Definition
Full thickness loss of the articular cartilage lining the patella and the trochlea
Epidemiology
Hart et al Br J Sports Medicine 2017
- systematic review on prevalence of PFJ OA on xray / MRI knees with pain
- 50% incidence of OA affecting the PFJ
Kobayashi et al Osteoarthritis Cartilage
- systematic review of patients with knee pain
- overall prevalence PFJ OA 39%
- PFJ OA females 41%, males 23%
- isolated PFJ OA 8%
Etiology
Obesity
Repetitive deep flexion
Malalignment / patella maltracking / trochlea dysplasia
Lateral patella tightness
Blunt trauma
Symptoms
Anterior knee pain - sitting / rising from chair / stairs
Signs
Tender patella - especially lateral facet
Pain with movement PFJ
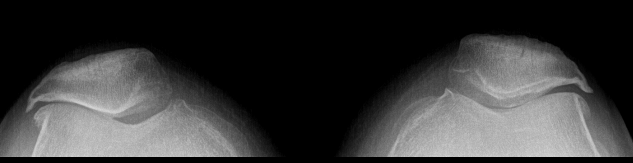
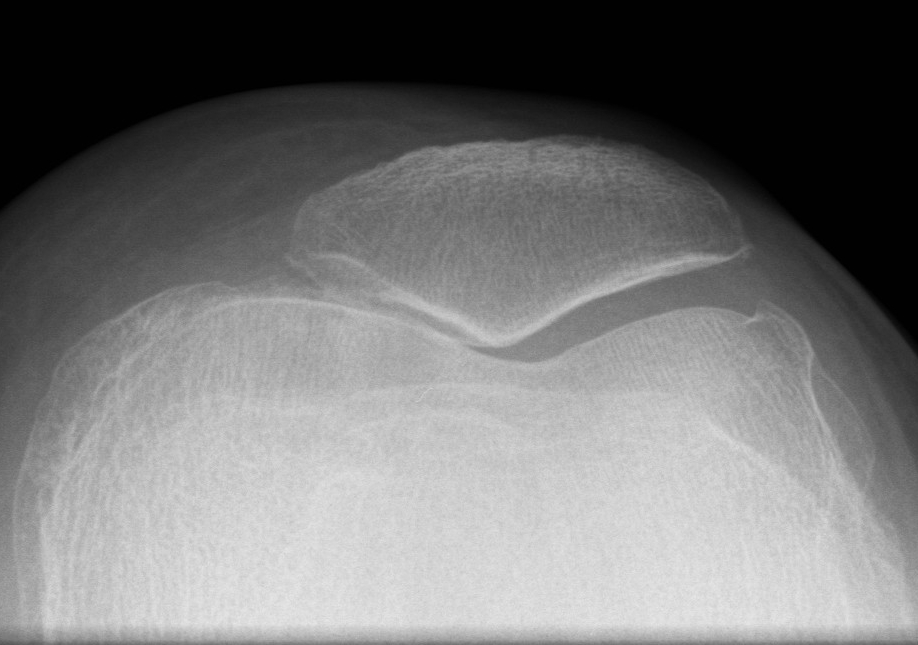
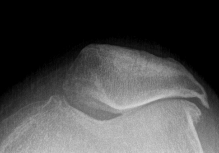
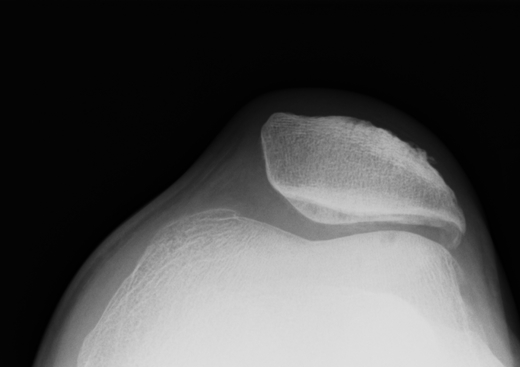
