

Anatomy
1. Seebacher's 3 layers of the medial knee
| Layer 1 | Layer 2 | Layer 3 |
|---|---|---|
|
Sartorius Sartorius fascia |
Superficial MCL Posterior oblique ligament Semimembranosus |
Deep MCL (meniscofemoral and meniscotibial ligament) Posteromedial capsule |
2. MCL
| Superficial MCL | Deep MCL |
|---|---|
|
Triangular in shape Origin: 3 mm proximal and 5 mm posterior to the epicondyle Insertion: 6 cm distal to the joint line onto posteromedial tibia, deep to pes anserinus Anterior margin free |
Deep to MCL Origin: inferior to medial epicondyle Insertion: 1 cm below joint line Meniscofemoral and meniscotibial ligaments - capsular thickening |
3. Posteromedial corner (5 components)
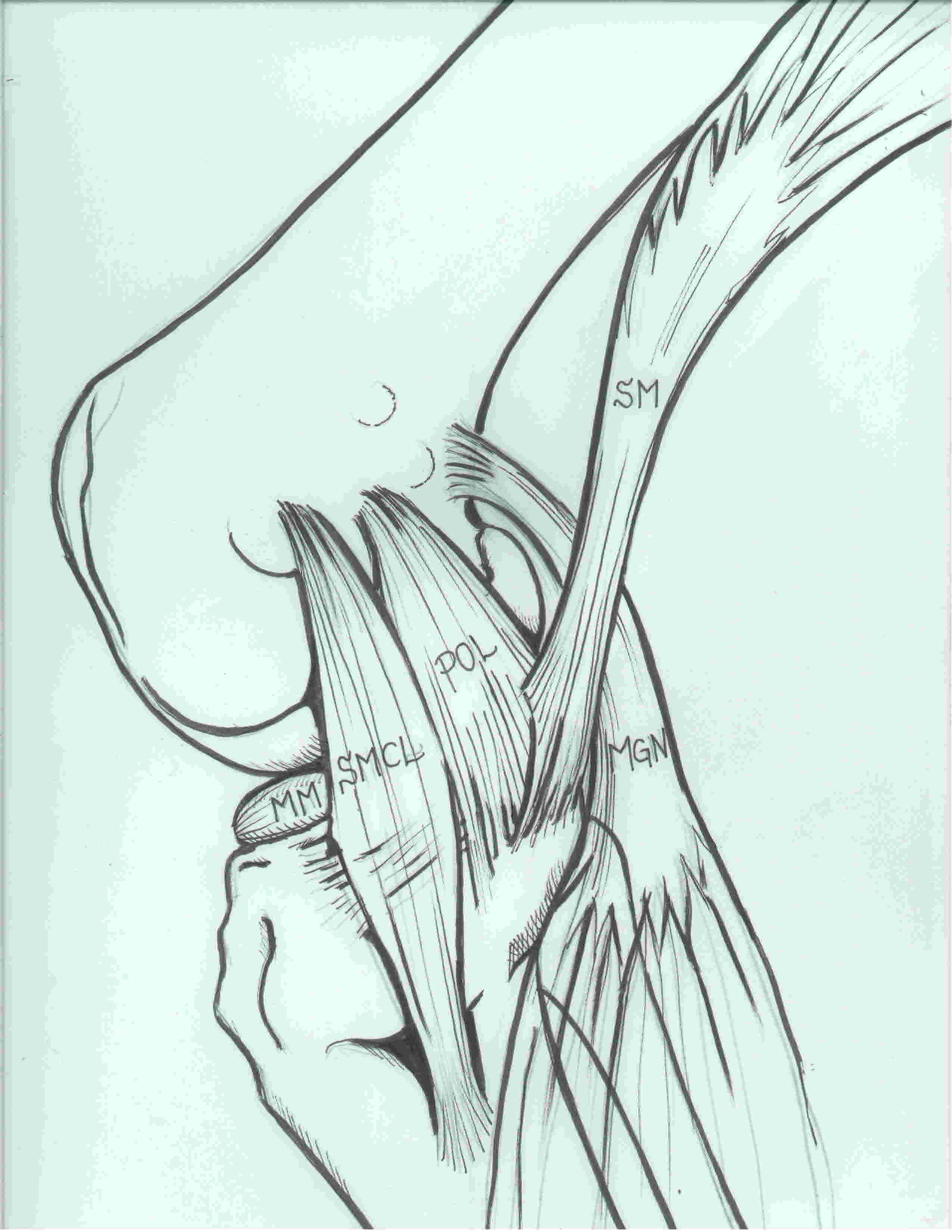
i) Posterior oblique ligament (POL)
- behind / posterior the superficial MCL
- origin: femur posterior and distal to adductor tubercle
- insertion: central arm onto posterior tibia below articular surface and the posteromedial capsule
ii) Semimembranosus
- attaches to the posteromedial corner of the tibia just below the joint line
- also has extensions blending with POL and OPL
- important dynamic stabiliser
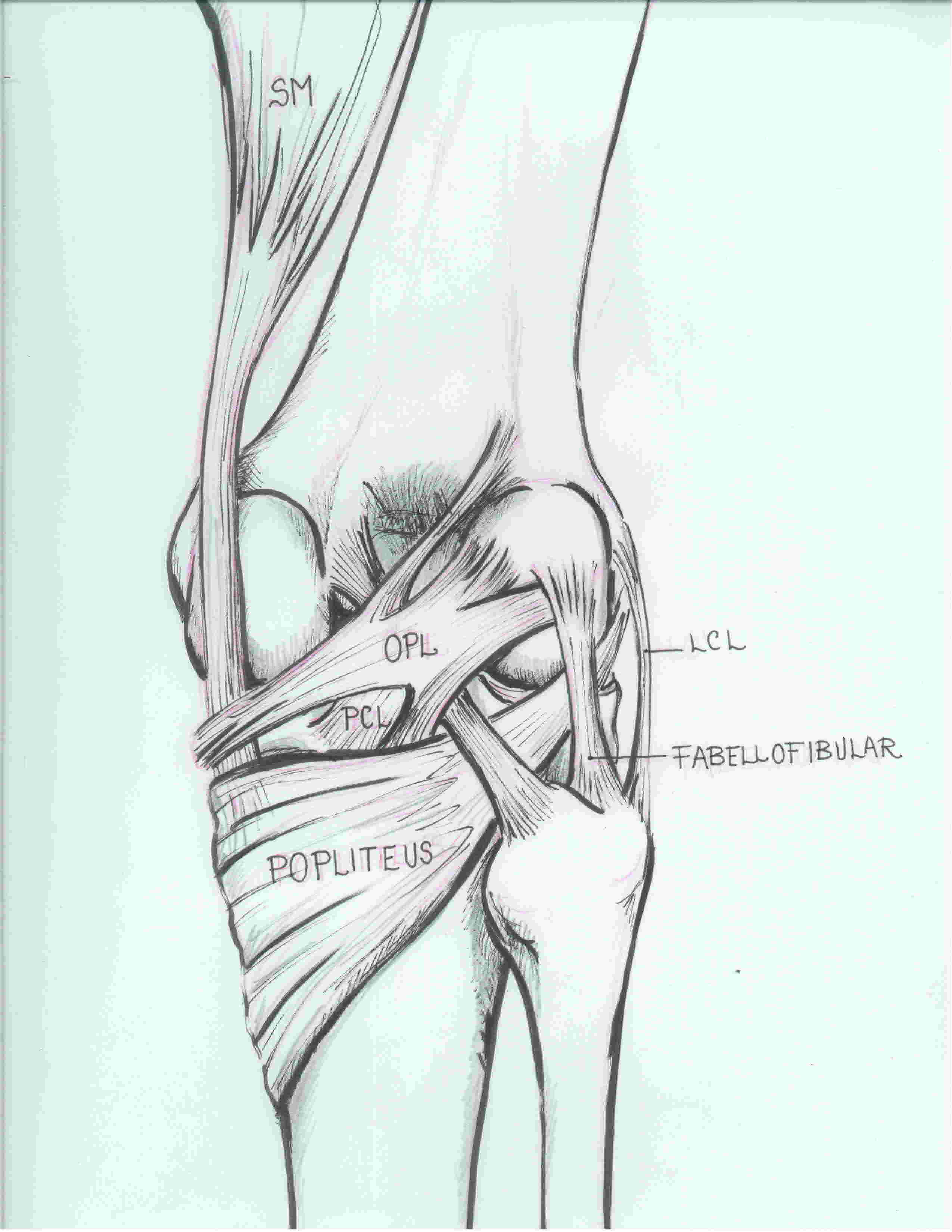
iii) Oblique Popliteal Ligament (OPL)
- extension of semimembranosus
- extents laterally towards lateral femoral condyle
- thickens posteromedial capsule
iv) posteromedial joint capsule
v) Posterior horn of medial meniscus
4. Pes anserinus
Runs superficial to MCL
- 3 components: sartorius, gracilis, semitendinosus
- "Say Grace before Tea"
- the saphenous nerve and small saphenous vein emerge between sartorius and gracilis
Function of MCL and Posteromedial corner
MCL primary valgus stability at 30o flexion
Secondary restraint to
- anterior translation
- external rotation
Secondary static medial stabilisers
- contribute to medial stability in full extension
- ACL
- posteromedial corner
- PCL
Secondary dynamic medial stabilisers
- pes anserinus
- semimembranosus
History
Valgus force +/- external rotation
May hear a pop
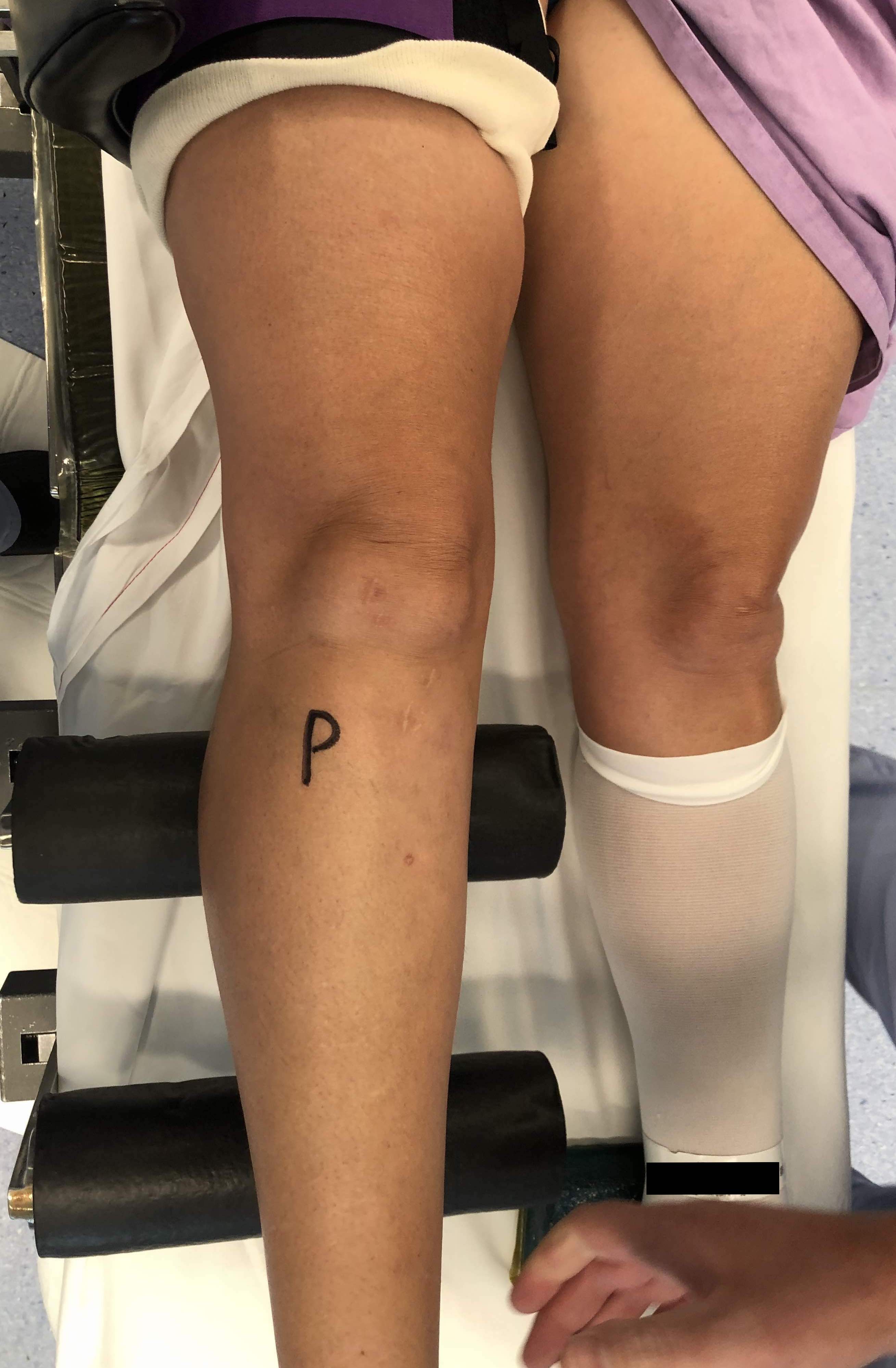
Examination
Discreet tenderness at femoral or tibial insertion of MCL
1. Valgus stress test at 30° flexion and full extension
Remember to test both sides, and compare to contralateral side
Gapping at 30° flexion
- isolated injury to MCL

