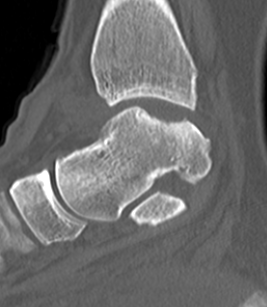
Osteochondral defects

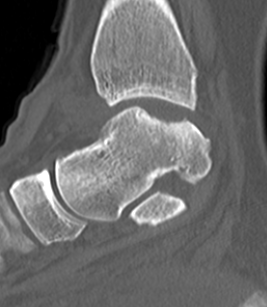
Definition
Defect of cartilage +/bone
Typically on talus
Options

Defect of cartilage +/bone
Typically on talus
Indication
Bony defects > 30 %
Options
- Latarjet - may be insufficient for lesions in the region of 50%
- Iliac crest - associated with high incidence of OA
- distal tibial allograft - radius of curvature matches glenoid highly
Bone healing requires 3 things
- osteoconduction - scaffold / matrix
- osteoinduction - growth factors
- osteogenesis - cells to produce osteoid
Definition
- property of a matrix that supports the attachment of bone forming cells for subsequent bone formation
Substances
1. Isolated LCL injury
2. Isolated Posterolateral Corner
3. PCL + posterolateral corner
4. ACL / posterolateral corner
5. ACL / PLC / posterolateral corner
Levy et al. Am J Sports Med 2010
- failure in 4/10 knees treated with acute primary repair
Usually occurs in patients over 60
- due to decreased vascularity & collagen weakness
Younger patient on steroids / growth hormone
Occasionally occurs in young athlete with excessive contracture
Often preceded by quadriceps tendinosis
- reported higher incidence with immediate reconstruction in acute phase
- reduced by settling inflammation / effusion and obtaining FROM
- always best to delay if not professional athlete
- problematic if patient has locked bucket handle mensical tear
Bottoni et al Am J Sports Med 2008
- RCT of early (average 9 days) v late reconstruction (average 85 days)
Graft Preparation

Defrost
- in 2 litres normal saline
- can add vancomycin powder
Choose which part of graft to use
- usually central third
- can take either side
- try to leave sufficient graft in case of disasters
- i.e. dropping or rupturing graft
Good initial results but unacceptably high failure rate with longer follow-up
Problems
1. Too stiff (low ultimate strain)
- poor resistance to abrasion
- ligament failure by attrition most common
2. Recurrent synovitis, infection, loosening and osteolysis
Rule out infection
Assess rotator cuff / bone stock preoperatively
Approach
- difficult / scarring +++
- very difficult to restore any loss of ROM
Removal of prosthesis
Glenoid
- may not be able to revise
Humeral component
- long stem
Rule out infection
- CRP / ESR
- ultrasound or xray guided aspiration