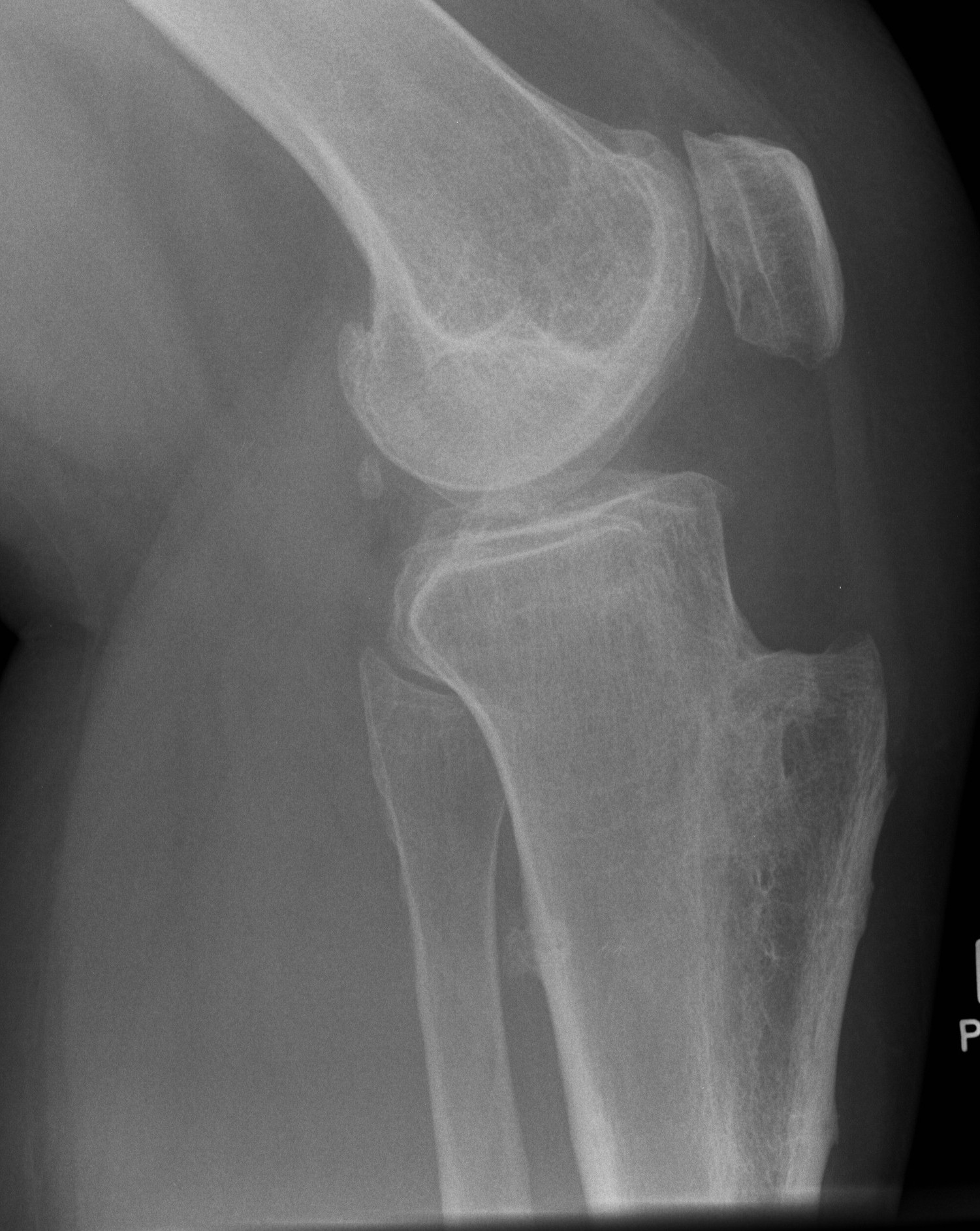
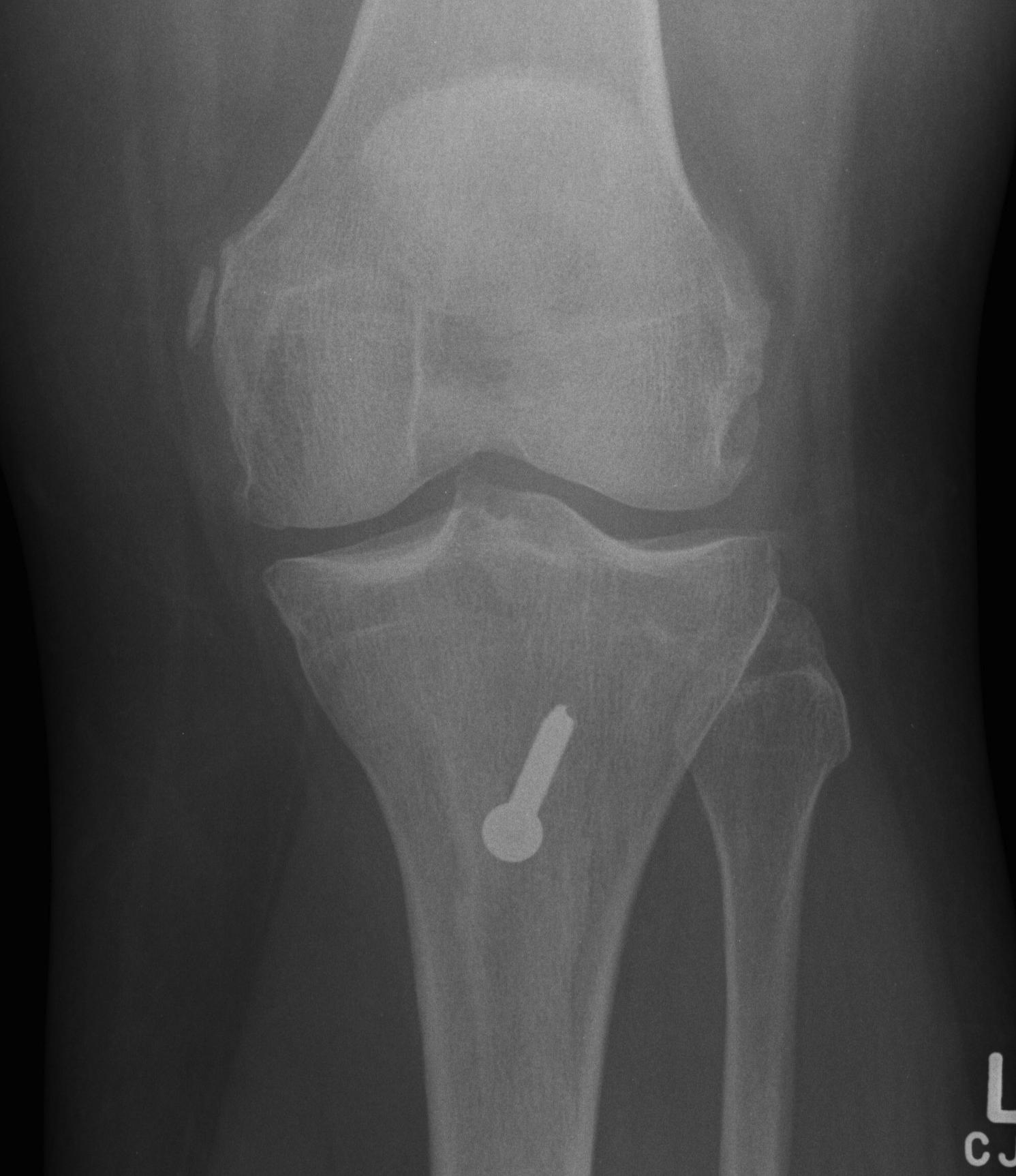
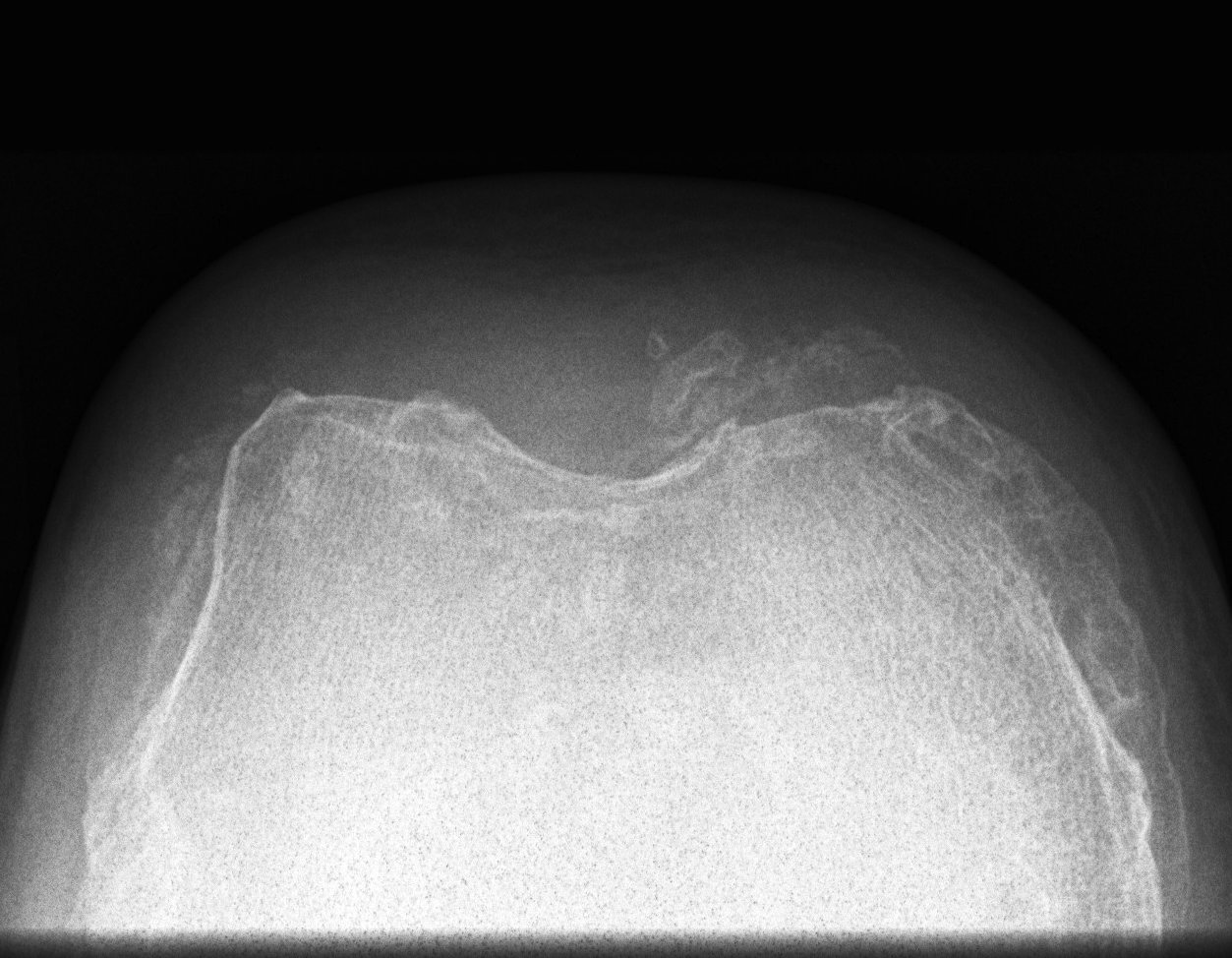
X-ray
Narrowing / osteophytes / sclerosis
Tilt / subluxation

Tilt Subluxation / osteophytes
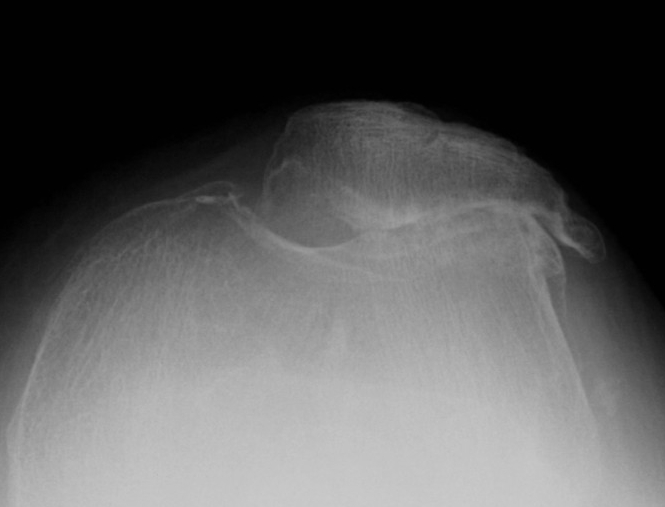
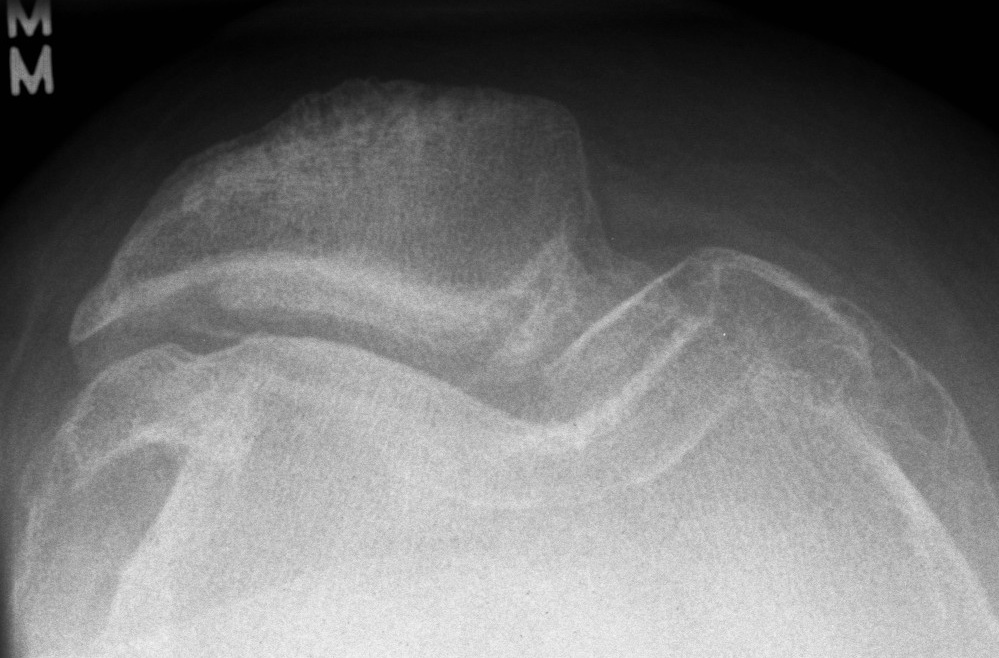
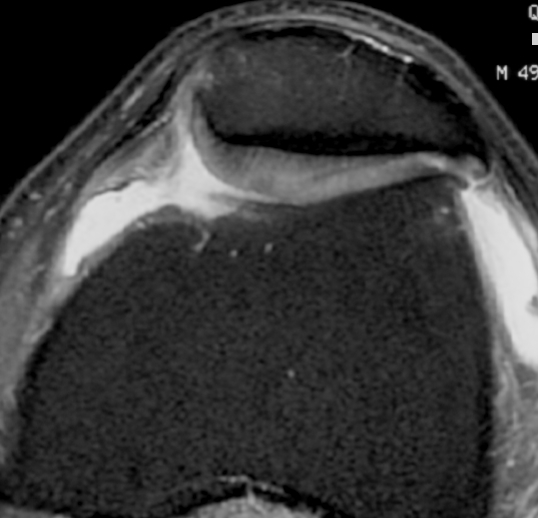
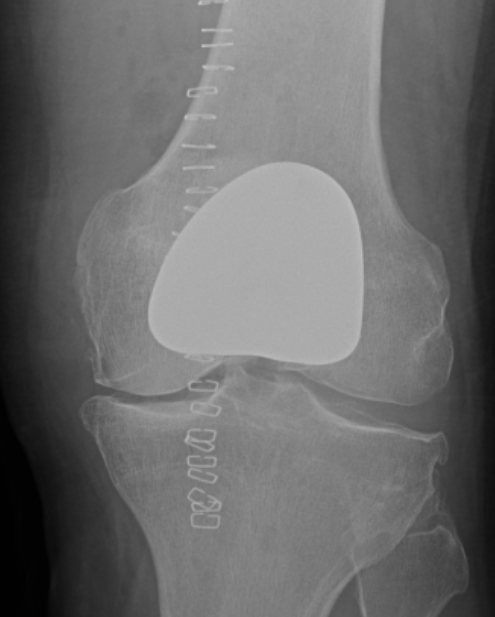
MRI
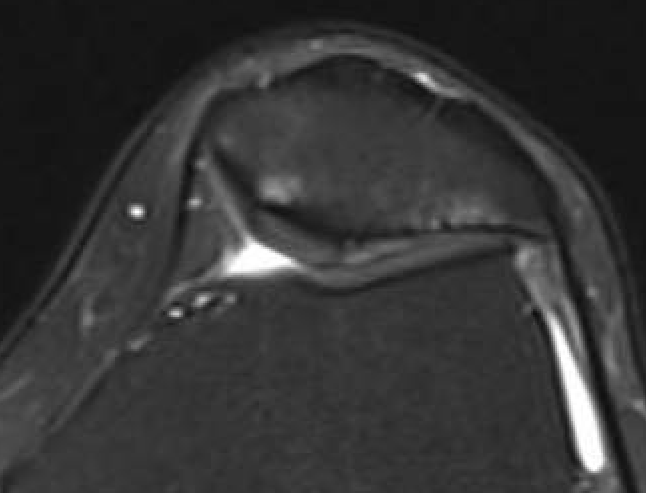
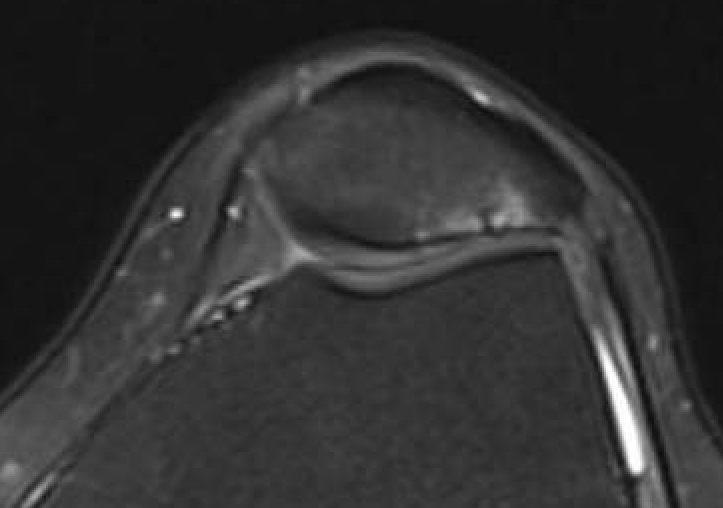
Moderate lateral facet PJF OA with tilt
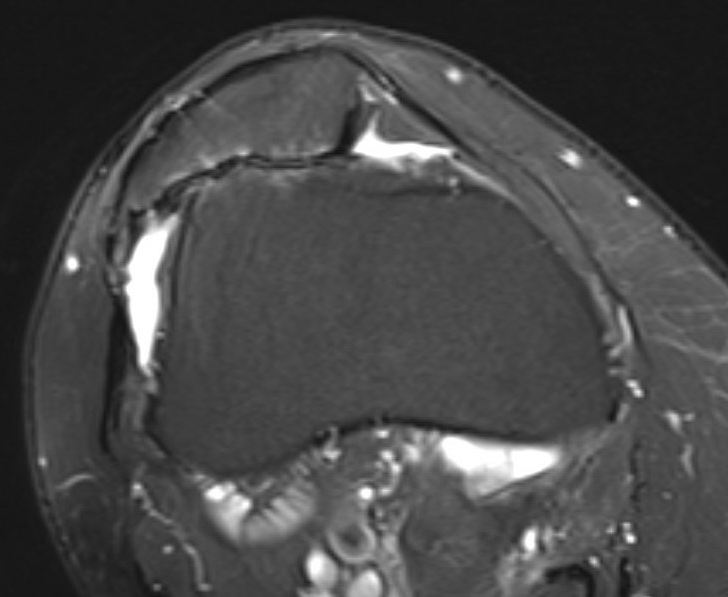
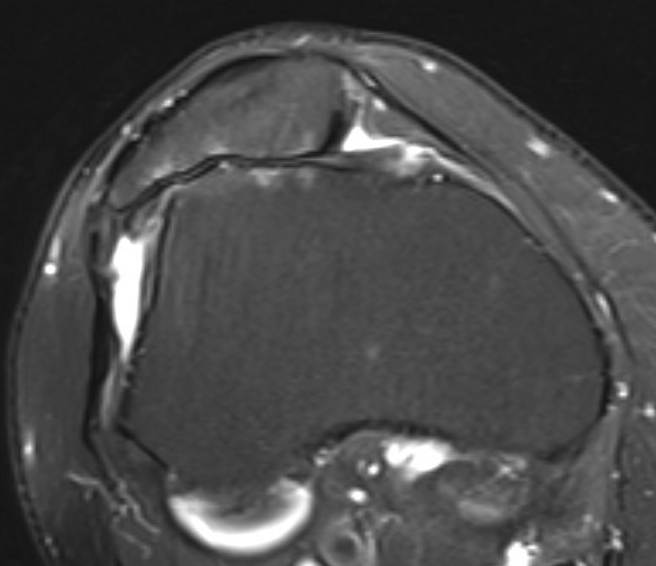
Severe lateral PFJ OA in the setting of maltracking / subluxation / tilt
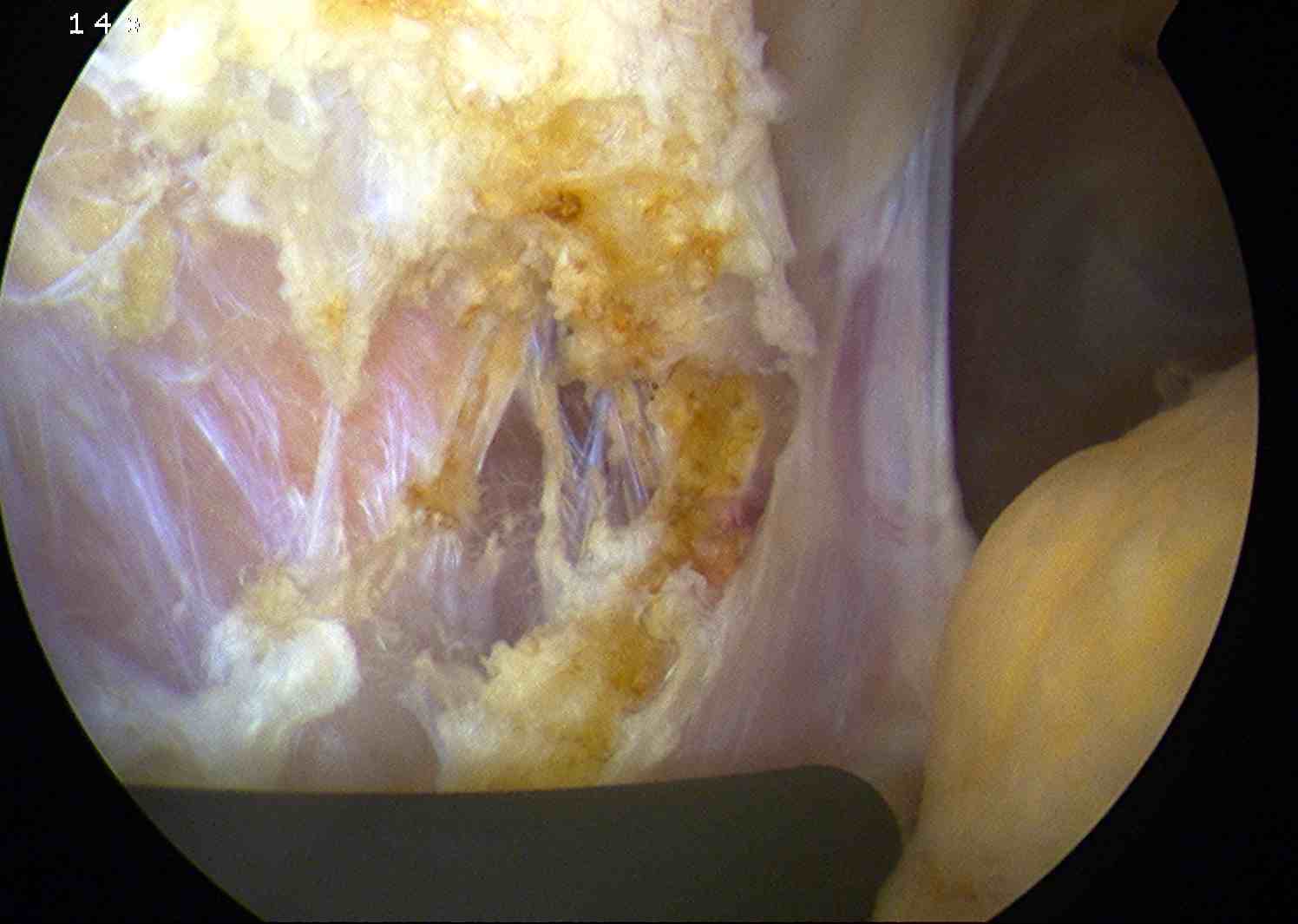
Arthroscopy
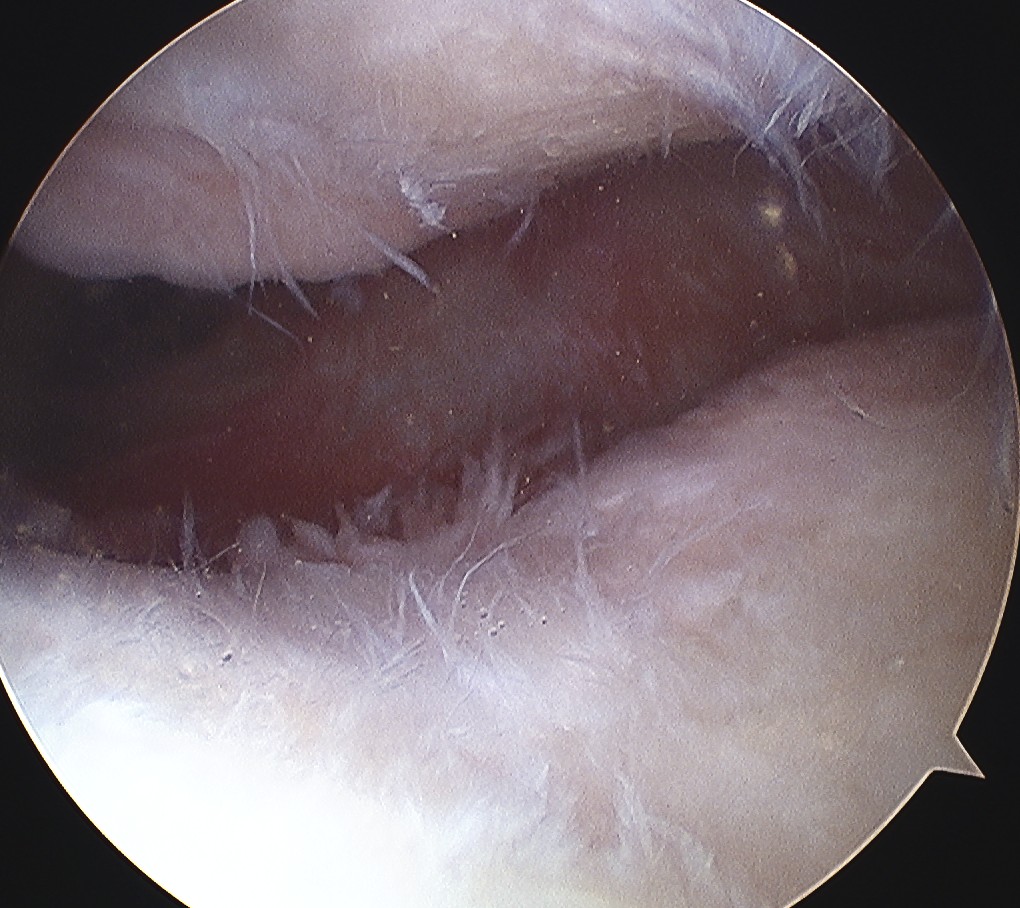
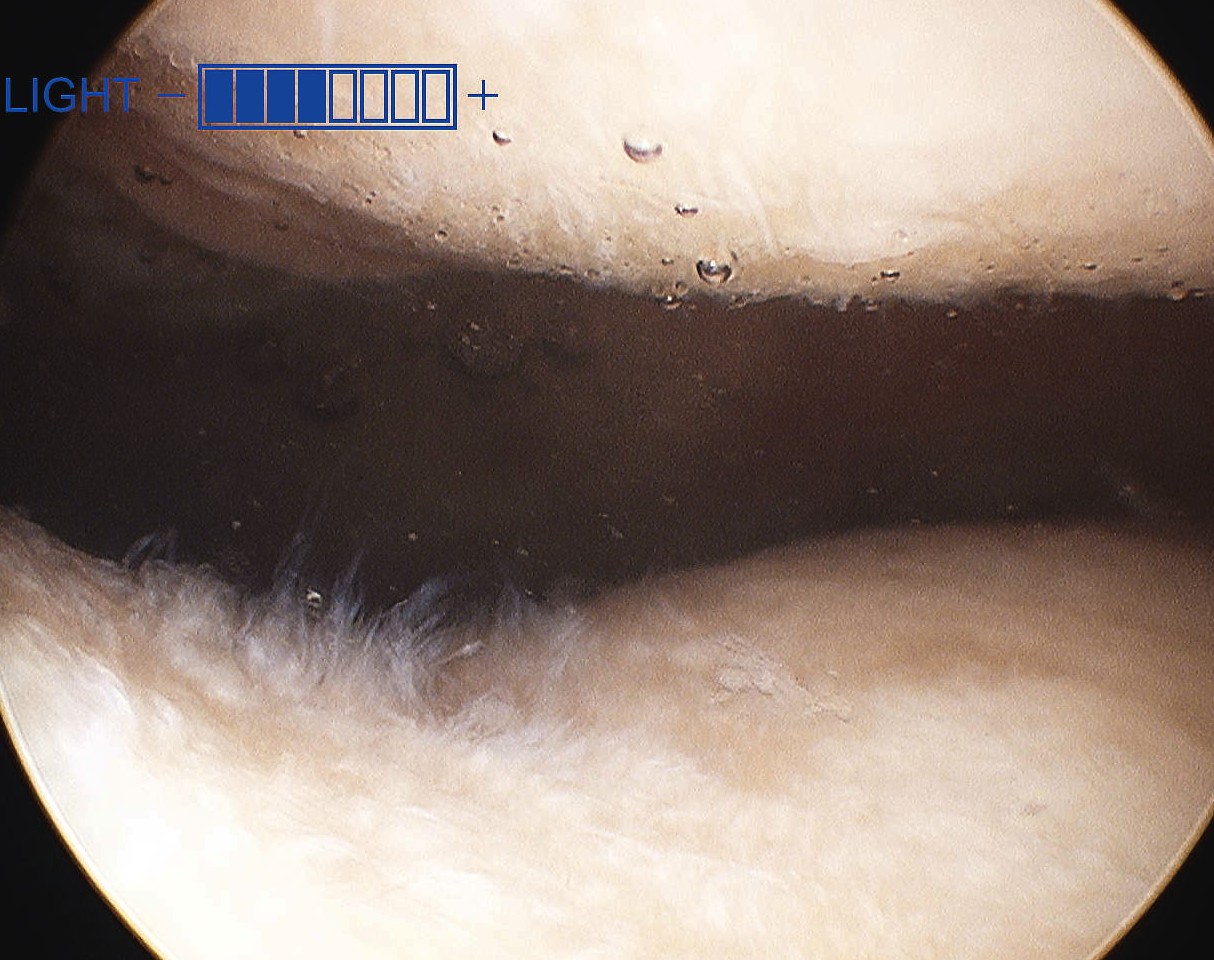
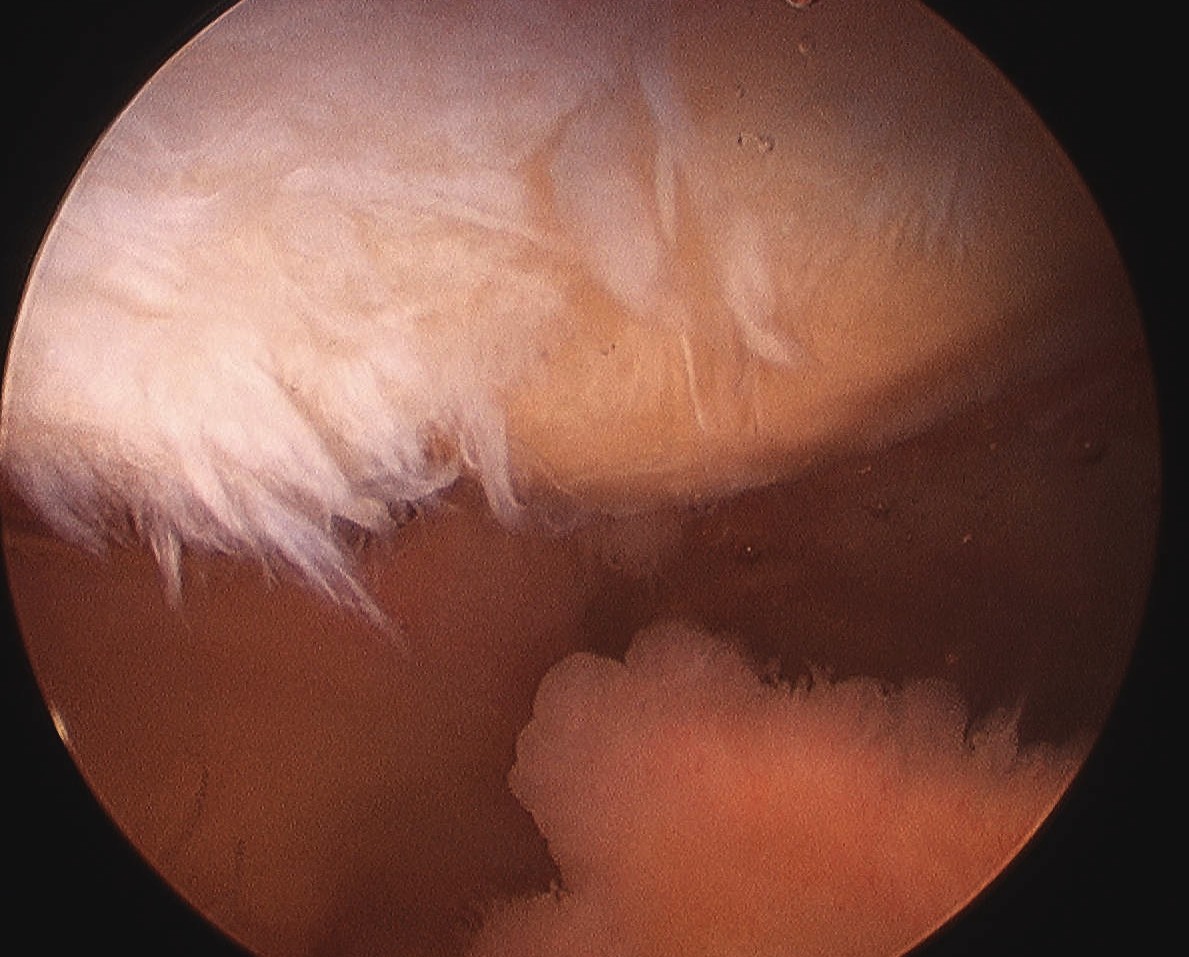
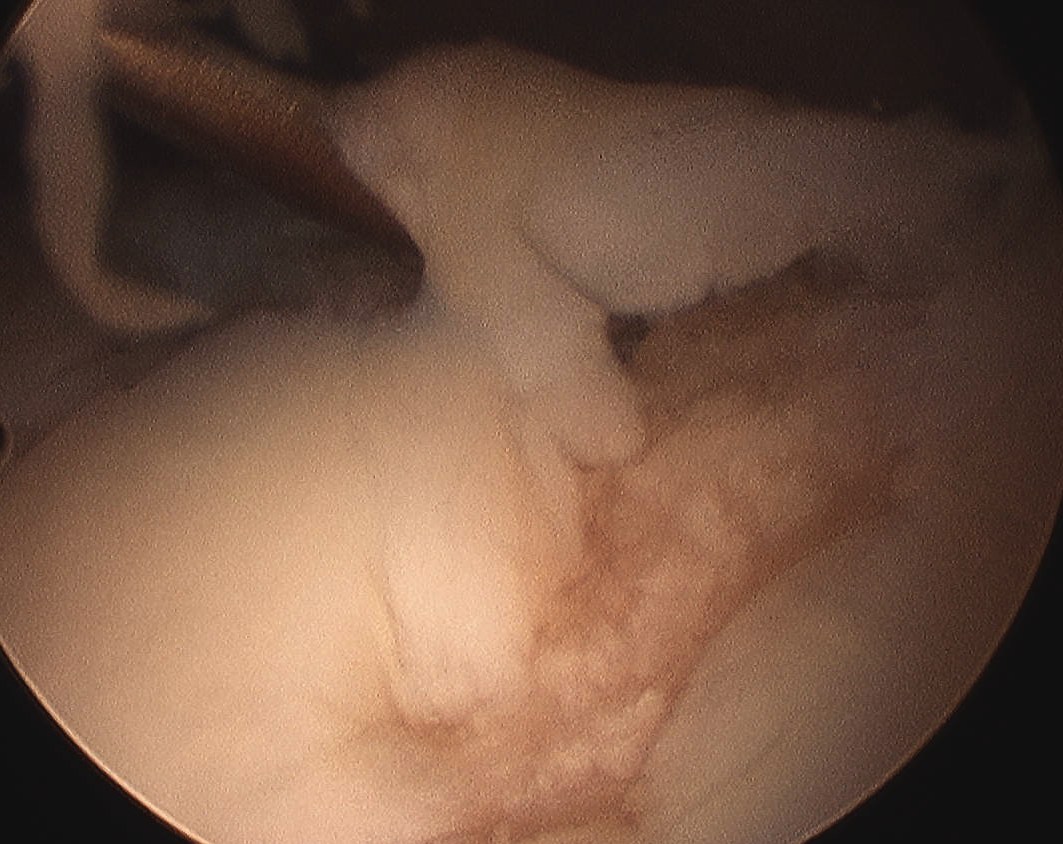