Gapping in full extenstion
- injury to a secondary stabilizer
- ACL / PCL / posteromedial corner
2. Anteromedial rotational instability (AMRI)
Assessing for injury to posteromedial corner
a) valgus stress test with foot external rotated (see medial gapping with forward subluxation of the anteromedial tibia)
b) anterior drawer test at 90o with foot externally rotated (again will see forward subluxation of the anteromedial tibia)
Posteromedial corner review article
3. Assess ACL / PCL
MCL Grading
Fetto and Marshall Clin Orthop 1978
Grade I / Pain at 30° flexion no opening
Indicates sprain but no tear of MCL
Grade II / Some laxity at 30° flexion, none in full extension
Partial tear of MCL
Grade III / Laxity in full extension
Complete tear of MCL and posteromedial corner
Possible disruption to ACL / PCL

Grade III MCL - opening in full extension
Associated Injuries
1. ACL
- 60% of ACL injuries involve an injury to the superficial MCL
2. Posterior oblique ligament
- 99% of patients with grade III MCL injury had POL injury
2. Meniscus
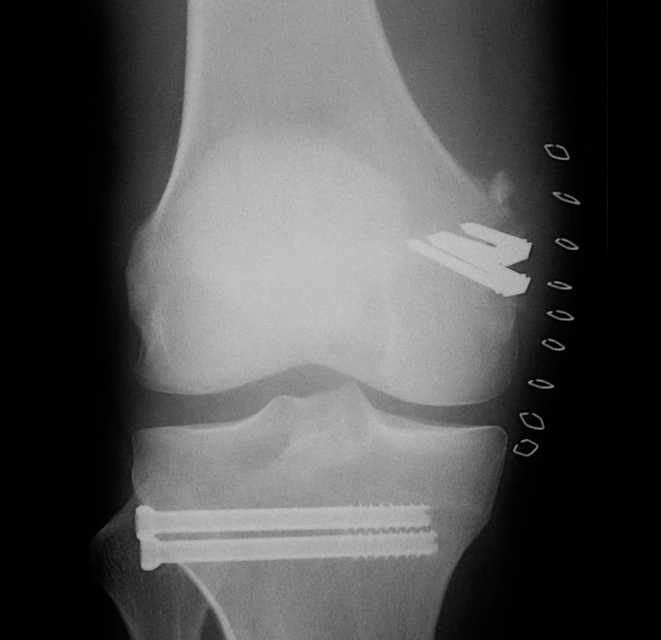
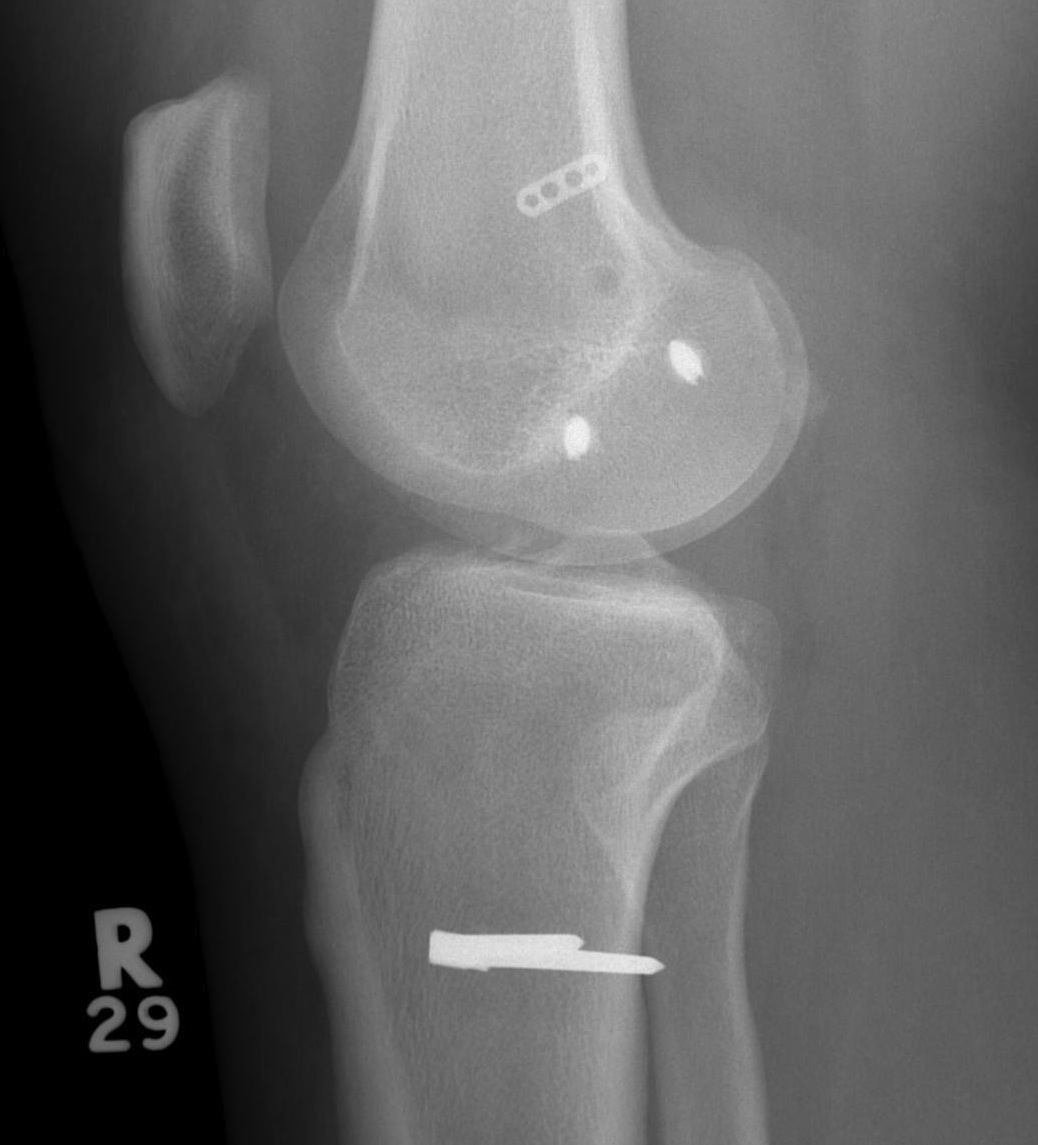
X-ray
Usually normal in acute injury
Bony avulsions (rare)

Bony avulsion of MCL on femoral side
Pellegrini-Stieda Lesion
- calcification at insertion of femoral MCL
- indicative of chronic injury

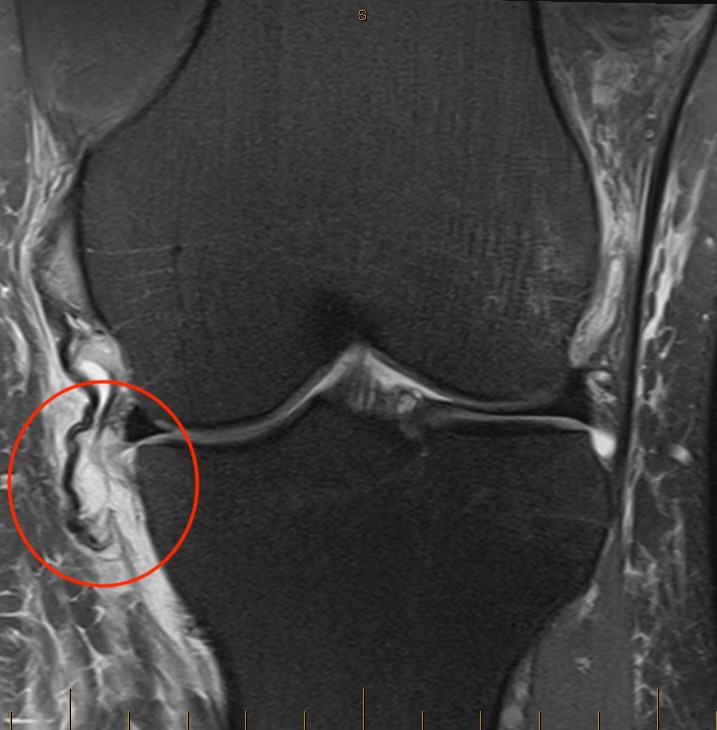
MRI
Classification
Grade I: intact ligament with periligamentous oedema
Grade II: partial tearing with surrounding oedema
Grade III: complete ligament tear
Sites
Femoral avulsion
Midsubstance
Tibial side: wave sign, ensure that the MCL is no flipped above pes anserinus as will not heal (analogous to Stener lesion)


