Graft selection
A. Synthetic Grafts
Good initial results but unacceptably high failure rate with longer follow-up
Problems
1. Too stiff (low ultimate strain)
- poor resistance to abrasion
- ligament failure by attrition most common
2. Recurrent synovitis, infection, loosening and osteolysis
B. Autograft
1. Contralateral BPTB / hamstring
2. Reharvested central BPTB
C. Allograft
- many advantages (shorter surgery, decreased morbidity, larger bone blocks)
- disadvantages (disease risk, slower incorporation, higher cost)
- irradiation has dose dependent effect on mechanical properties with significant effect at 3 Mrads
- higher failure rates
- over 1700 revision ACL from ACL registry
- repeat revision 14% allograft
- repeat revision 6% autograft
- 70% lower risk of repeat revision with autograft compared to allograft
Pre-operative Assessment
Crucial to good outcome
Patient expectations
- results not as good as primary
- aim for ADL's, sports may not be possible
History
- history infection
- history arthrofibrosis
- has knee ever been good or always unstable
- was it good then traumatic injury
Examination
Alignment
ROM
- patient hyperextension linked to poor outcomes
Confirm ACL deficient
- Lachman's / Anterior drawer / Pivot Shift
Check Secondary restraints
- assess PCL / PLC
- dial test important
- may need posterior and varus stress xrays
Old OT notes
Technique / graft
Fixation techniques
Tunnel sizes
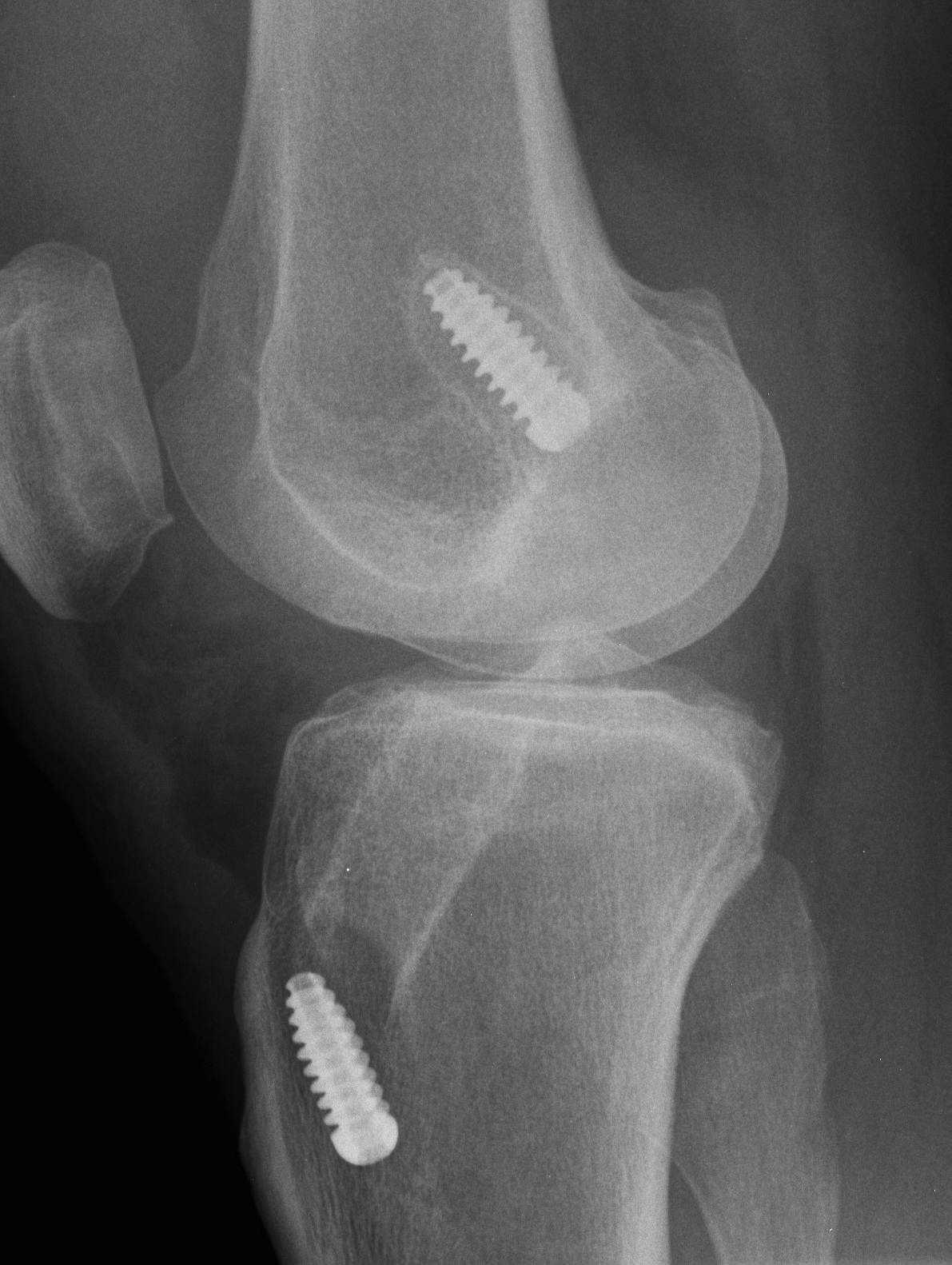
