

Definition
Chronic instability due to rupture of one or more of the lateral ankle ligament
Recurrence risk
Incidence
- sytematic review of 31 studies
- up to 33% patients still have pain 1 year after acute ankle sprain
- up to 34% risk of recurrent ankle sprain
Factors
Thompson et al BMC Musculoskeletal Disord 2017
- prognostic factors associated with poor recovery after acute ankle sprain
- female, increased severity of initial injury
- pain at 3 months, resprain within 3 months
- increase number of ligament injuries + bone bruise on MRI
Osteoarthritis
Lofenberg et al Foot Ankle Int 1994
- patients with chronic ankle instability at 20 year follow up
- 6/46 (13%) had OA on xrays

History
Swelling
Instability - giving way with activity & walking on uneven ground
Chronic pain is unusual with isolated chronic instability (see Bone School section)
- osteochondral fracture / injury
- syndesmosis injury
- lateral talar process / anterior calcaneal process fracture
- peroneal tendonitis / subluxation / dislocation
- sinus tarsi syndrome
Examination
| Anterior drawer | Talar tilt |
|---|---|
| Assess ATLF | CFL test / subtalar instability |
|
10° plantarflexion neutral rotation Draw talus anterior to tibia |
10-20° plantarflexion Ankle inversion |
| > 3mm difference to other ankle | > 20o difference to other ankle |
 |
 |
Xrays
Osteochondral lesions

Loose bodies


Stress Xrays
| Anterior drawer | Talar tilt |
|---|---|
| Assess ATLF | CFL test / subtalar instability |
|
10° plantarflexion neutral rotation Draw talus anterior to tibia |
10-20° plantarflexion Ankle inversion |
| > 3mm difference to other ankle | > 20o difference to other ankle |
 |
 |
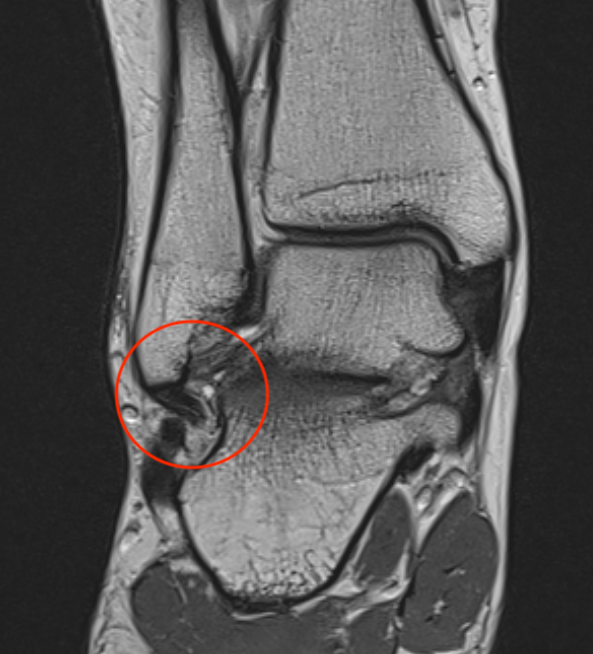
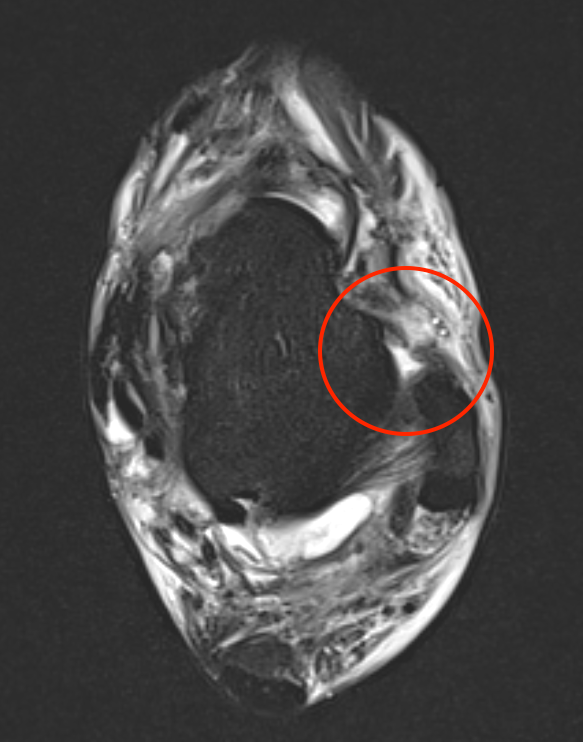
MRI
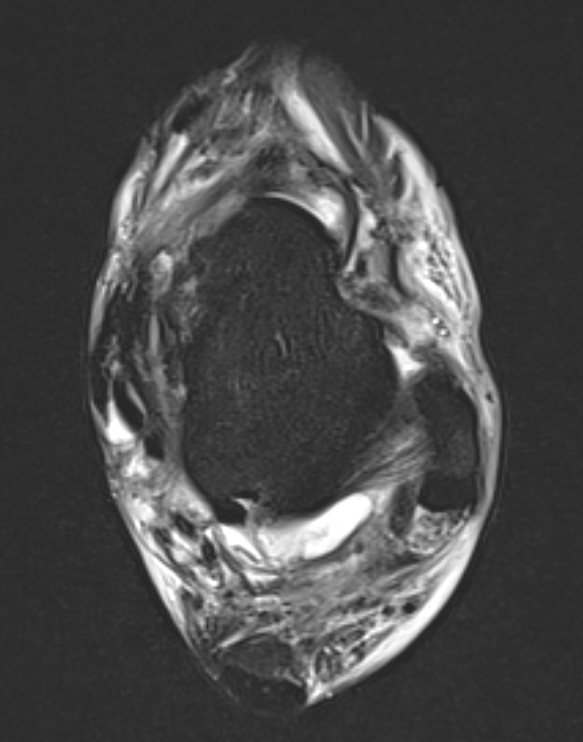
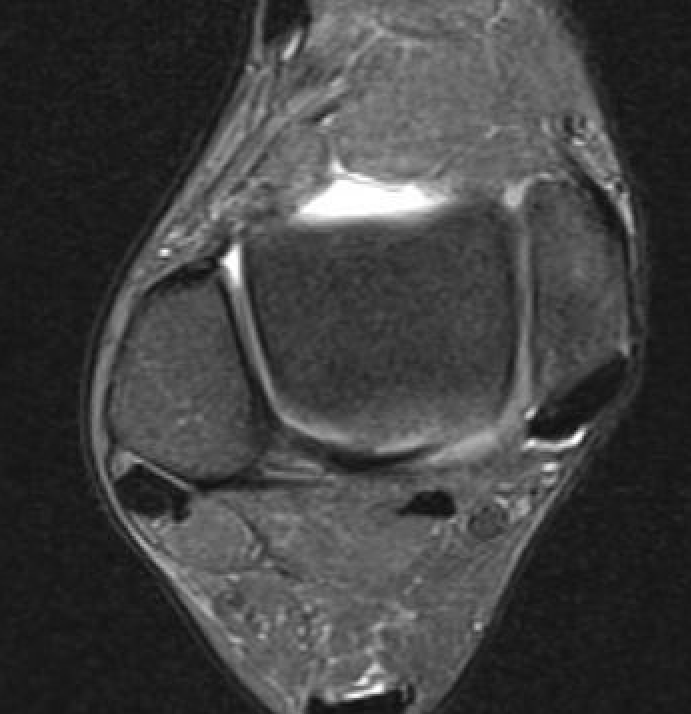

ATFL tear