Patterns
Lateral facet - patella maltracking / trochlea dysplasia
Medial facet - patella dislocation and cartilage damage
Global - primary OA, patella fracture, obesity
Central trochlea - repetitive deep flexion
Medial facet OA Lateral facet OA
Management
Non Operative
Quadriceps exercises
van der Heijden et al Cochrane Database 2015
- evidence for exercise therapy in reducing anterior knee pain
Bracing / Taping
- systematic review of bracing and taping for PFJ OA
- good evidence for short term reduction in pain
Injections
Hyaluronic acid
Hart et al Orthop J Sports Med 2019
- RCT of 86 patients with patellofemoral pain syndrome
- no efficacy of HA versus sham injections at 6 months
PRP
- meta-analysis of RCTs of injections for knee OA
- 10 RCTs and 1000 patients
- PRP superior to HA and saline at 12 months
- systematic review of PRP versus HA for knee osteoarthritis
- improved outcomes with PRP versus HA
Operative
Options
Lateral retinacular release
Tibial tuberosity osteotomy
Facetectomy
Patellectomy
Patellofemoral joint replacement
Total knee replacement
Lateral retinacular release
Indications
Lateral facet OA in setting of lateral tilt and tight lateral retinaculum
Lateral patella compression syndrome
Complications
Medial patella instability - don't over release
Hemarthrosis - superior lateral geniculate artery
Technique
Vumedi arthroscopic lateral release technique
Results
Arthroscopic lateral release
Aderinto et al Arthroscopy 2002
- retrospective study of 53 knees
- 80% patients felt some reduction in pain
- 41% unsatisfied
Open versus arthroscopic
Hamawandi et al Arch Orthop Trauma Surg 2022
- RCT of open v arthroscopic release in 80 patients
- better functional outcomes at 2 years with arthroscopic release