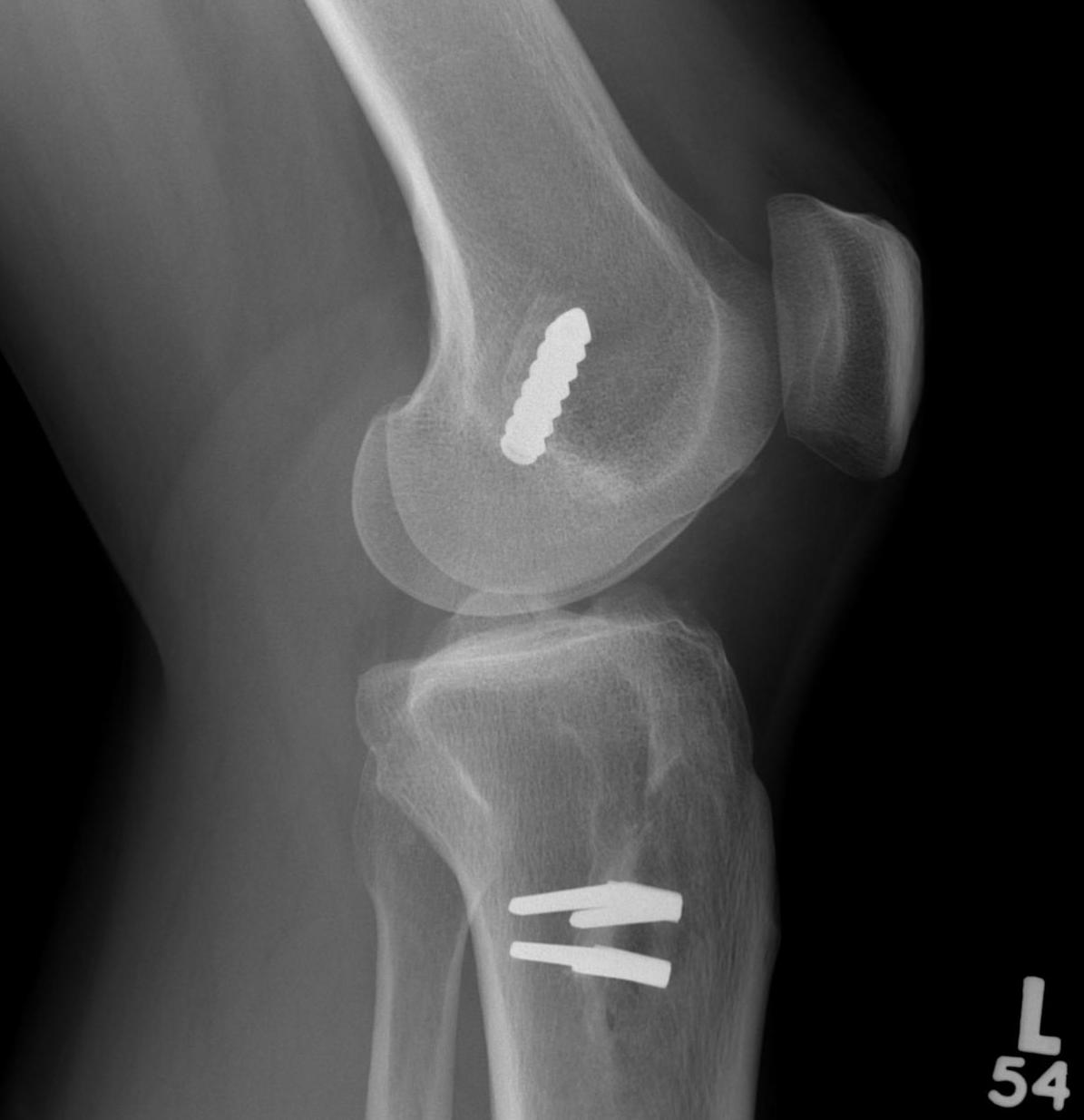
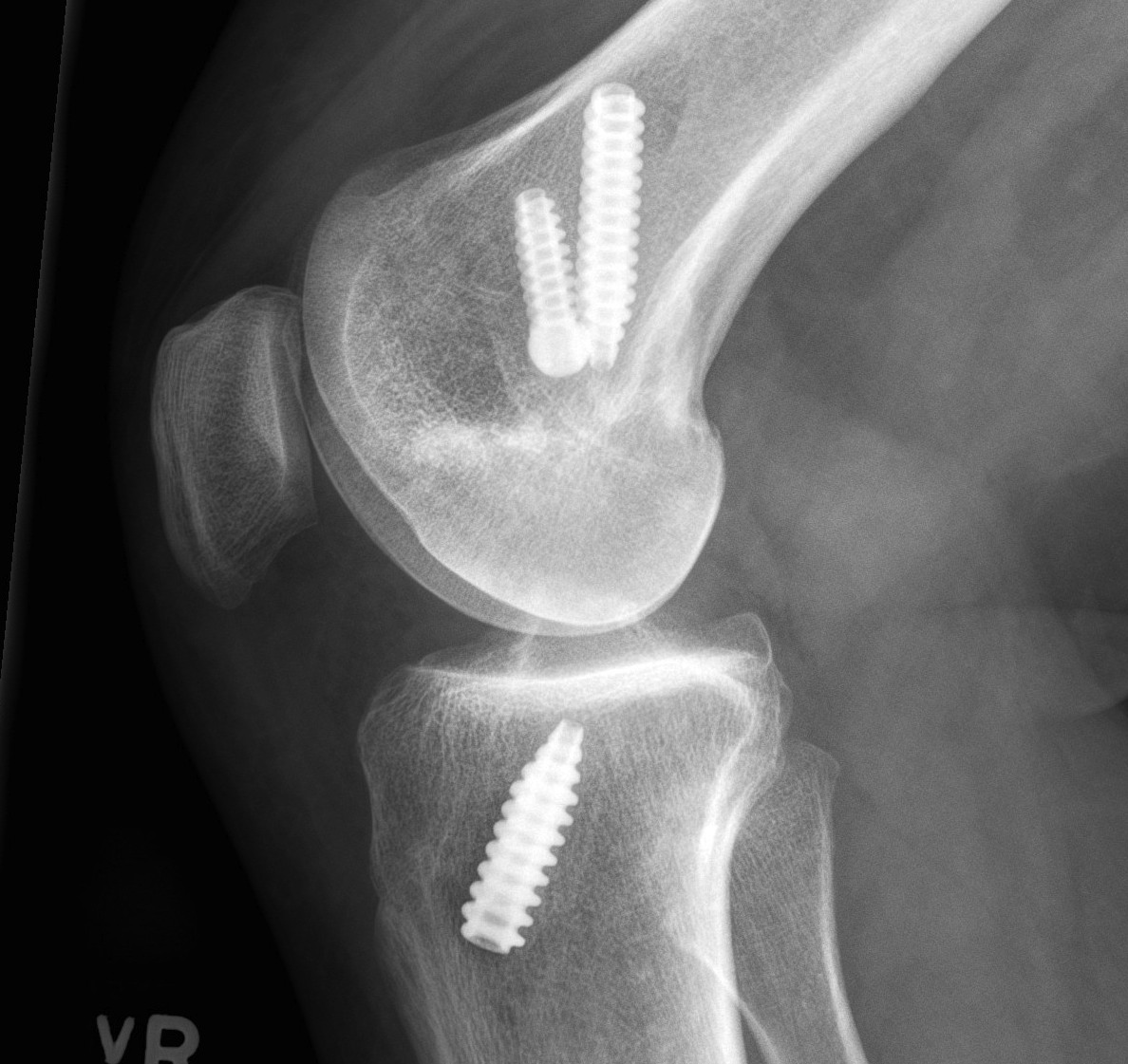
Xray
AP and Lateral
- assess tunnel placement
- Assess metal work
- types of fixation
- metal v plastic
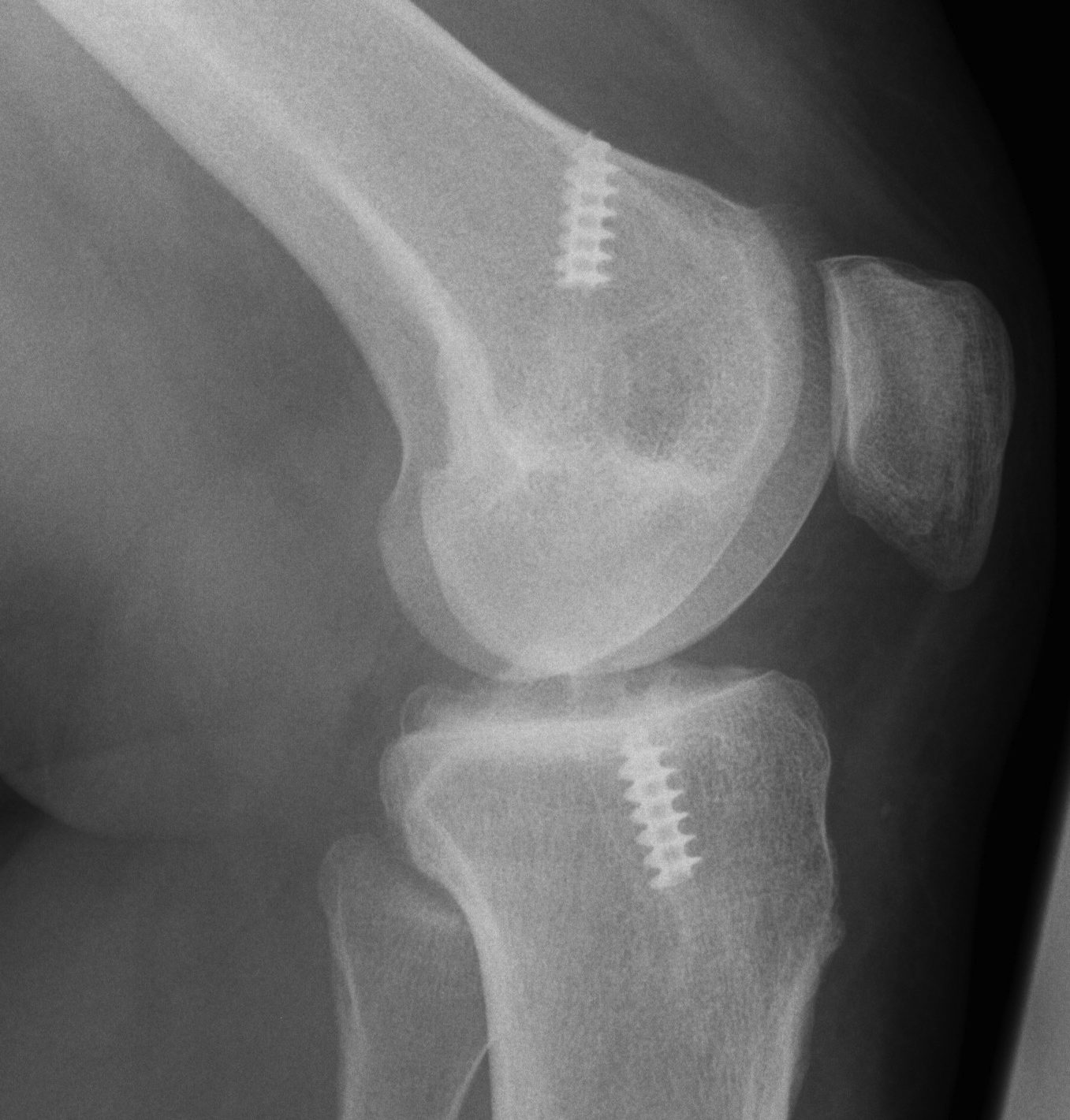
Stress xrays
- check PCL / PCL
MRI
1. Is graft intact / non functional or ruptured
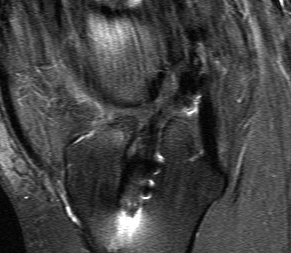
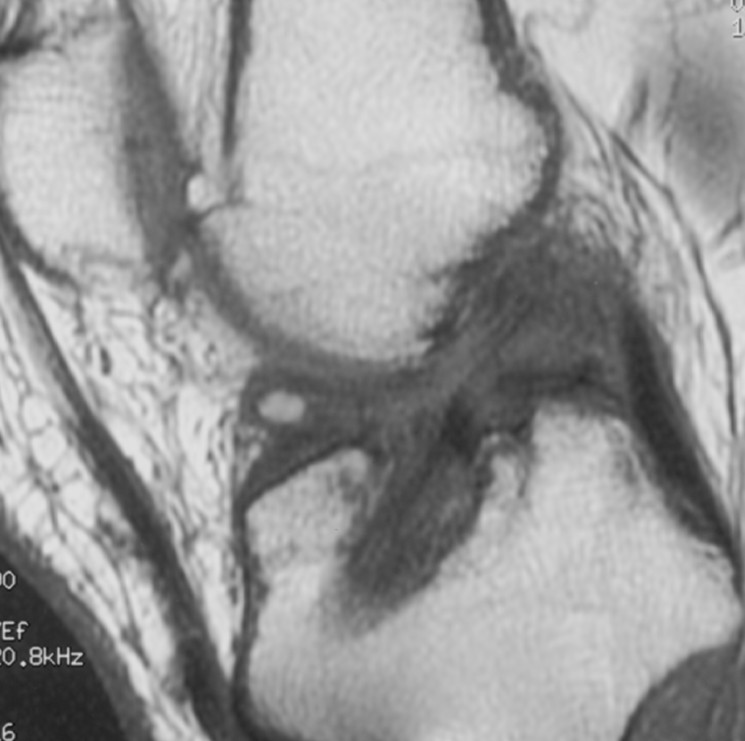
2. Assess meniscus / chondral surfaces
3. Evidence of other ligament injury (difficult)
CT
Assess for tunnel lysis
Arthroscopy / EUA
Confirm graft lax or torn / + Pivot Shift

4 Tunnel Situations in Revision Surgery
1. Correct tunnel position, normal size
Reuse same tunnels
- remove hardware
- may require larger screws if some lysis