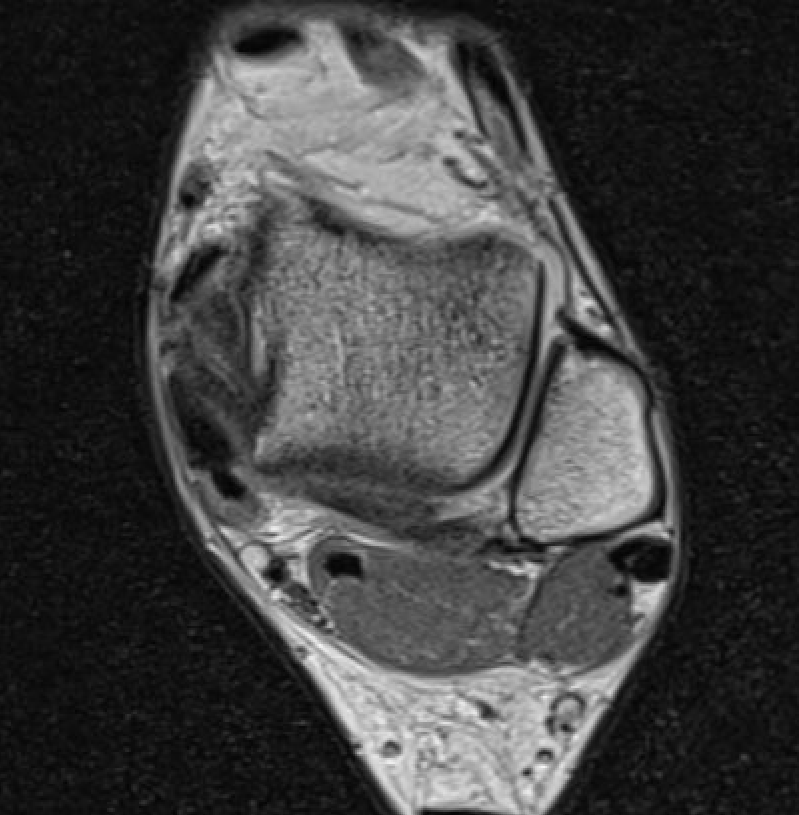

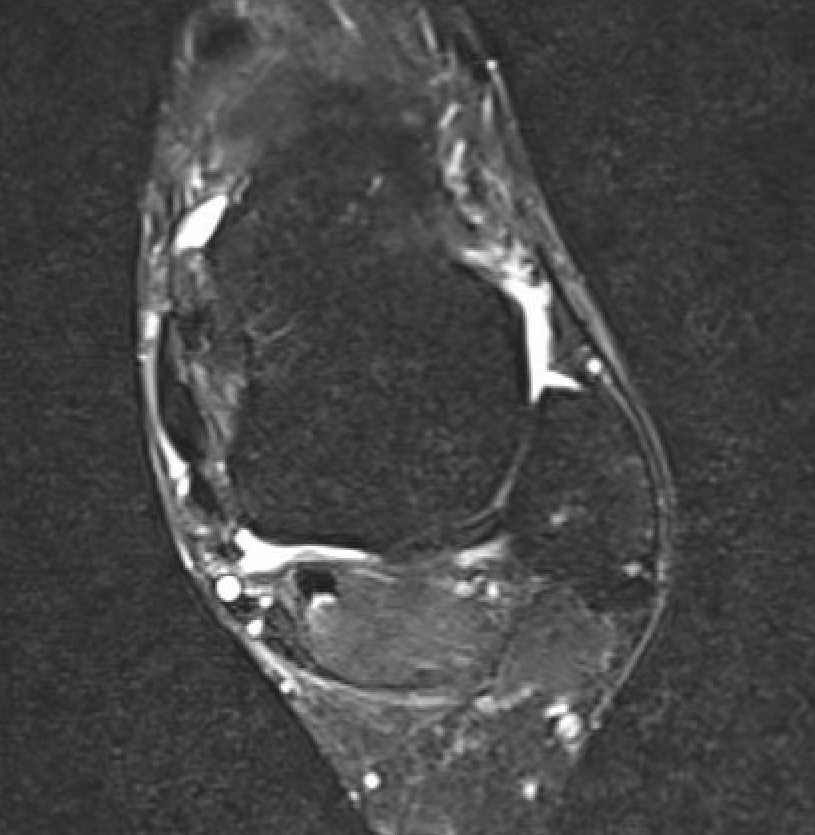
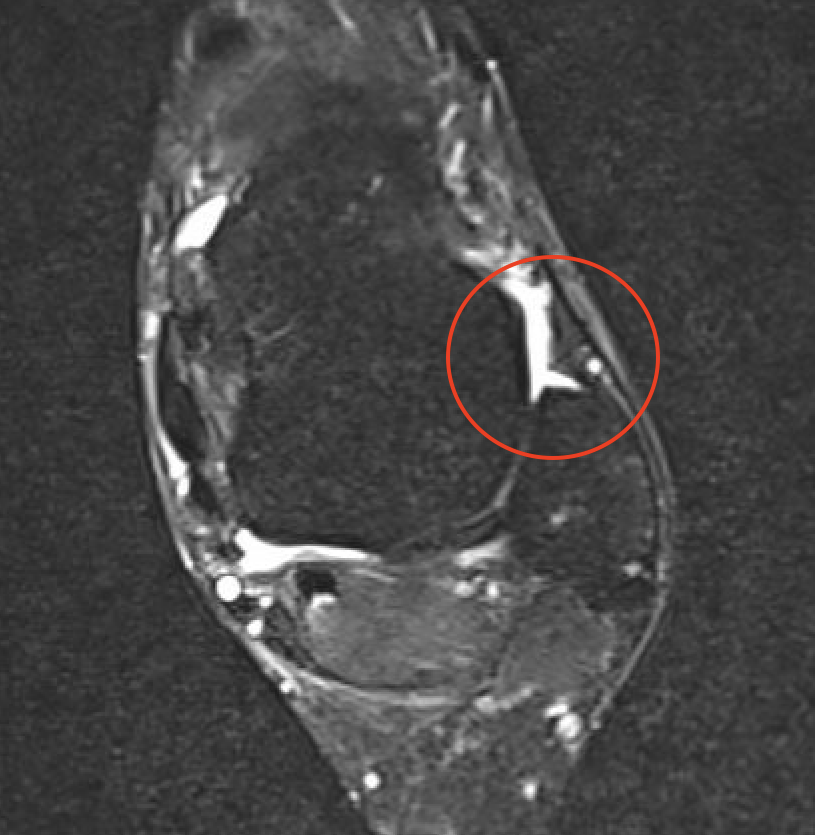
ATFL tear




CFL tear
Management
Non-operative
Bracing / taping
- systematic review of effect of kinesio taping for chronic ankle instability
- evidence for gait improvement and reduced inversion/eversion
Rehabilitation exercises
Neuromuscular training / proprioception / balance / strengthening
- systematic review of multimodal rehabilation for chronic ankle instability
- evidence of efficacy of 4 week programs
Operative Management
Indication
Ongoing instability
Options
Anatomic repair - modified Brostrom
Anatomic reconstruction - autograft / allograft reconstruction ATFL / CLF
Non anatomic reconstruction - peroneus brevis tenodesis
Results
Vopat et al Arthros Sports Med Rehab 2022
- systematic review of repair versus reconstruction versus suture tape augmentation
- 41 studies and 2000 patients