- 4 cases medial patellar instability in the open release group
Lateral retinacular lengthening
- RCT of arthroscopic release versus open retinacular lengthening
- 86 patients
- better outcomes with open retinacular lengthening
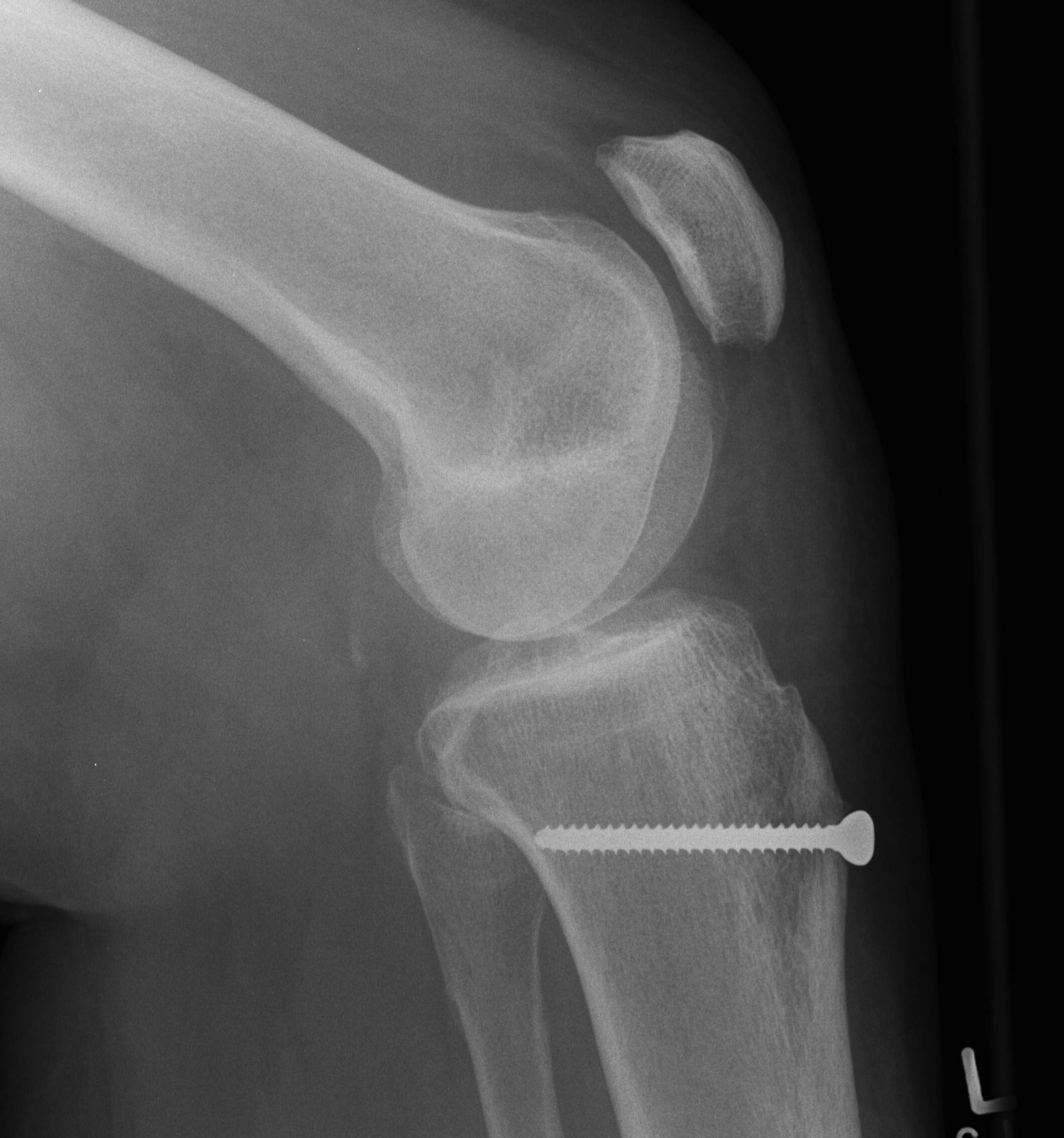
Tibial tuberosity osteotomy
Types
Maquet - elevation
Elmslie-Trillat - medialization
Fulkerson - anteromedialization
Maquet procedure

Technique
Perform TTO then elevate with insertion bone graft
- originally described elevating by 2.5 cm
- problems with skin necrosis / prominence
- reduced to only 1 cm and recommended via an anterolateral incision
Results
- 100 knees treated with Maquet for grade IV OA
- 62% success rate
Atkinson et al Arch Orthop Trauma Surg 2012
- 50 knees with PFJ OA treated with 10 - 15 mm elevation using femoral head allograft
- 77% good or excellent results
