Mechanism
1. Direct lateral blow to patella
- usually with knee partly flexed and quadriceps relaxed
2. Indirect low energy injury
Epidemiology
2 Groups of Patients
1. Patients with no predisposition to patella instability
- traumatic injury
- contact sports
2. Patients with anatomic predisposition to instability
- atraumatic / minimally traumatic injury
- young / valgus malalignment / ligamentous laxity / malrotation
Associated injuries
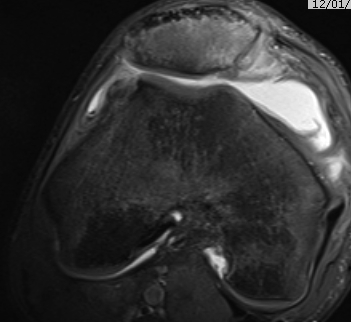
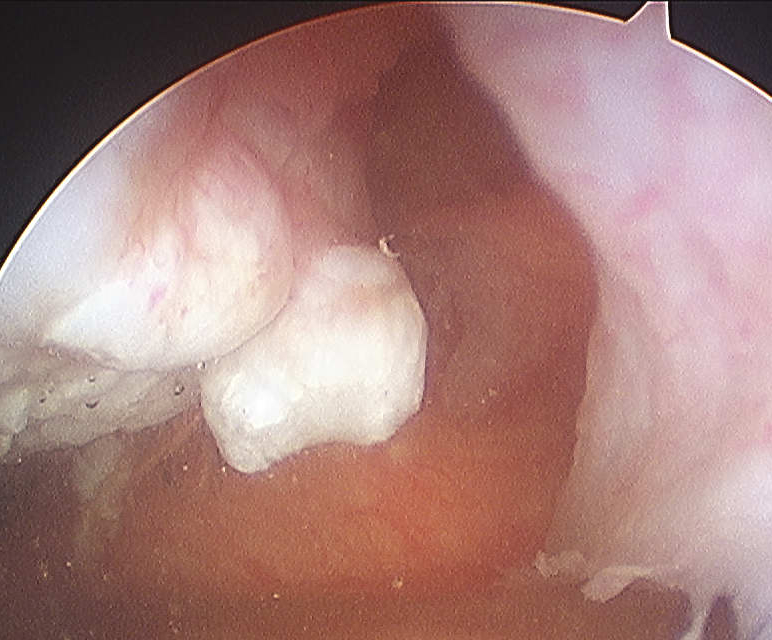
Osteochondral fracture (40-50%)
- LFC or medial facet patella
- patient will have haemarthrosis
- must identify this group, investigate and manage appropriately
Pathology
Medial Patellofemoral Ligament (MPFL)
- from MFC between femoral epicondyle and adductor tubercle
- to superolateral border patella
- deep to retinaculum / superficial to capsule