Acute femoral avulsion
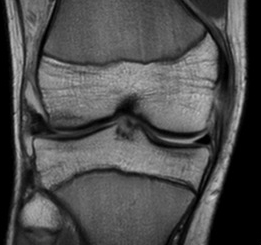

Midsubstance MCL tears

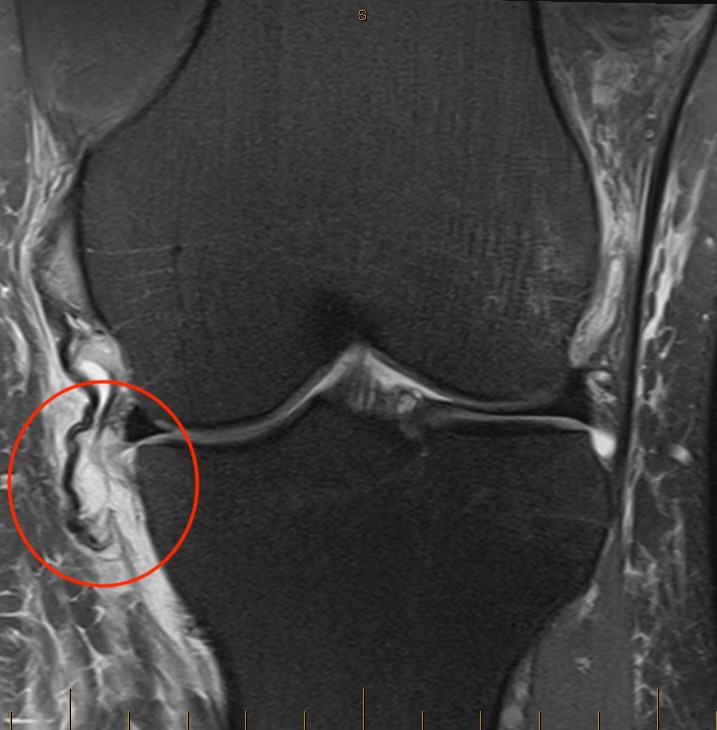
Wave sign indicative of tibial avulsion, with ligament retracted above pes anserinus / hamstring tendons
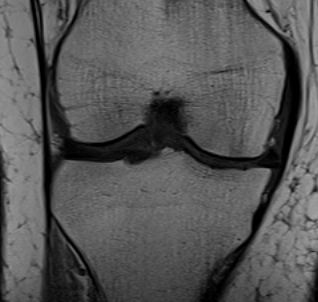

In the chronic setting see thickening of the MCL
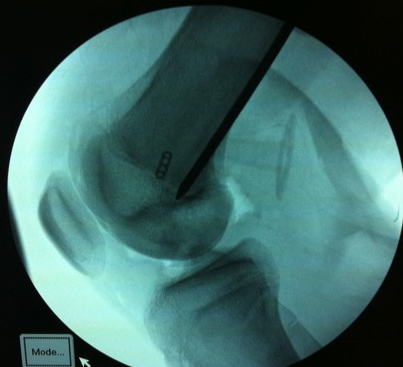
Arthroscopy
Findings
- medial drive through sign
- excessive opening of medial compartment
- may see lift off of the medial meniscus with injury to deep MCL / meniscotibial ligament
- may see injury above medial medial meniscus with injury to deep MCL / meniscofemoral ligament
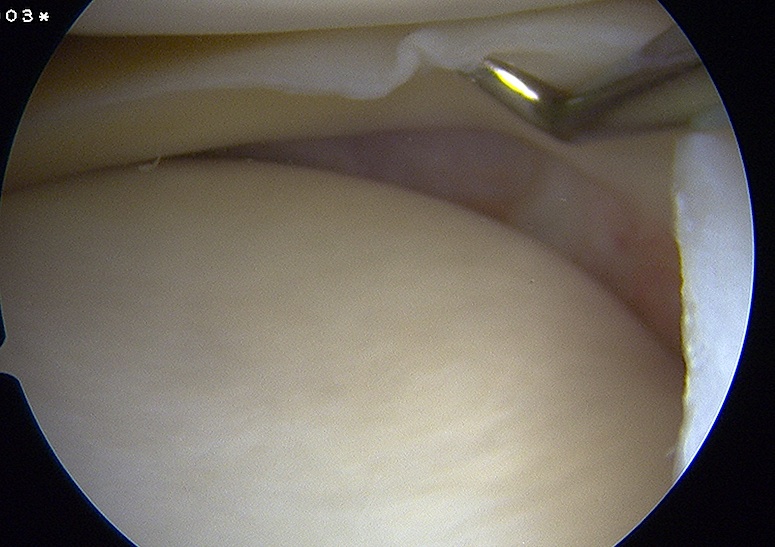
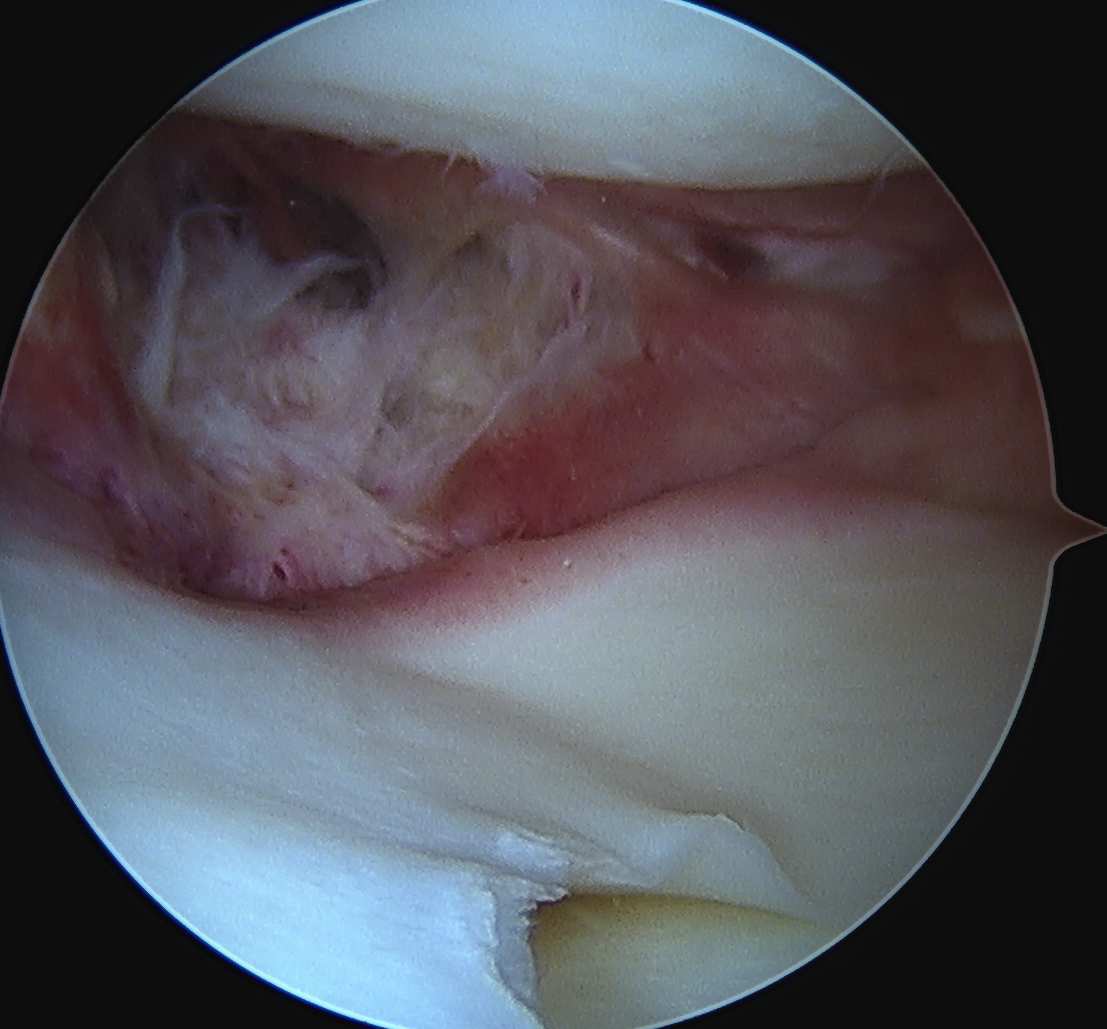
Meniscotibial ligament injury Meniscofemoral ligament injury
Isolated MCL Management
Non operative Management
Indication
- isolated injury to MCL (grade I / II)
- no ACL / PCL / posteromedial corner / meniscal injury
- no displaced tibial avulsion of MCL
Grade I / II
Control pain & inflammation
- RICE / analgesia / weight bear as tolerated
- muscle-strengthening exercises once FROM
- begin jogging once pain free
- grade I: typically, 1 - 3 weeks return to sport
- grade II: can be 6 - 8 but sport dependent
- usually, a brace is not necessary
- 130 MCL injuries UEFA elite soccer players
- use of brace in grade II associated with longer return to play
Grade III
Ensure no concomitant injury
Consider a hinge brace
Can consider extension block but risk stiffness
Combined Ligament Injury
ACL + MCL
Grade II MCL
Millett et al J Knee Surg 2004
- early ACL reconstruction with non operative management MCL in 18 patients
- at 2 year follow up no graft failure or valgus instability
- 3 year follow up of ACL reconstruction with grade II MCL treated nonop
- no impact on AP instability on KT-1000 at 3 year follow up
- all patients had some residual ML instability on Telos stress xrays
Grade III MCL
Halinen et al. Am J Sports Med 2006
- RCT of acute ACL reconstruction in patients with grade III MCL
- early ACL reconstruction
- operative v non operative management of MCL in 47 patients
- no difference in the two groups with regards outcome or stability
Westermann et al. Arthroscopy 2019
- MOON group
- 1.1% (27/2586) had grade III MCL with ACL
- 16 managed operatively, 11 managed nonoperatively
- patients managed operatively had worse outcomes scores both before and after surgery
Operative Management of Grade III MCL injuries
Indications
Displaced bony femoral avulsion
Displaced tibial avulsion above pes anserinus or into joint
Chronic grade III MCL / posteromedial corner injury with instability
Grade III MCL in setting of ACL / PCL ligament injury
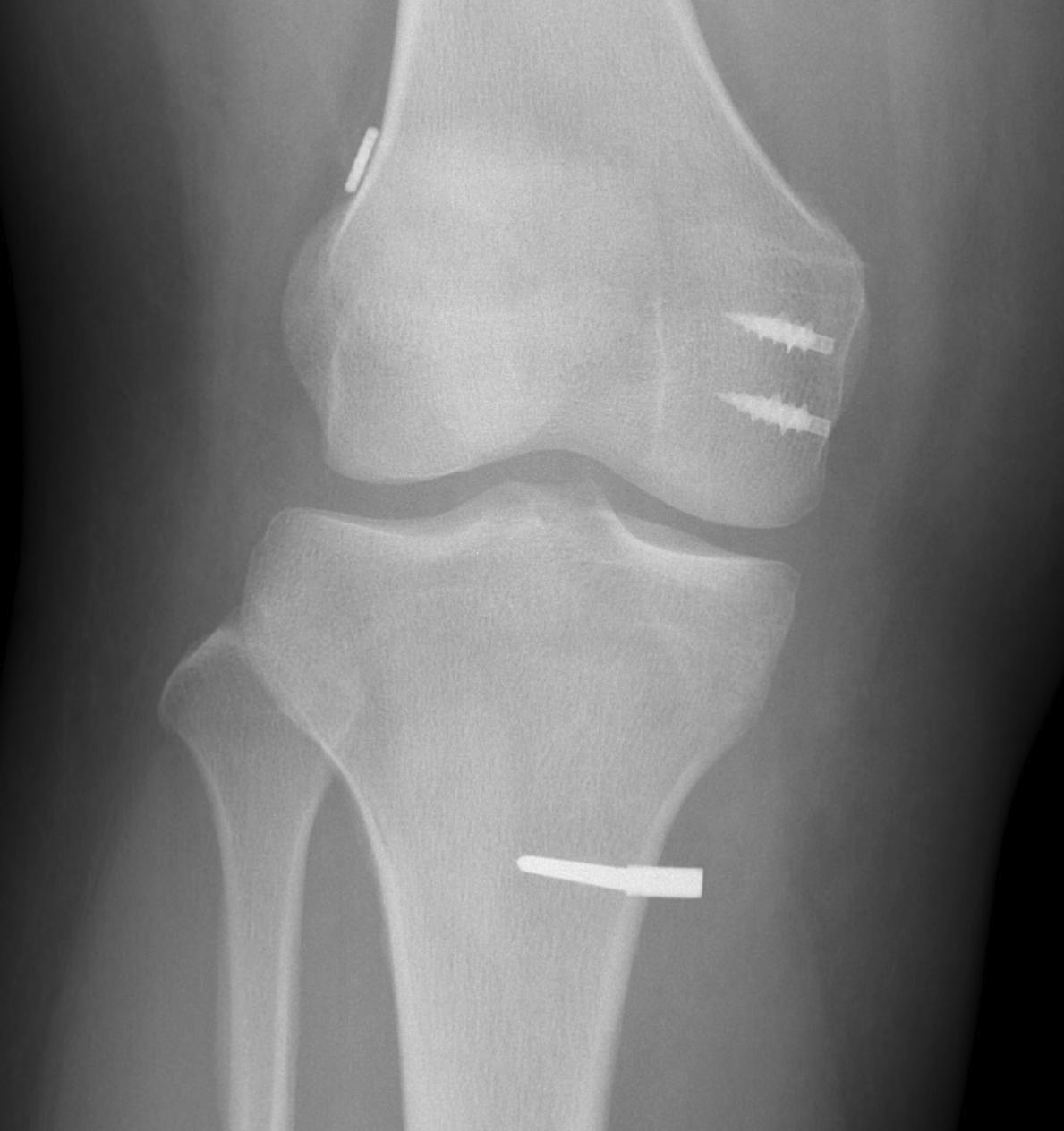
Bony MCL Avulsion
Elevate VMO and repair with staples or screw