- complication rate: reconstruction 3%, repair 4%, suture tape 11%
- no difference functional outcomes
Anatomic Repair / Modified Brostrom
Concept
Mid substance repair / bony repair
Gould Modification - reinforce ATFL repair with extensor retinaculum
Options
Internal brace / suture tape augmentation
Arthroscopic techniques
Augmentation with non anatomic / peroneus brevis reconstruction
Open technique
Arthrex modified Brostrom surgical technique video
Vumedi open modified Brostrom video
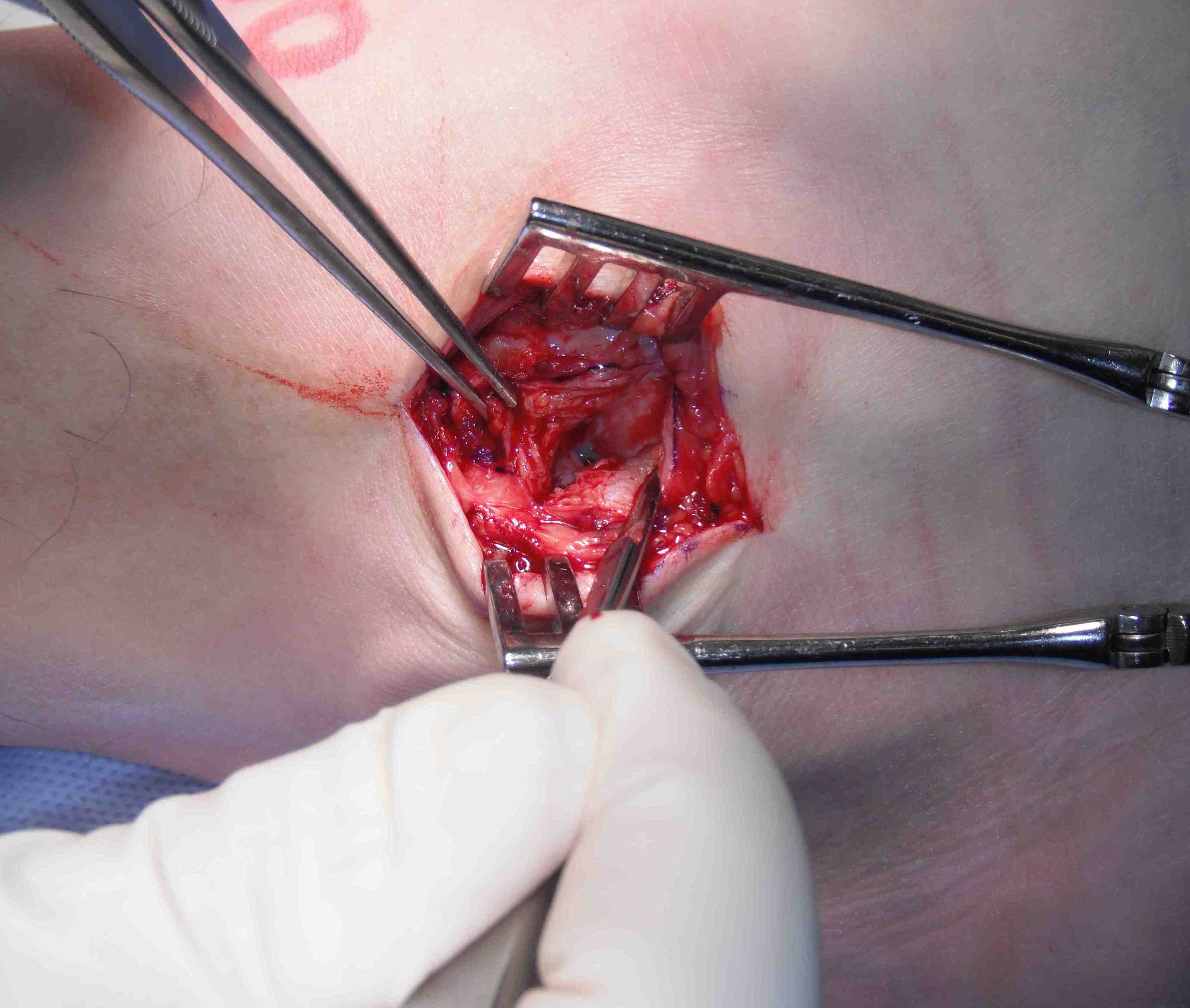
Longitudinal incision anterior to lateral malleolus
- protect branches of superficial peroneal nerve
- expose tissue of ATFL / CFL
- anterior incision between ATFL and CFL to talus
- begins at tip of fibula to talus
- take off fibula as broad / thick flap
- superior flap is ATFL / inferior flap is CFL
- need to protect peroneals with inferior portion of dissection
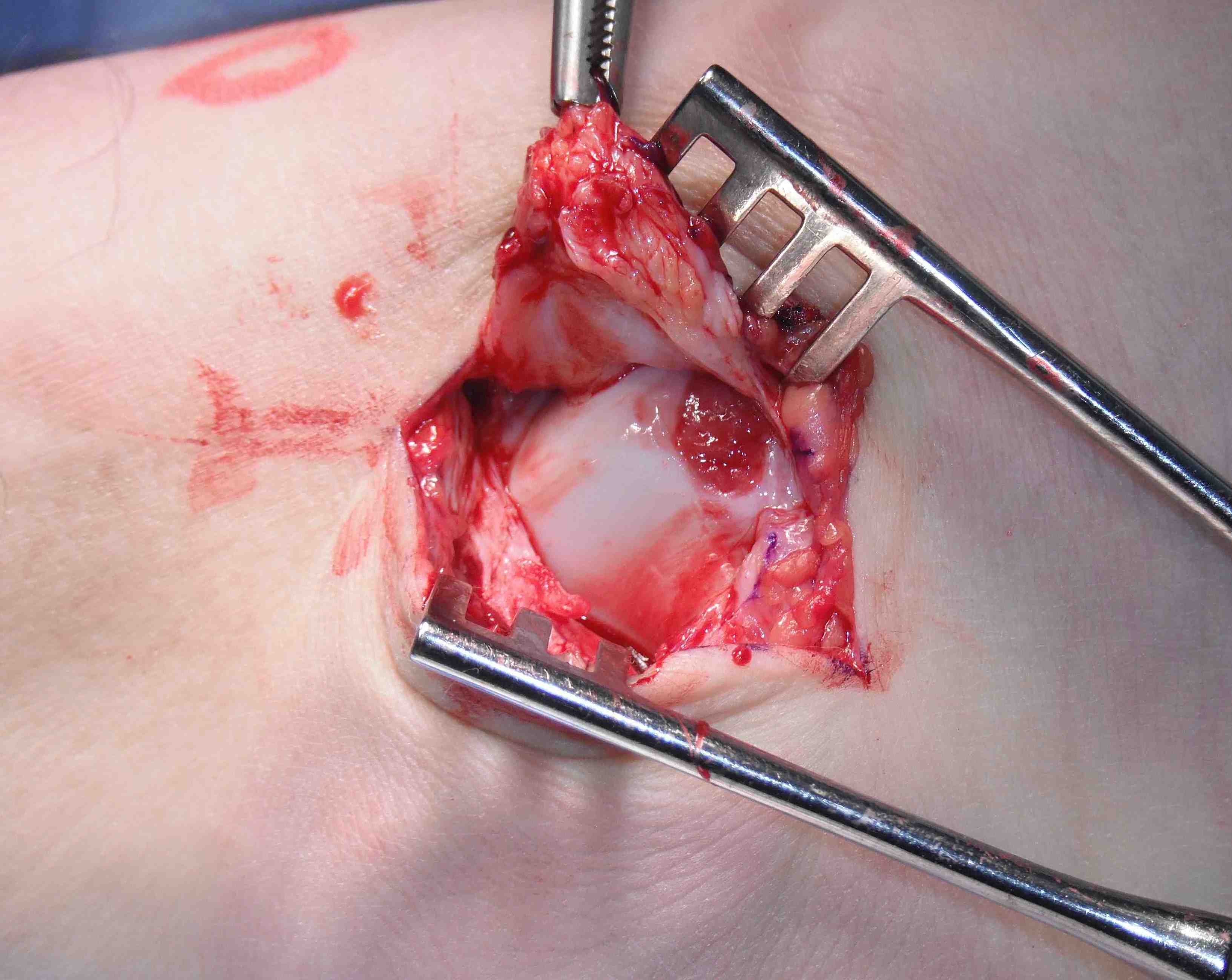