Usually tears off femur
Acts as a checkrein to lateral patella subluxation
- will usually be torn in all patients with patella dislocation
Recurrence rate
15-20%
- more likely in those predisposed to instability
Reduction technique
Conscious sedation
- knee extended
- medial force on patella
- usually reduces easily
- splint
Examination
Haemarthrosis post reduction
- investigate further
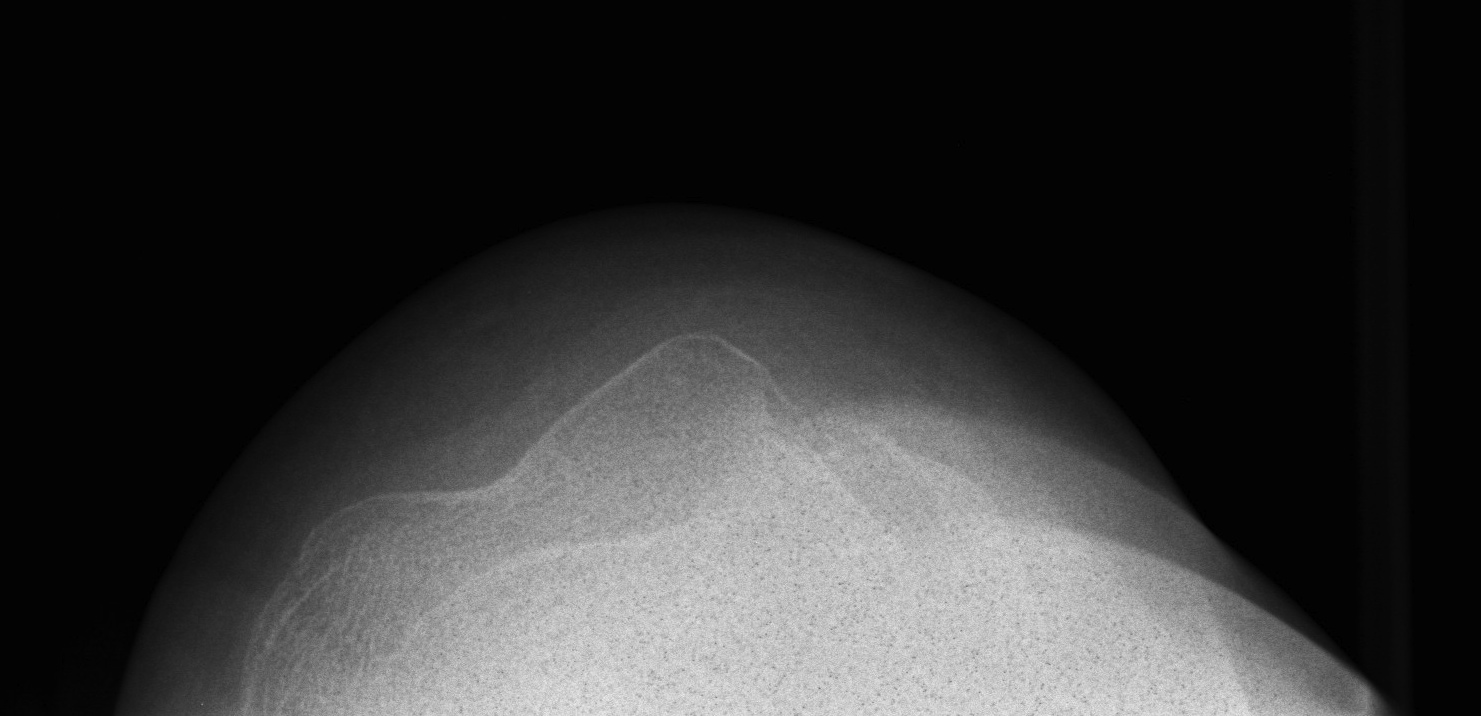
Xray
AP / Lateral / Skyline
- examine carefully for loose body

CT
Shows loose body and origin
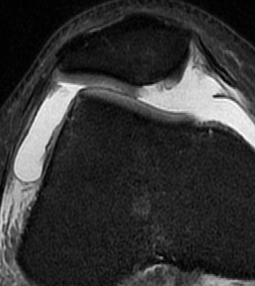
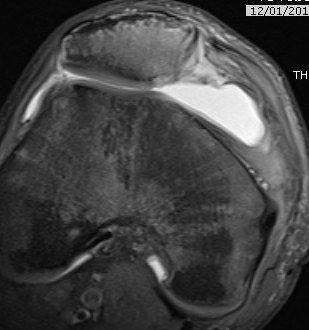
MRI
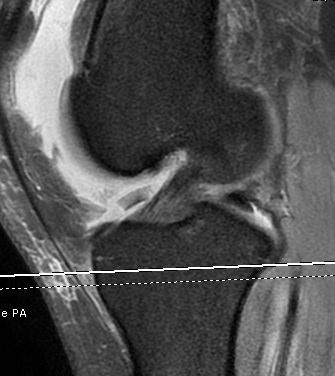
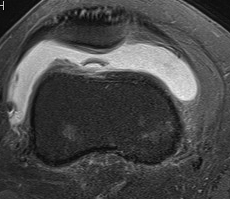
Demonstrates
- MPFL tear
- cartilage damage
- loose body
Management
Non operative
Options
1. First time dislocator with no associated injury
- splint in full extension with lateral patella pad