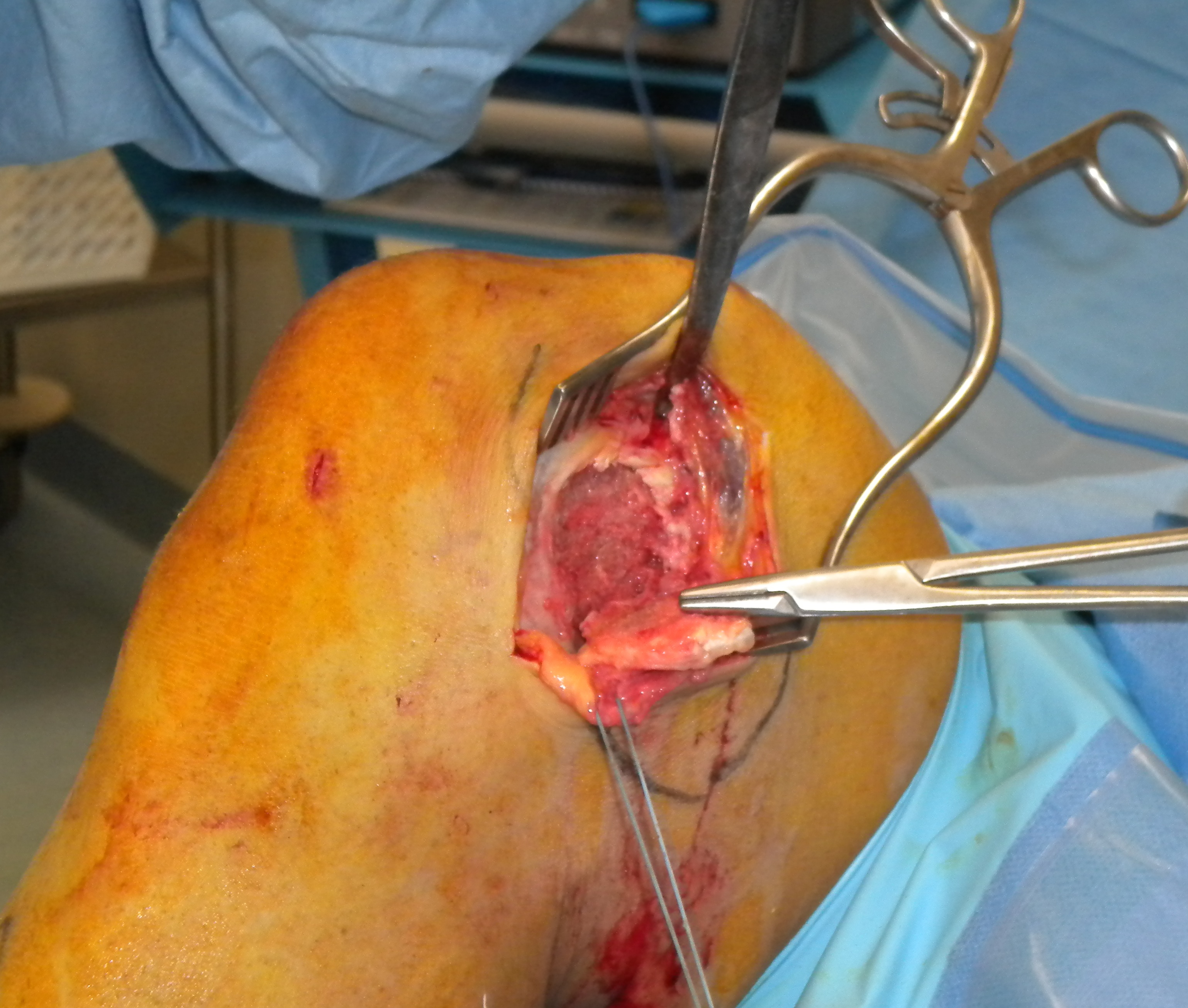

MCL repair
Tibial side
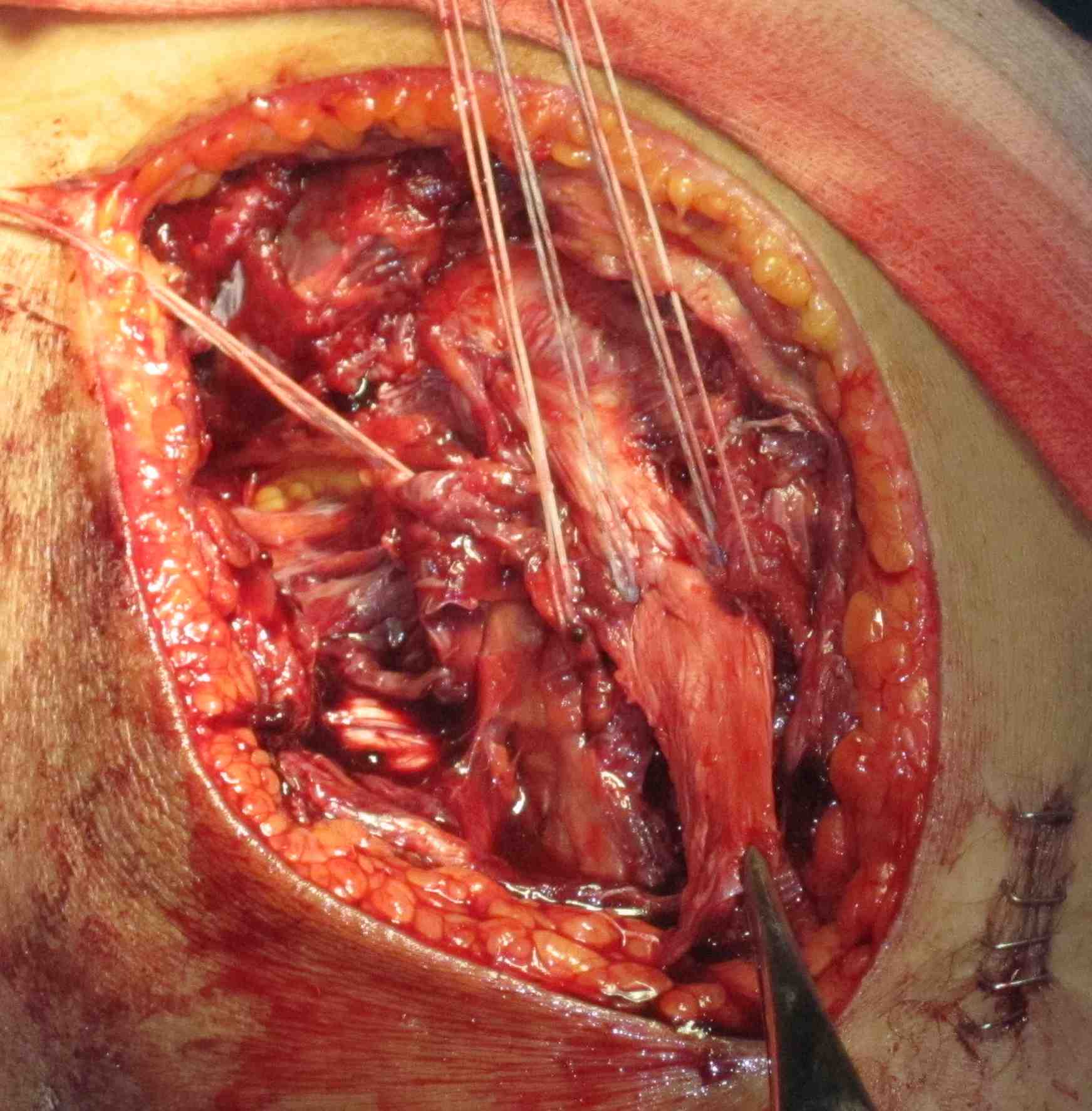
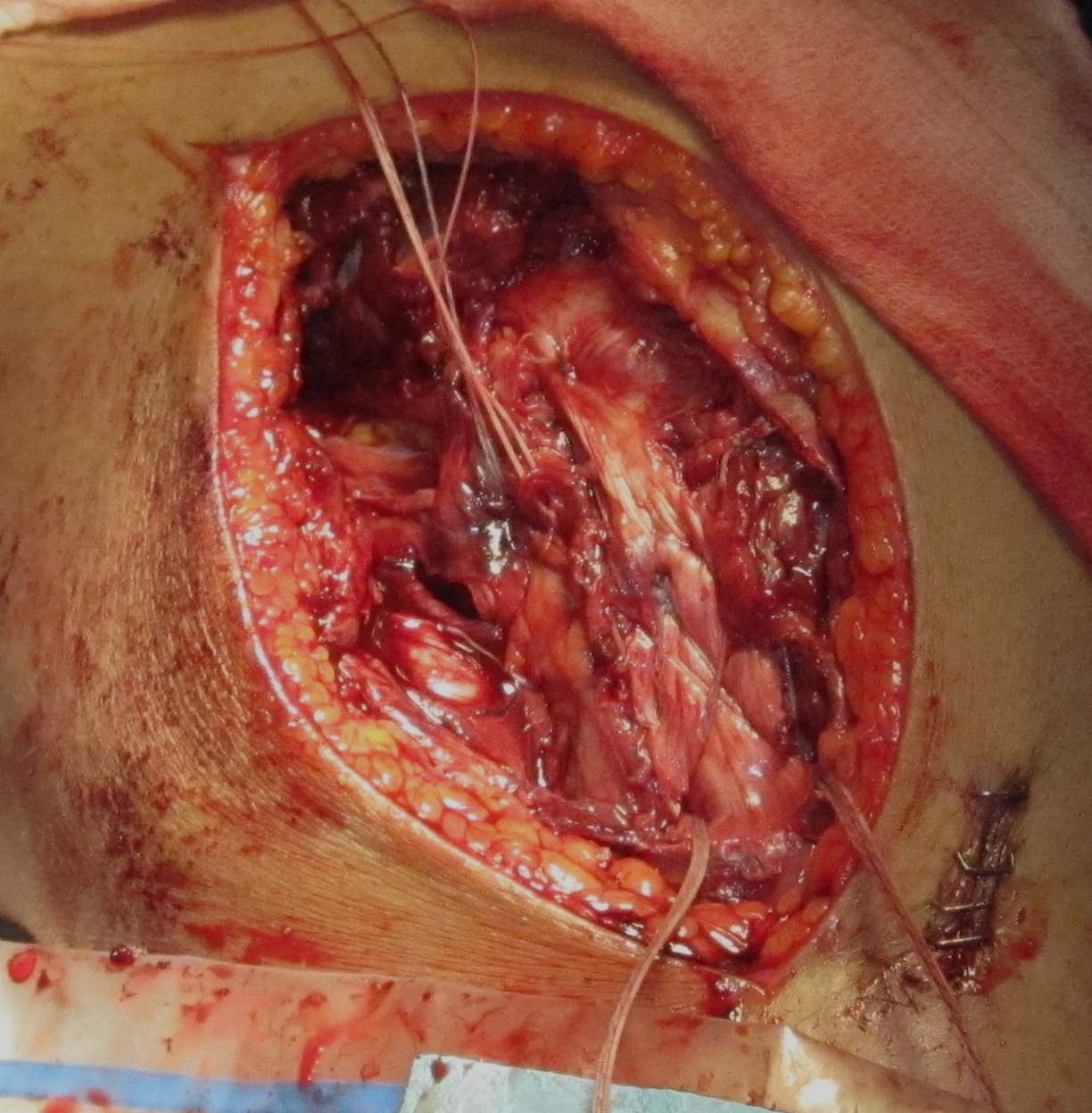
Femoral side
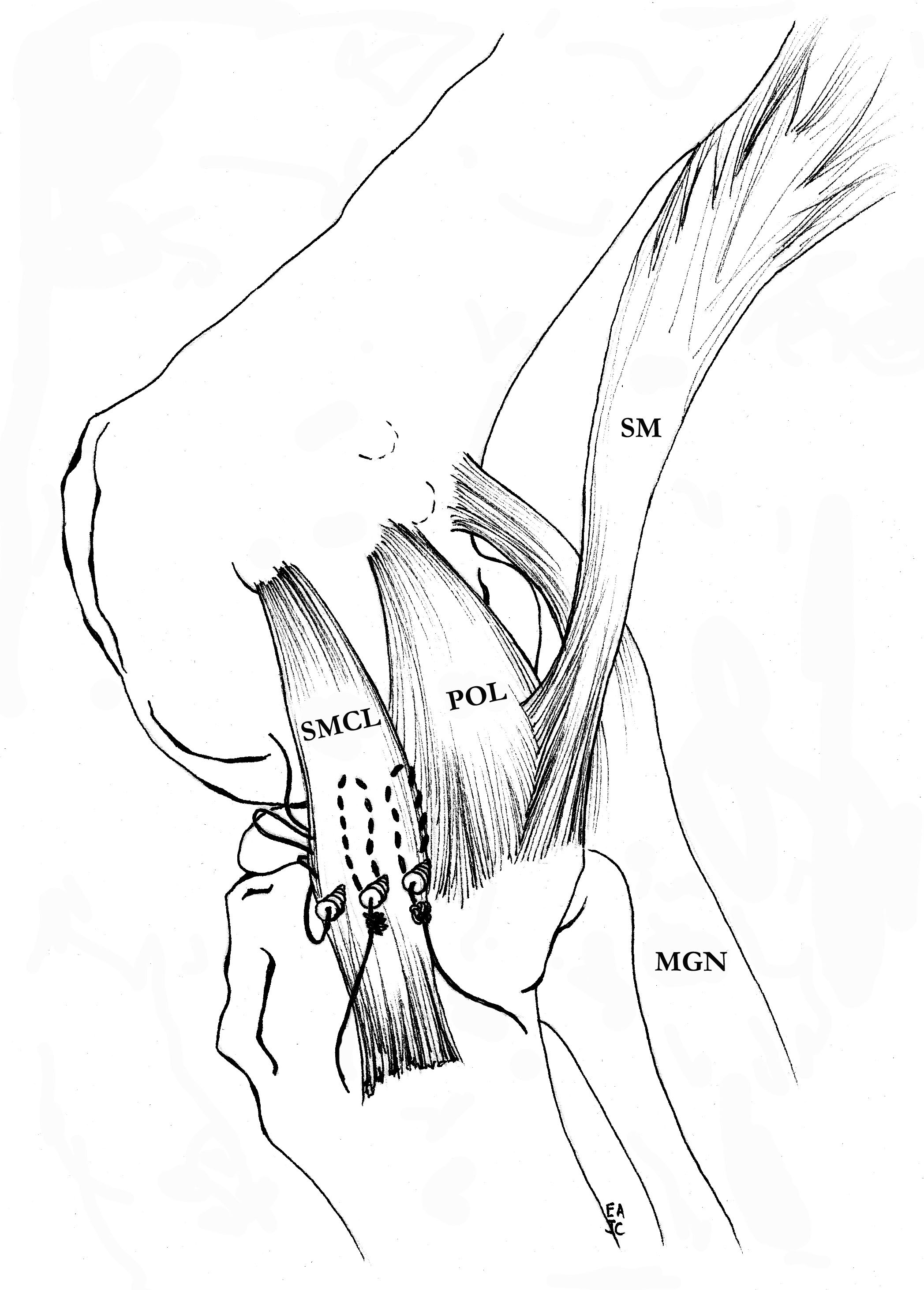