2. Correct tunnel position, increased size secondary to lysis
Staged bone grafting of tunnels
- use bone cores from iliac crest
- premade synthetic bone graft plugs
- wait for union / 3 - 6 months
- ACL revision
BTPB / Achilles allograft with larger bone block
3. Slightly incorrect tunnel position
Staged bone grafting of tunnels
4. Very incorrect tunnels
New tunnels anterior or posterior
- can leave old metalwork intact
Surgery
Issues
1. Skin incisions
2. Hardware removal
- screwdrivers for metal RCI screws
- drill through bioabsorbable screws
- ignore endobutton
- careful removal of all material in tunnels
3. Revision Notchplasty
- roof and lateral wall
- often osteophytes in this area
- must leave sufficient bone stock
4. Bony tunnels
Find femoral tunnel
- pass beath pin
- decide if tunnel reusable
- will usually be larger
- can use screw if posterior wall remains
Usually do tibial tunnel last
- will lose vision as water escapes
- can be difficult to find tunnel
- use needle to find tunnel
5. Graft
BPTB good option
- larger bone blocks useful in enlarged tunnel
Contralateral hamstring
- involve normal knee
- fixation difficult
6. Fixation
Femoral
- screw if posterior wall remains
- otherwise endobutton
- can tie over screw on femur if need to
Tibia
- usually scew +/- post
6. Secondary restraints
A. Posteromedial instability
- reconstruction / advancement
B. Posterolateral
- valgising HTO
- reconstruction
