Sachs > 250mm3 high risk
Carreira et al Am J Sports Med 2006
- prospective follow up 87 patients followed for 2 years
- 10% recurrent instability
Arthroscopic v Open Bankart Repair
Bottoni et al Am J Sports Med 2006
- RCT open v arthroscopic, 2 - 3 year follow up
- 2 failures in open group v 1 failure in arthroscopic group
- open took significantly longer and was associated with decreased ER
Revision of Failed Arthroscopic Stabilisation
Cho et al Am J Sports Med 2009
- revision of 26 failed arthroscopic stabilisation with open bankart
- redislocation in 3 shoulders all with engaging Hill Sachs and ligamentous laxity
Francheschi et al Am J Sports Med 2008
- 10 patients with failure of arthroscopic stabilisation
- managed with repeat arthroscopic stabilisation
- 1 recurrence