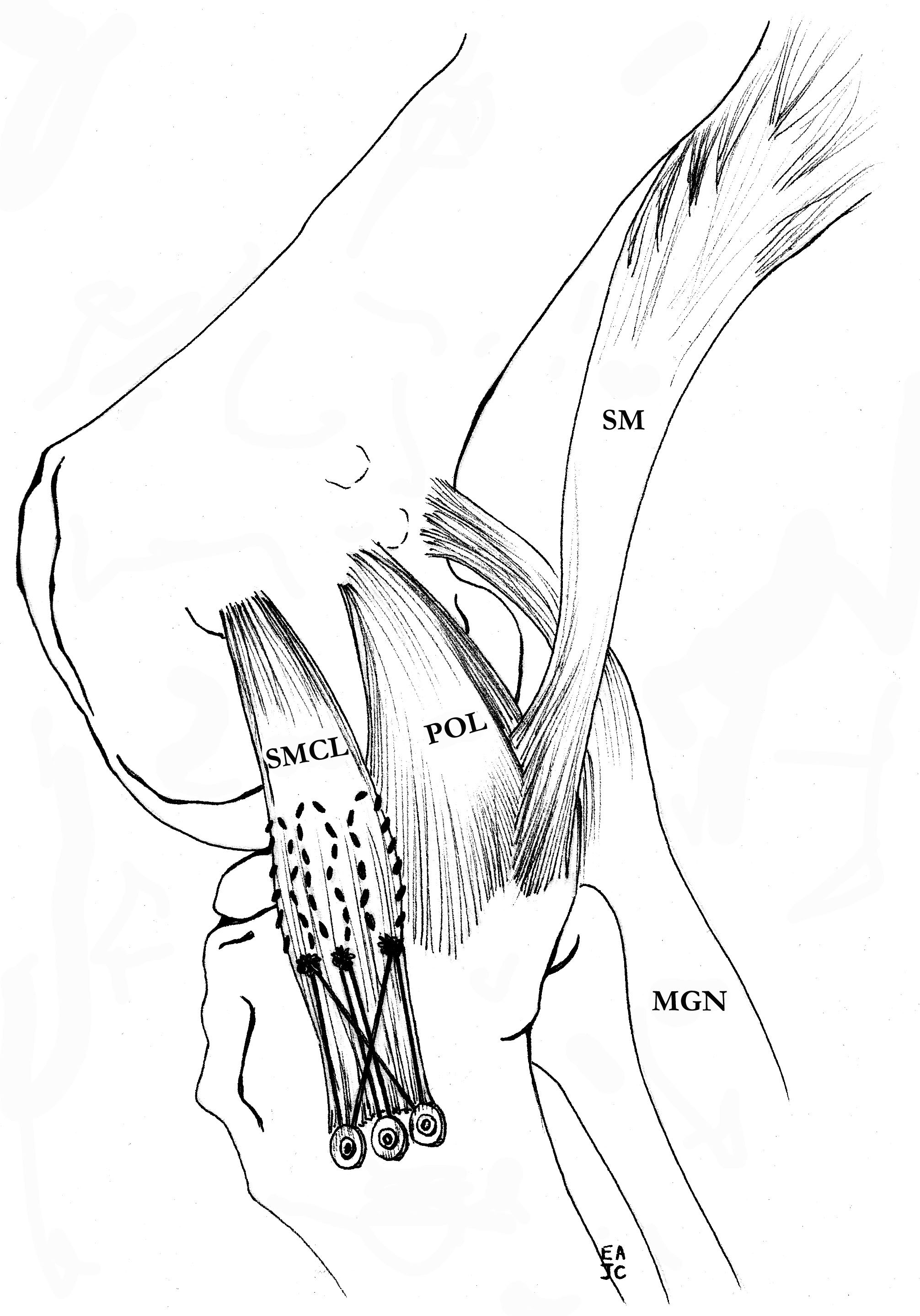
Hughston Procedure
- advance femoral attachment of MCL and POL
- tighten POL anteriorly onto MCL
- consider imbricating semimembranosus to decrease slack
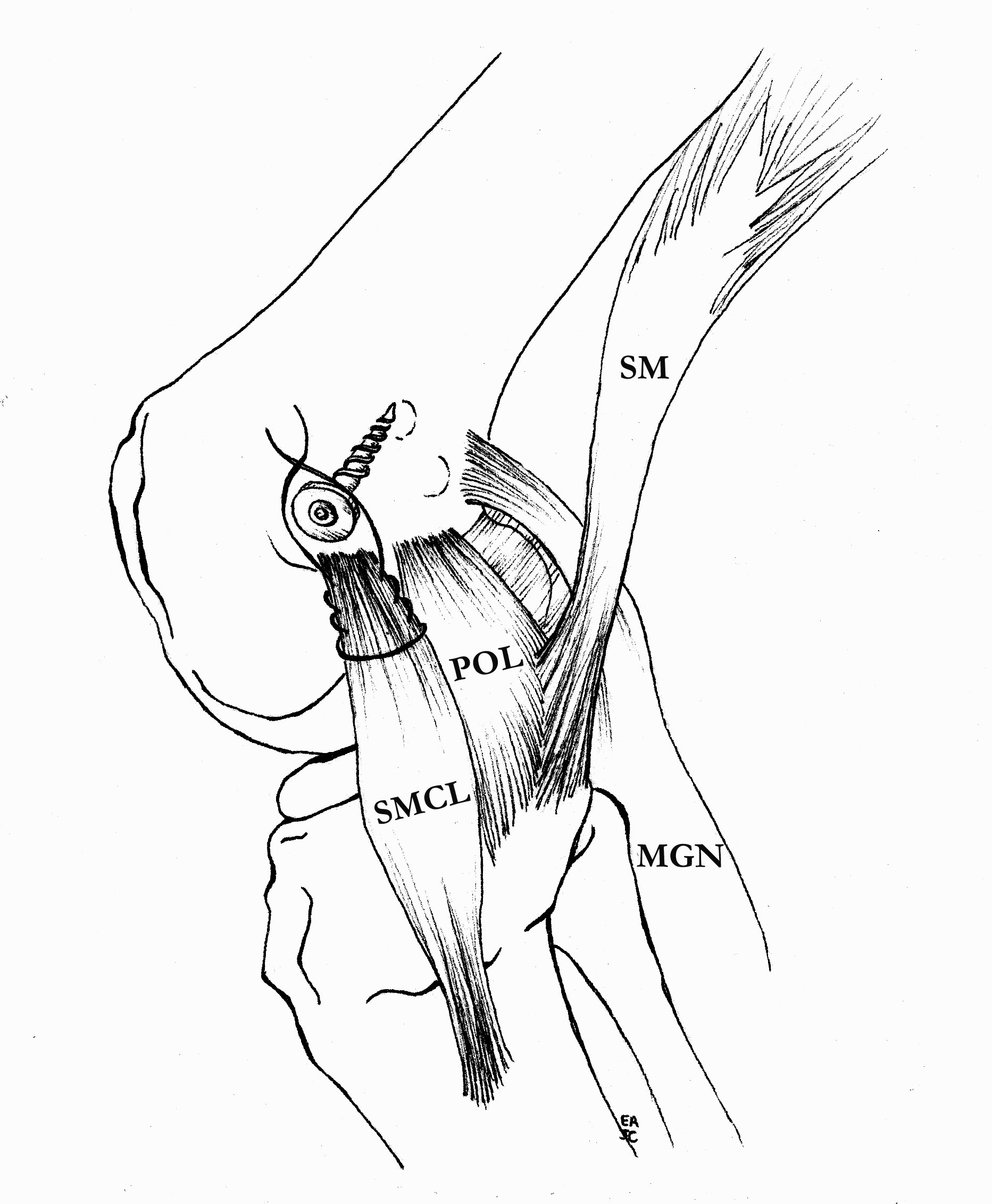