- reapproximate torn medial structures
- 4 weeks
- then begin VMO exercises +++
2. Recurrent dislocator
- splint only initially for symptom relief
- early ROM and rehabilitation
- no role for long term splintage
Operative
Indications
- loose body
- management of OCD Lesions
- +/- early MPFL repair
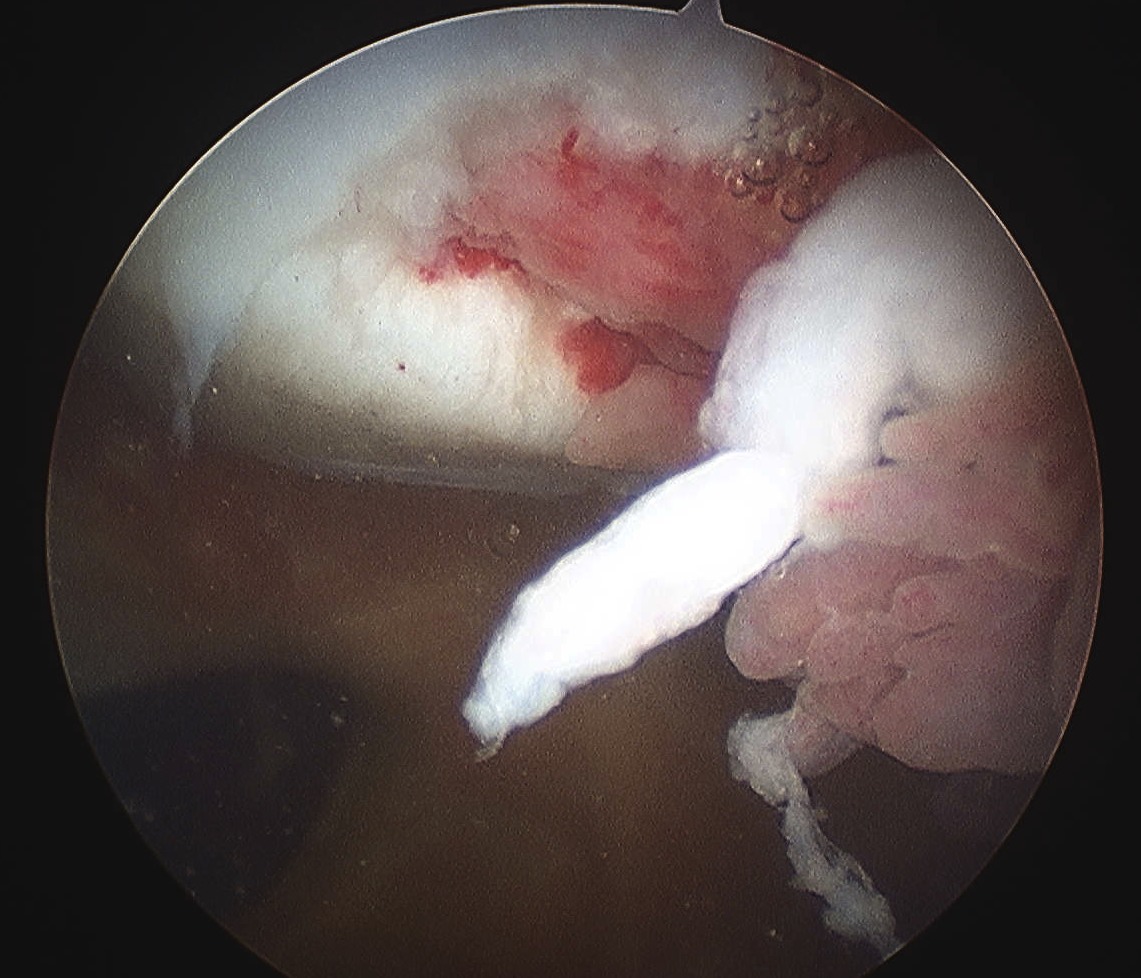
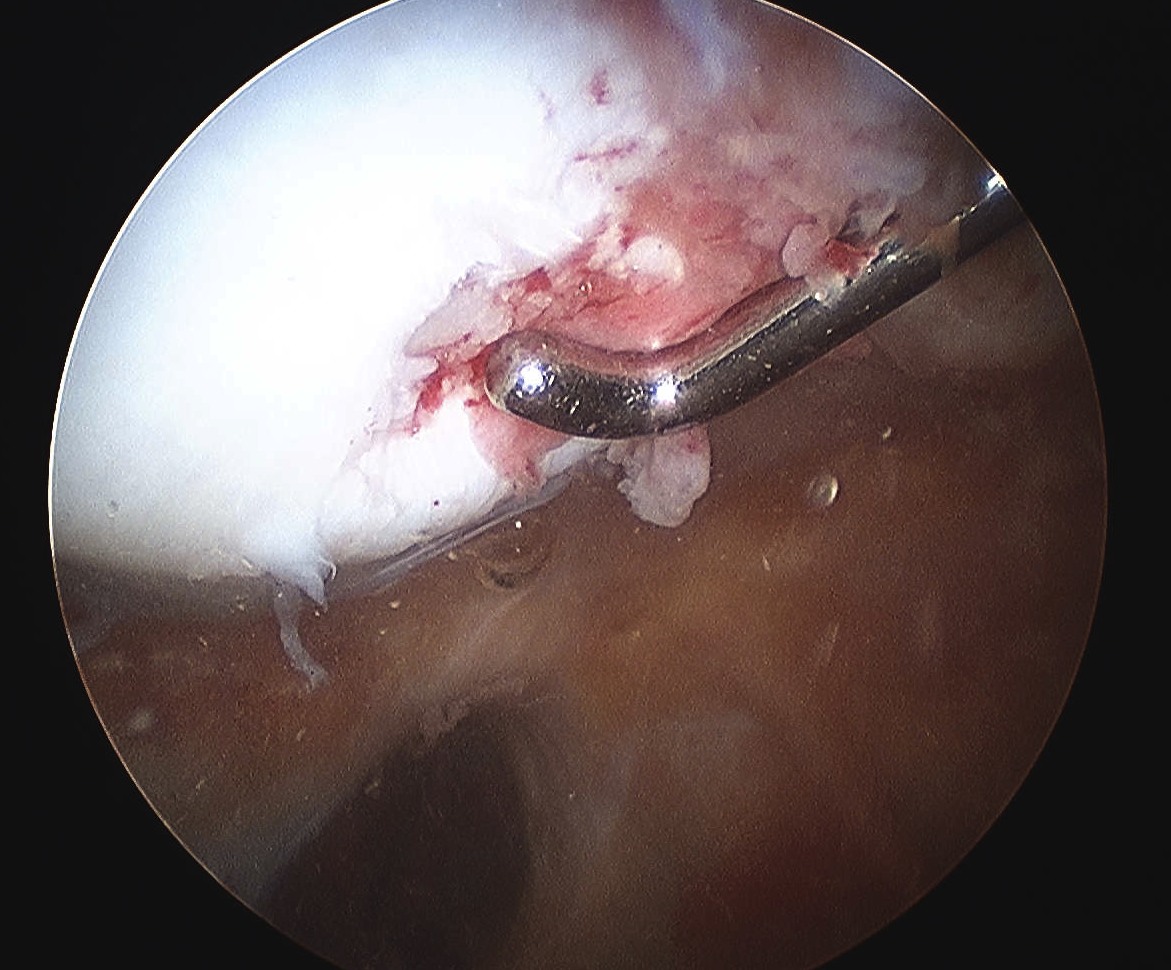
Arthroscopy
Assess Patella and Femoral Lesions
1. Small pieces cartilage
- remove loose bodies
- microfracture if necessary

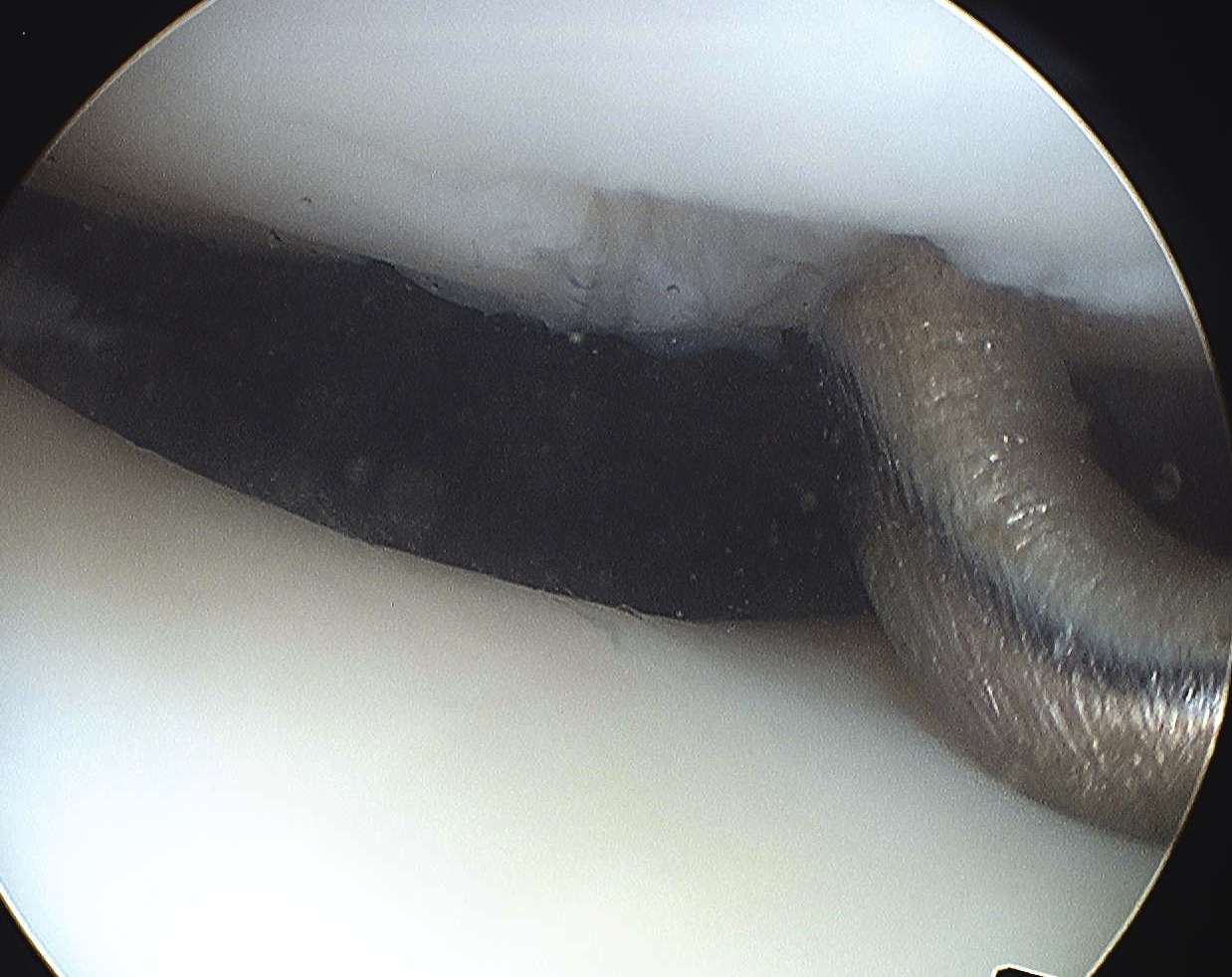
2. Large Osteochondral Fragment
- usually medial patella or lateral femur
- open approach to knee
- reduce and fix with bioabsorbable compression screws / pins
3. Large Chondral piece with minimal or no bone
- can attempt suture fixation
- need to warn of risk of failure and need for reoperation