- inspect talus for chondral damage

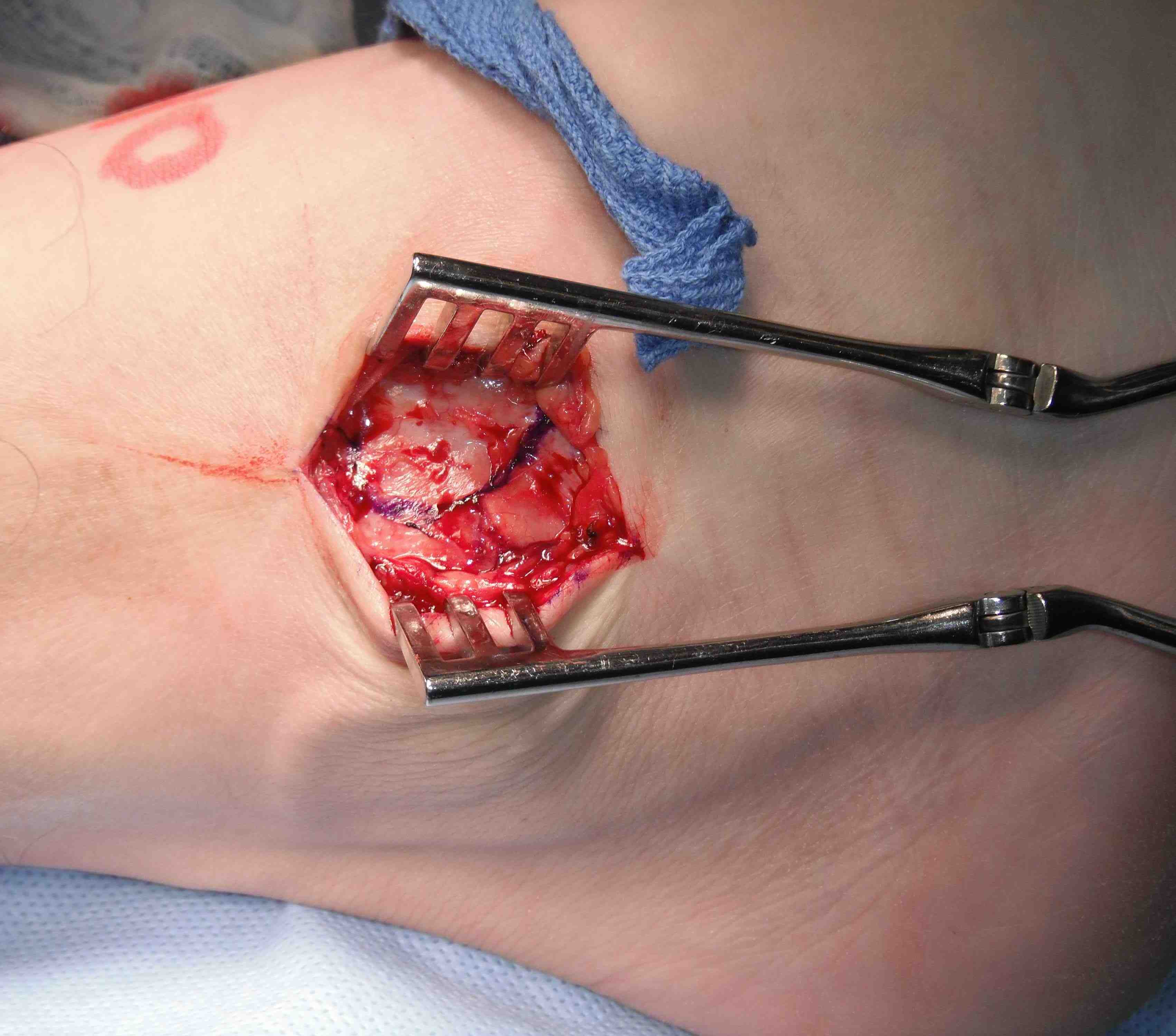

Place foot in eversion and AJ neutral
- 2 x 3.5 mm anchors in fibula
- ensure not in joint and not prominent
- 4 sutures through ATFL
- 2 through CFL
- 2 sutures either side of interval of ATFL and CFL
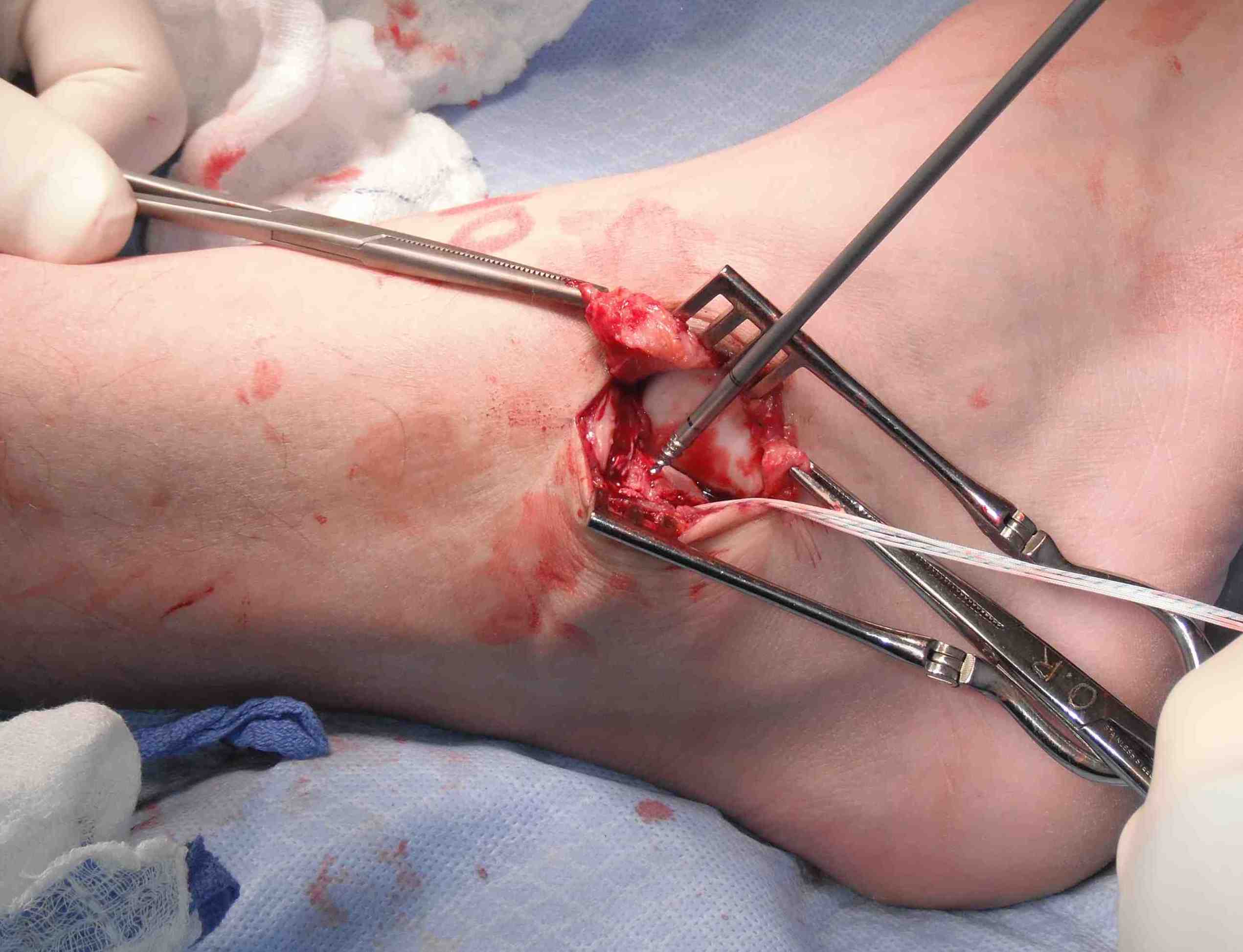
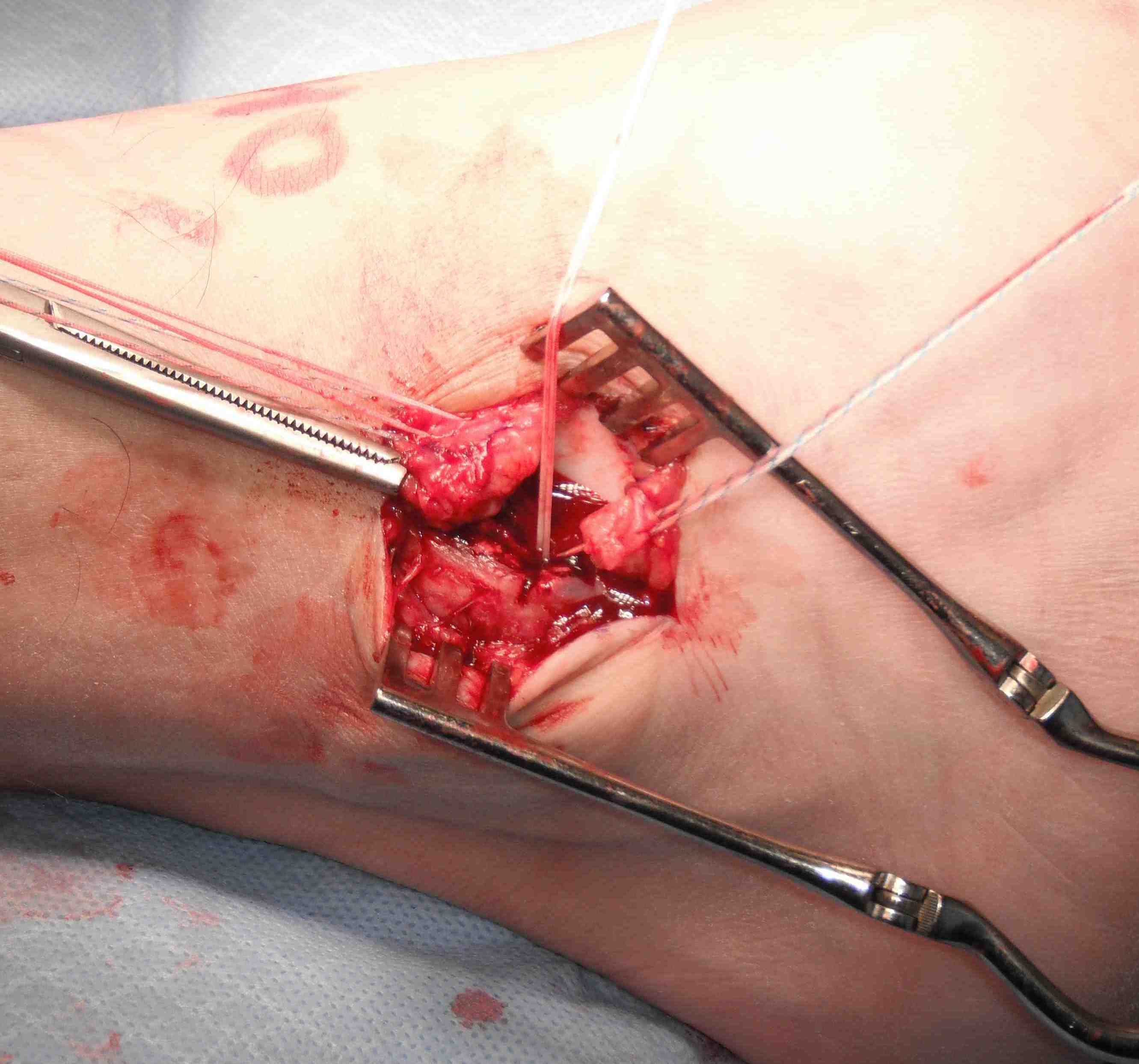
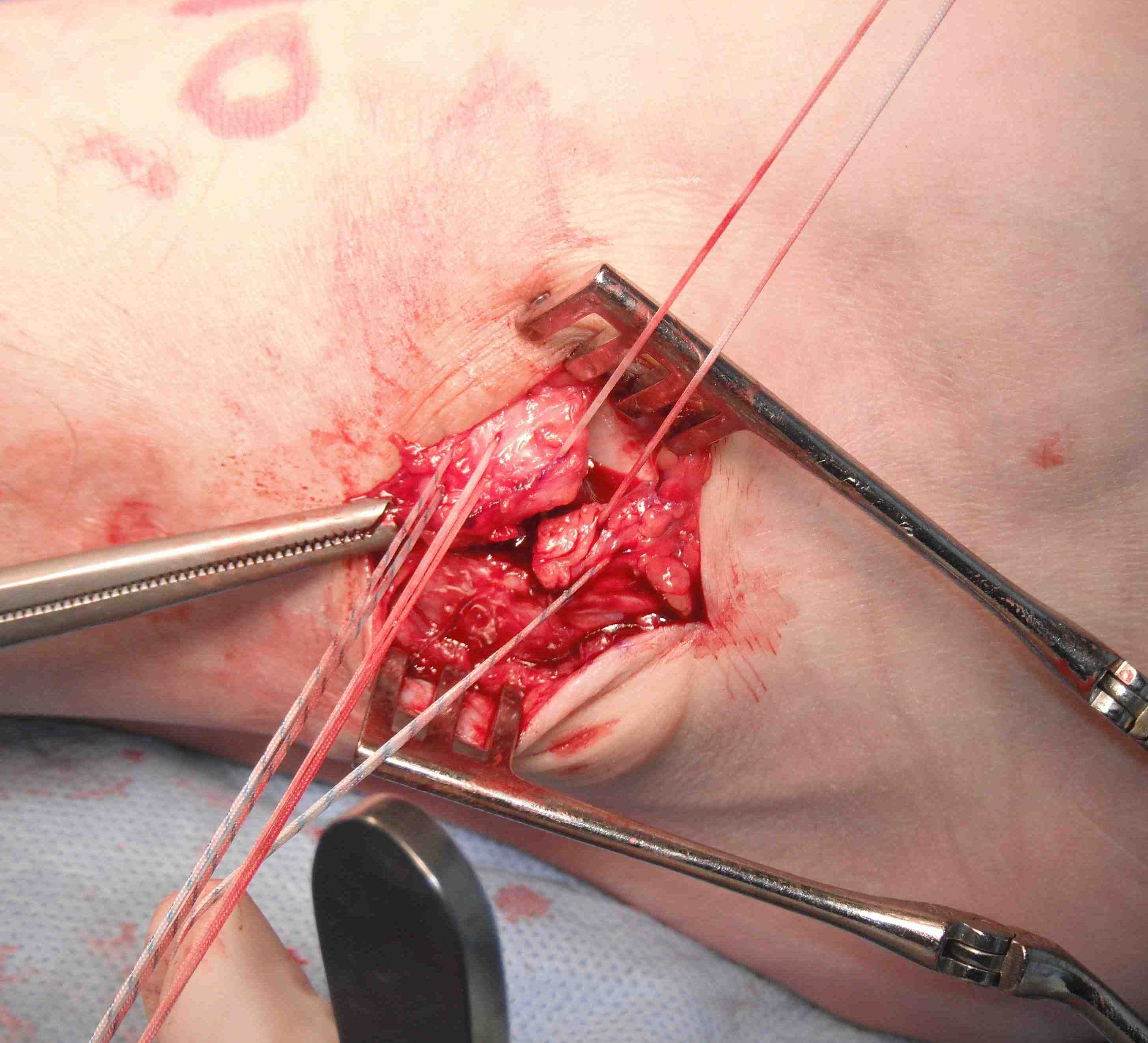
Gould modification
- inferior extensor retinaculum anatomy laterally arises from anterior surface calcaneum
- medially has 2 limbs - med malleolus & plantar aponeurosis
- advance the inferior retinaculum and suture to the fibular to reinforce the repair


Results
Ligamentous laxity
- 199 ankles with mean 5 year follow up
- modified Brostrom
- clinical failure non ligament lax: 11%
- clinical failure ligament lax: 45%
- ligamentous lax / talar tilt > 15 / anterior displacement > 10 mm / syndesmotic widening / OC lesion