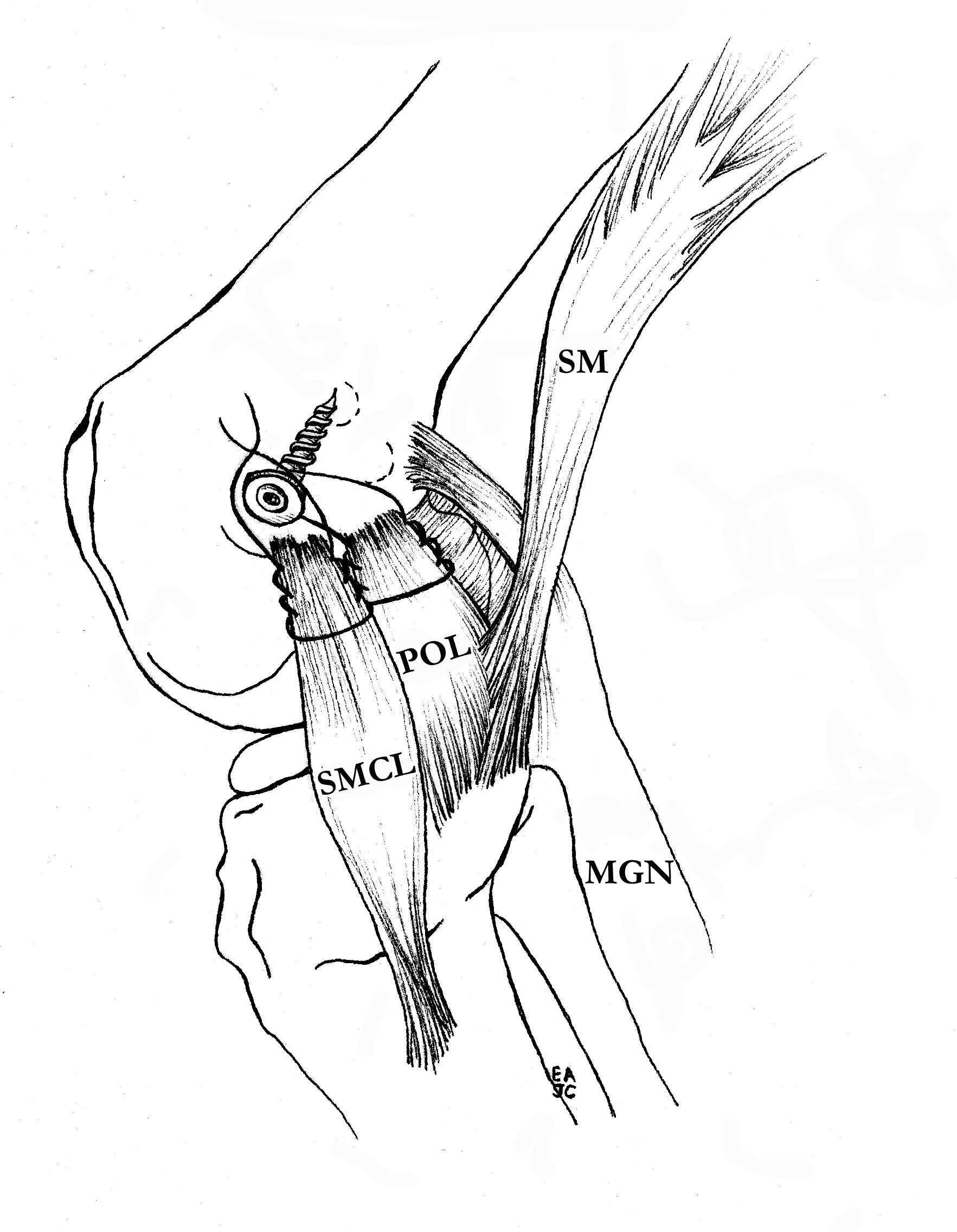
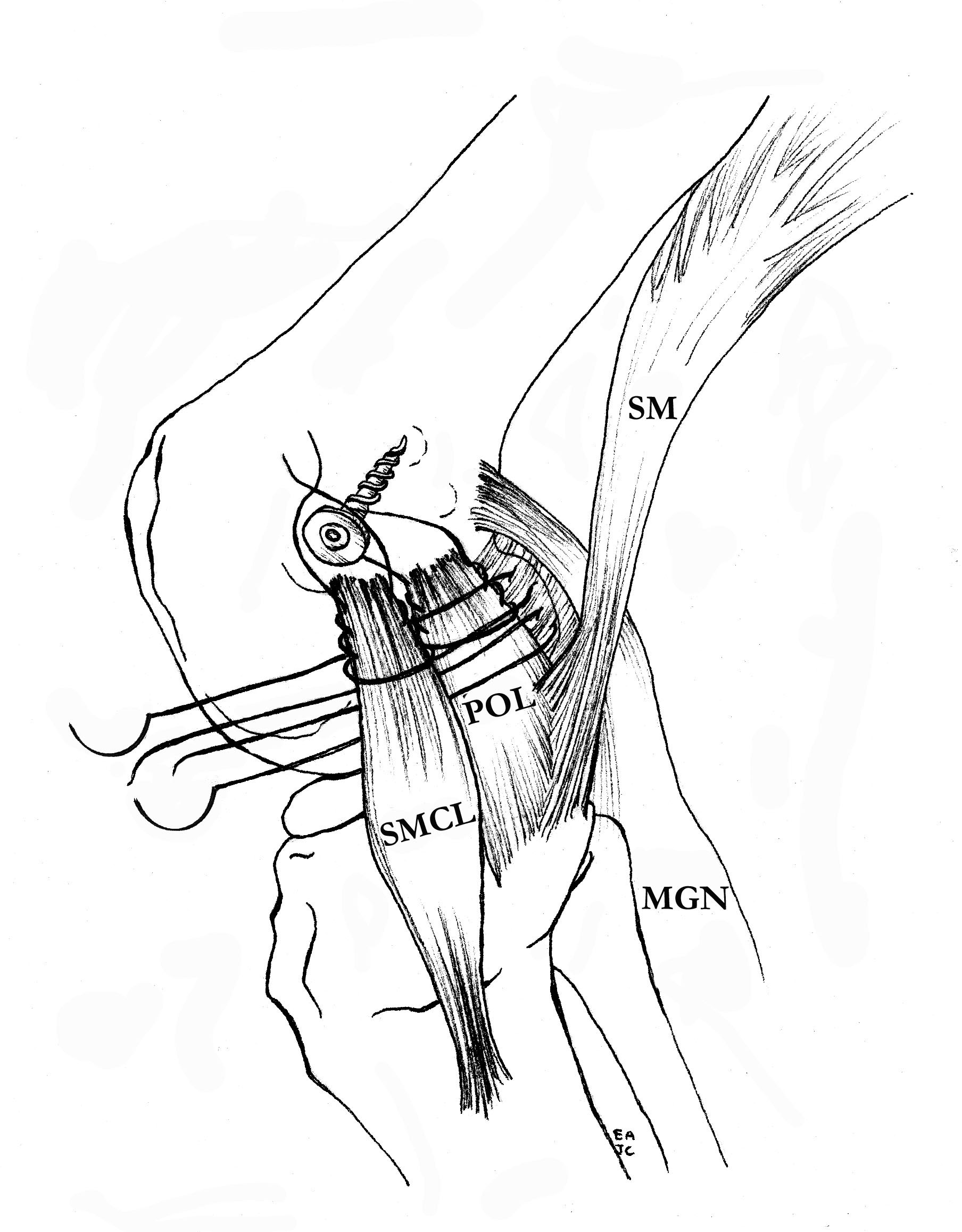
Advancement of proximal MCL / POL with screw, and imbrication / tightening of POL
Tightening of proximal MCL / POL with sutures