- 3 tibial tuberosity fractures
- 8% superficial wound infections
Fulkerson
Technique
Vumedi surgical technique video
Oblique osteotomy 45˚
- enables antero-medial transfer of tibial tuberosity
- unloads the lateral facet simultaneously


Results
Fulkerson et al Am J Sports Med 2019
- anteromedialization osteotomy in 17 knees with distal or lateral OA
- 15 year follow up
- 94% would repeat the procedure
- Fulkerson osteotomy in 40 patients mean age 50
- 20% went on to have TKA
Berk et al Orthop J Sports Med 2023
- review of 344 TTO
- stiffness 16%
- superficial infection 8%
- hemarthrosis 6%
Facetectomy
Indication
Isolated OA of one facet
Techniques
Open procedure
Arthroscopic lateral facetectomy
Youtube surgical technique video
Results
- lateral facectomy in 168 knees with average 11 year follow up
- 37% failure
- arthroscopic lateral facetectomy and release in 56 knees
- 86% survival at 7 years
- arthroscopic lateral release and partial lateral facetectomy in 66 knees
- 88% very satisfied or satisfied
Patellectomy

Technique
Concept
Excise patella in full close retinaculum tightly with VMO advancement
Concerns
- extensor lag and weakness
- continued pain if trochlea lesions
- issues with later TKA
AO Surgery Reference Technique
Results
Outcomes
- patellectomy for OA in 20 knees
- 19/20 satisfied
- systematic review of 31 articles and 1400 patellectomies
- 85% good or excellent if extensor mechanism reinforcement is performed
Complications
- 12 patellectomies
- good function, but extensor weakness and ROM differences
Asopa et al J Orthop Surg Res 2015
- better results with disease confined to the patella
TKA and patellectomy
- systematic review of TKA after previous patellectomy