Postoperative weight bearing
Vopat et al Orthop J Sports Med 2020
- systematic review of early versus delayed weightbearing after lateral ligament repair
- 28 studies and 1500 patients
- early weight bearing higher functional outcome scores
- early weight bearing increased objective laxity
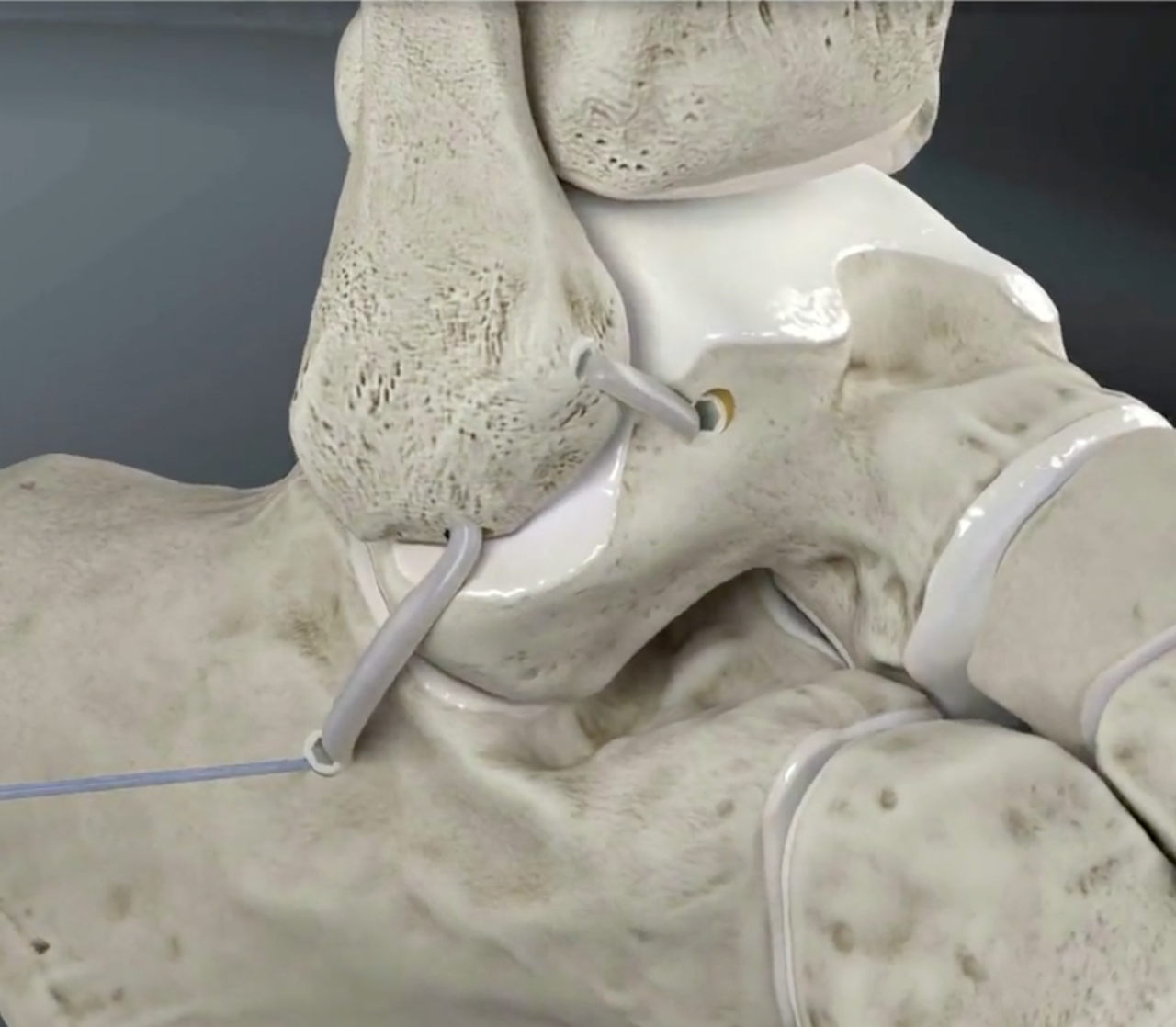
Suture tape augmentation / internal brace

Arthrex
Technique
Arthrex internal brace ankle ligament repair PDF
Arthroscopic techniques internal brace ankle ligament repair PDF
Results
Mercer et al Orthop J Sports Med 2022
- systematic review of suture tape augmentation compared to primary repair
- no difference in outcomes
- no evidence to recommend additional suture tape augmentation
Arthroscopic techniques
Technique
Vumedi arthroscopic ligament repair video
Arthroscopic ligament repair surgical technique PDF
Arthroscopic ligament repair + suture tape augmentation PDF
Results
Attia et al Orthop J Sports Med 2021