- careful monitoring
4. Large irreparable chondral lesion
- remove loose body
- microfracture / abrasion initially
- if continue to be asymptomatic, consider alternative procedure
- MACI / mosaicplasty
Early MPFL repair
Issue
- ? would recurrence rates be reduced with early repair / reconstruction MPFL
Results
Palmu et al JBJS Am 2008
- RCT of early operative treatment in adolescents < 16
- very high rates of recurrence in both groups (70%)
- up to 50% of this group had contralateral patella problems
Silanpaa et al Am J Sports Med 2008
- compared operative and non operative treatment
- all operative patients had arthroscopic repair of medial retinaculum
- equal (20%) redislocation in each group
Christiansen et al Arthroscopy 2008
- RCT comparing non operative to open MPFL femoral repair
- redislocation rates the same in each group
Camanho et al Arthroscopy 2009
- RCT of operative v non operative
- excluded patients with flat trochlea / valgus > 15o / patella alta
- in surgical group determined if injury on patella side or femoral side
- 7 from patella repaired arthroscopically
- 10 from femur repaired open with anchors
- 0/17 in surgical group redislocated
- 8/16 in surgical group redislocated
Problem
1. Can repair MPFL but if anatomically predisposed to instability
- will still redislocate and rerupture MPFL
- exclude valgus / alta / flat patella
2. If attempting early repair, need to address specific MPFL pathology
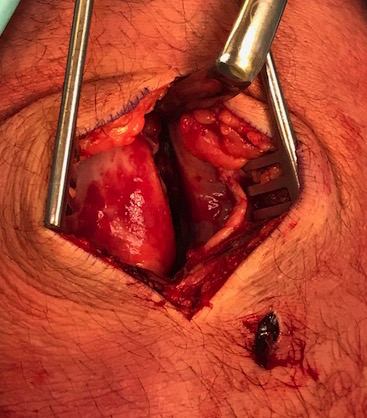
Open Technique
Very important to determine if torn from patella or medial epicondyle
- MRI very useful
1. Medical epicondyle avulsion
- over medial epicondyle
- divide deep fascia
- elevate VMO
- identify MPFL
- repair using bone anchors
2. Patella MPFL avulsion