- reduced flexion and increased risk complications in patients with patellectomy
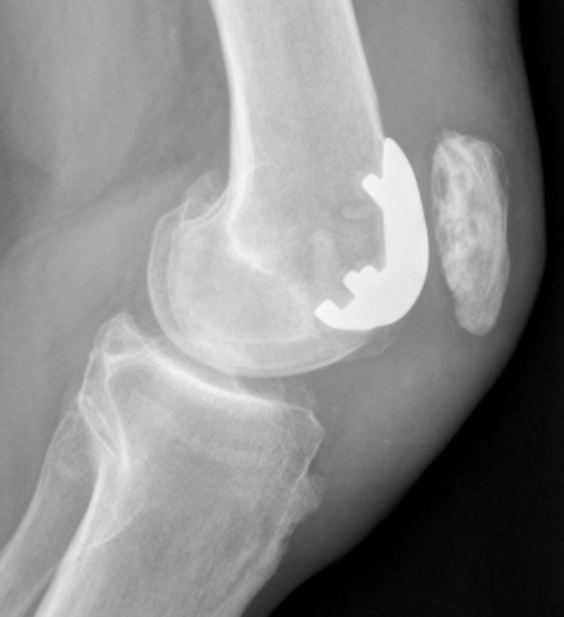
Patellofemoral joint replacement


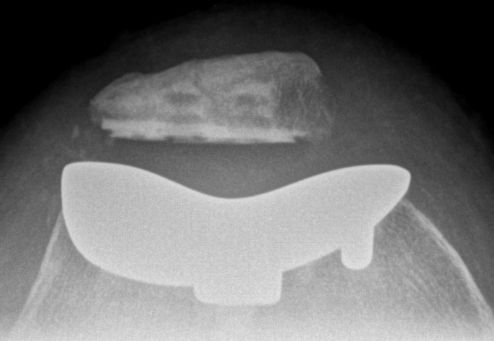
Technique
Vumedi surgical technique video
JBJS Essential Surgical technique PDF
Contra-indications
Inflammatory conditions
Patella maltracking / malalignment
Tibiofemoral arthritis / medial or lateral joint pain / instability
Results
Outcomes
- systematic review of inlay versus only PFJR
- no difference in functional outcome
- higher progression of OA with only trochlea implants
Australian Joint Registry 2023
- 15 year revision rate of 3326 PJF arthroplasty: 35.6
- increased risk with males and < 65
| PFJ Arthroplasty | TKA | |
|---|---|---|
| 1 year | 1.4 | 1.0 |
| 3 year | 6.5 | 2.4 |
| 5 year | 10.6 | 3.1 |
| 7 year | 15.3 | 4.6 |
| 10 year | 22.4 | 6.2 |
| 15 year | 35.6 | 7.7 |
Complications