- systematic review of open versus arthroscopic repair
- 8 studies and 400 patients
- superior outcome scores with arthroscopic
- no difference in objective stability
Anatomic reconstruction
Options
Autograft
Allograft
Suture tape
LARS ligament
Technique
Arthrex anatomic reconstruction surgical technique video
Arthroscopic ATLF reconstruction technique PDF

Arthrex
Results
- systematic review of return to sports after anatomic ankle ligament reconstruction
- 25 studies with 1400 patients
- 95% return to any sport
- 83% return to previous sport
- 87% return to competitive sport
- mean time 12 weeks
- RCT of anatomic reconstruction with LARS v modified Brostrom
- 41 patients with 2 year follow up
- improved outcomes and reduced failure with LARS
Non anatomic reconstruction
Indications
Poor tissue for anatomic repair
Hypermobile STJ / ligamentous laxity
Revision
Issue
Limited movement of subtalar joint
Osteoarthritis
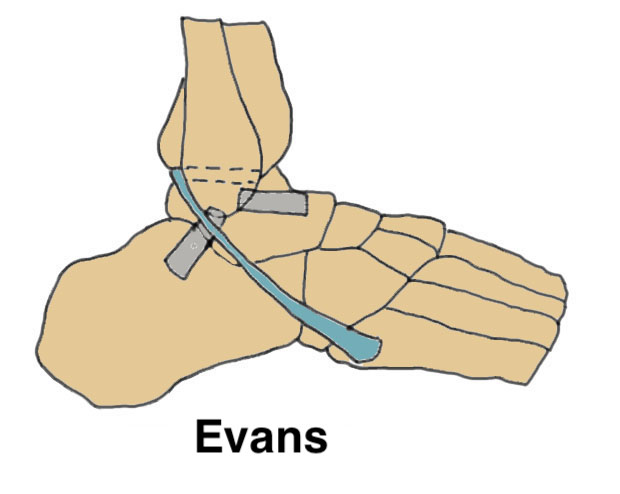
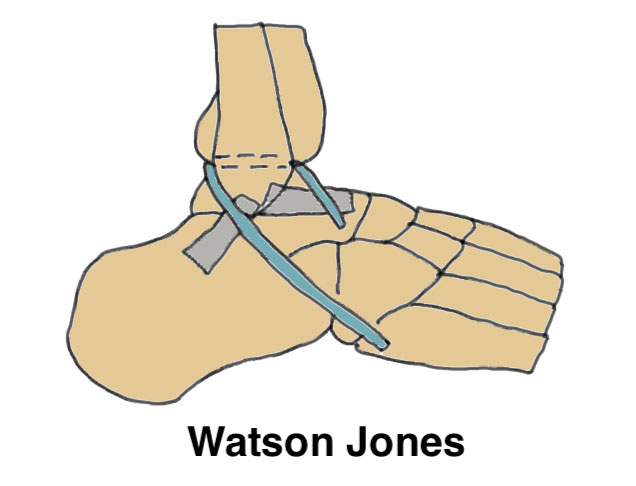
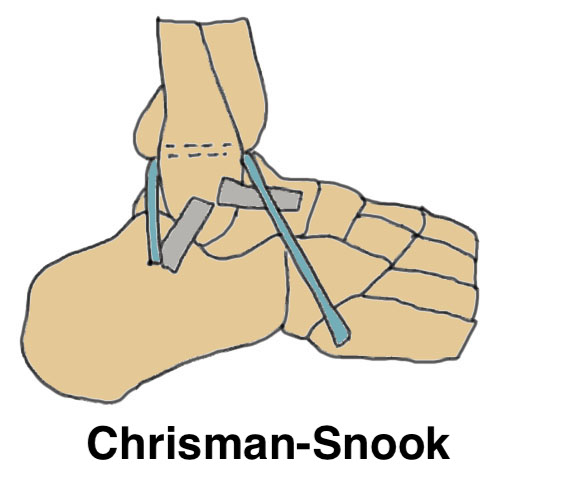
| Evans | Watson-Jones | Chrisman-Snook |
|---|---|---|
| Tenodesis of Peroneus brevis |
Split peroneus brevis |
Split peroneus brevis |
|
Transect peroneus brevis proximally at MT juction. Proximal stump tenodesed to peroneus longus. Distal stump transferred transosseously to fibula |
Split Peroneus brevis in two Leave attached to base 5th metatarsal Divide proximally Pass through fibula posterior to anterior Pass into drill hole in talar neck |
Split Peroneus brevis in two Leave attached to base 5th metatarsal Divide proximally Pass through fibula anterior to posterior Pass into drill hole in calcaneus |
 |
 |
 |
Results
- RCT of static versus dynamic reconstruction using peroneus brevis
- increased satisfaction with static reconstruction
- reduced recurrence with dynamic reconstruction