Advancement of femoral MCL and staple / suture anchor fixation
Outcomes
Delong et al. Arthroscopy 2015
- systematic review of all repair techniques
- 16 papers with 355 knees
- 75% had side to side difference of < 3 mm
- 6% failure rate
3. Reconstruction of MCL and posteromedial corner
A. Single bundle anatomic allograft MCL reconstruction (no POL)


Bony fixation with screw of femoral side, screw and soft tissue washer fixation on tibial side
Marx technique MCL reconstruction with tendoachilles allograft PDF
Marx technique MCL reconstruction with tendoachilles allograft Vumedi
Femoral attachment
- 4 mm proximal and posterior to medial epicondyle
- 40o anterior to avoid notch
- 40o proximal to avoid PCL tunnel
Tibial attachment
- 6 cm from joint line
- just posterior to pes attachment


B. Single bundle anatomic hamstring autograft MCL reconstruction (no POL)

Technique
- harvest both hamstrings and leave attached distally
- re-routed more posteriorly on tibia around screw / soft tissue washer or with anchors (recreates tibial insertion)
- femoral attachment is 12 mm distal and 8 mm anterior to adductor tubercle (attachment of adductor magnus)
- femoral attachment is 3 mm proximal and 4 mm posterior to femoral epicondyle
- isometric centre on fluoroscopy is line of intersection of posterior femoral condyle and blumensaat's line
- drill femoral tunnel and fix with screw
LaPrade surgical technique PDF
C. Double bundle anatomic reconstruction of MCL and POL
Technique
- use separate hamstring tendons to recreate MCL and POL
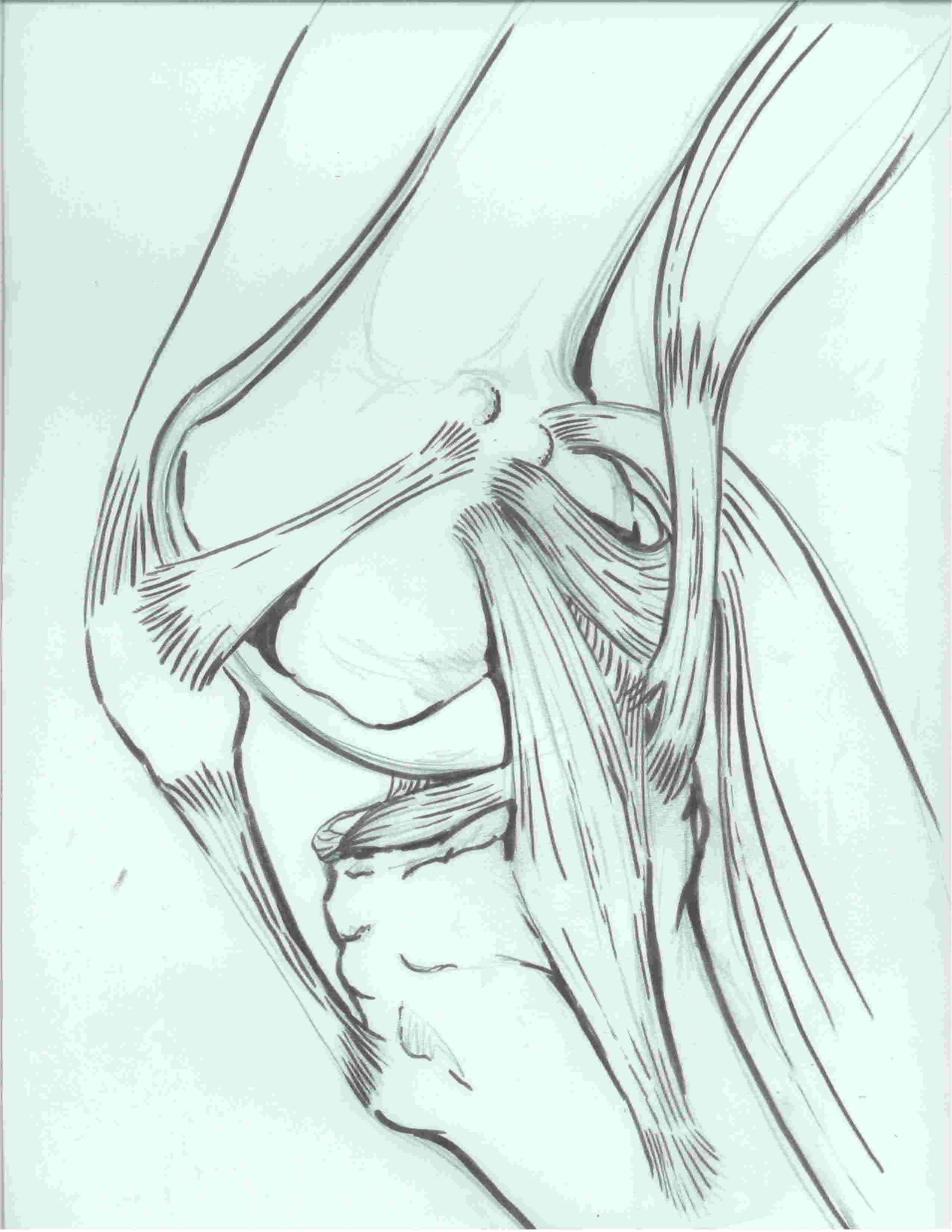
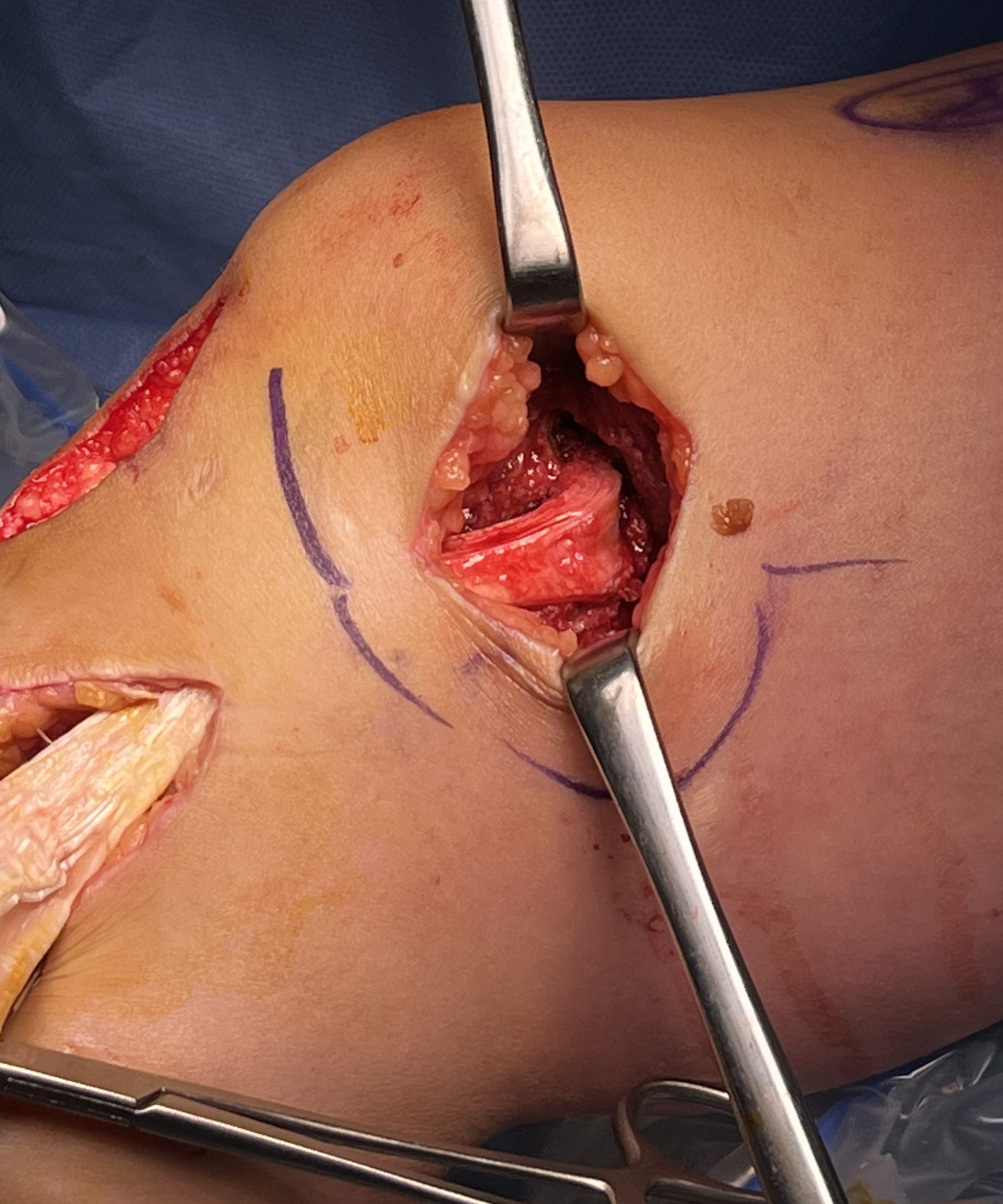
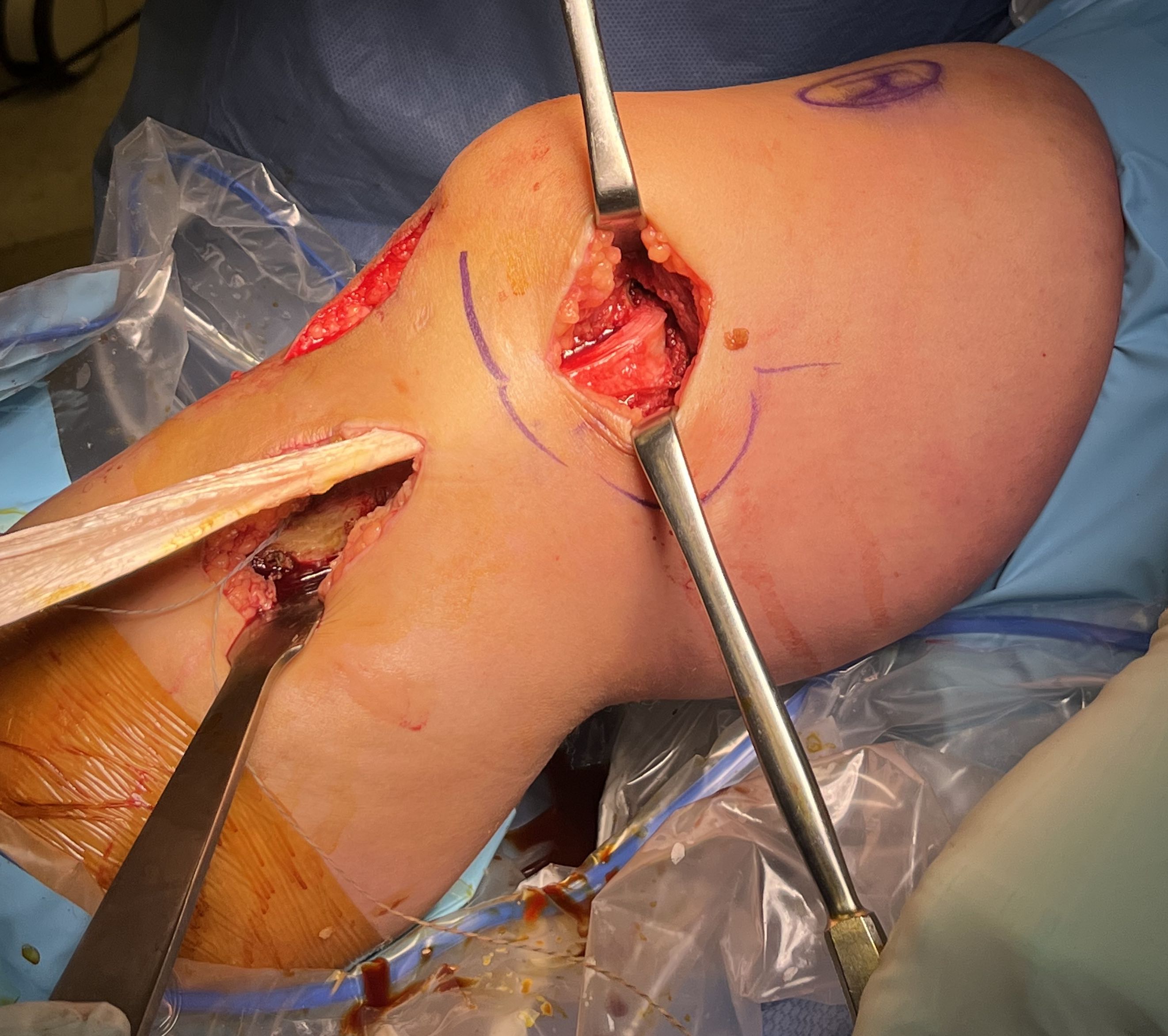
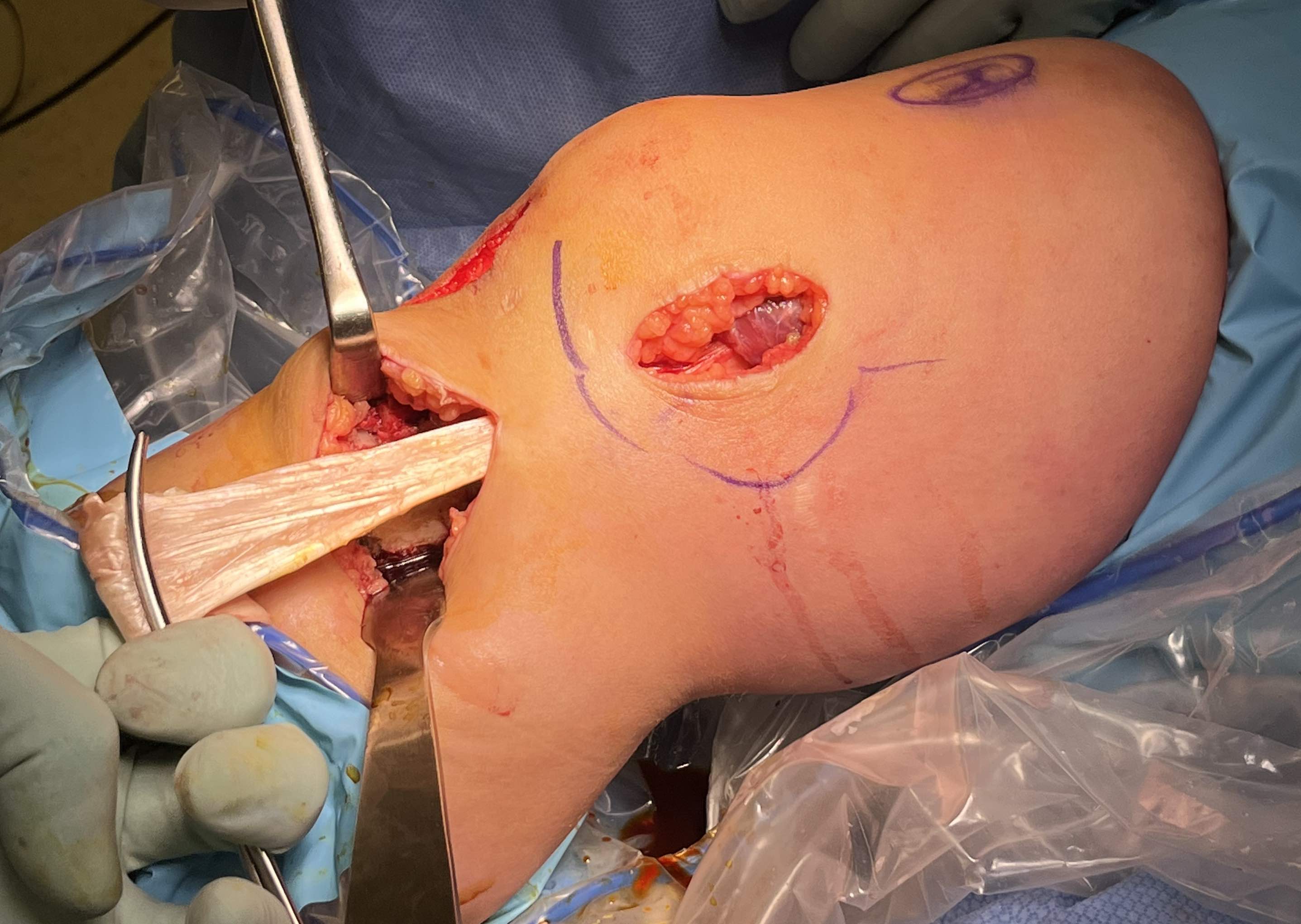
Surgical Approach to Medial Knee
Position
- knee flexed to 90o, over bolster
- tourniquet
- sandbag under hip
Incision
- hockey stick medial incision
- halfway between borders of tibia
- extends proximally to adductor tubercle
- distally to pes anserinus
Superficial dissection
- protect the saphenous nerve and small saphenous vein
- emerges from between sartorius and gracilis
- divide medial patella retinaculum from VMO down
- divide sarfascia over pes anserinus
- reflect pes anserinus inferiorly
Deep dissection
- elevate VMO to identify proximal insertion of superficial MCL
- expose superficial MCL running from medial epicondyle down to tibia under pes
- popliteal oblique ligament and semimembranosus are posterior to MCL
- can expose posterior capsule by carefully reflecting medial gastrocnemius posteriorly
