


Conditions
Fracture
Stress fracture
Sesamoiditis
Nerve impingement
AVN
Osteoarthritis
Anatomy
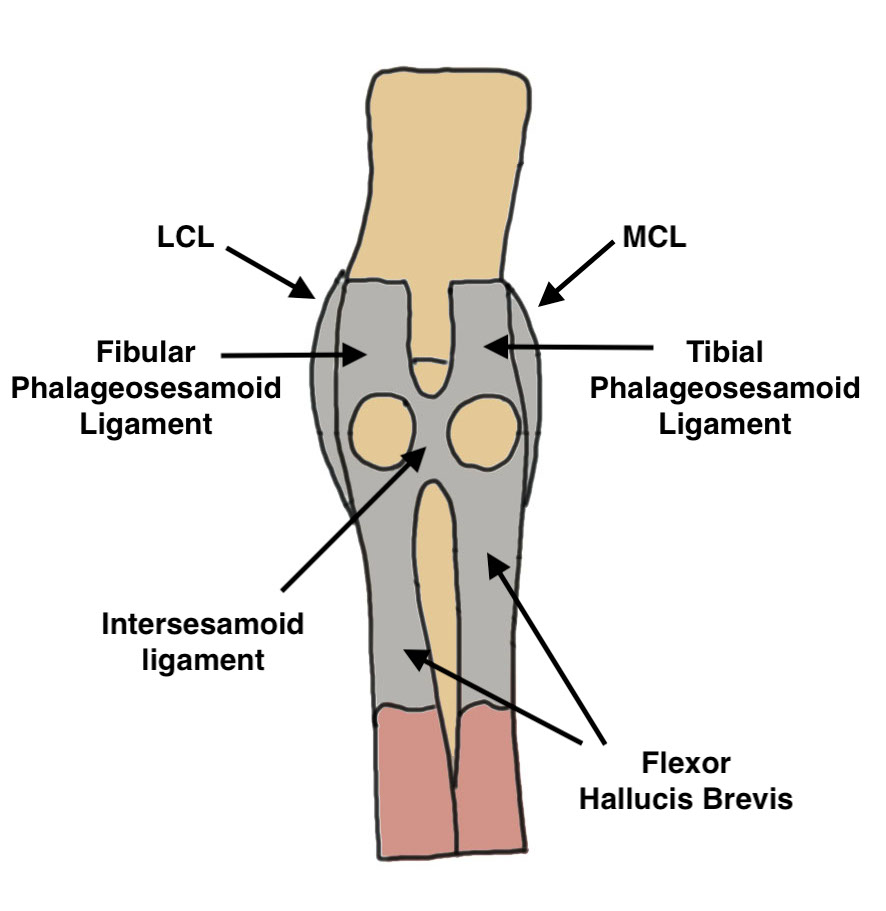
| Sesamoids | Insertions | Tibial sesamoid | Function | Position |
|---|---|---|---|---|
|
Embedded in plantar plate - phalangeo-sesamoid ligaments - intersesamoid ligament
Each side of inter-sesamoid ridge Articulate with plantar facets |
FHB tendons Adductor hallucis Abductor hallucis |
Larger than fibular Weight bearing Higher incidence fracture |
Absorb weight FHB fulcrum |
Proximal to MT head in stance Pulled under MT head with dorsiflexion / toe off |
Congenital absence rare
3 sesamoids - extra on plantar aspect of IPJ
Blood Supply
Type A: 50% medial plantar artery and plantar arch
Type B: 25% plantar arch
Type C: 25% medial plantar artery
Increased risk of AVN if only single vessel into sesamoid
Bipartite sesamoid
Ossification
Begins between age 7-10 years
- often multiple centers
- may result in bipartite / tripartite appearance
Incidence
Tibial bipartite 10%
Bilateral 25%
Fibular bipartite rare



Bipartite sesamoids
Sesamoid Fracture
Clinical
Acute injury
Acute pain
Tender over sesamoid
Differential diagnosis
Bipartite sesamoid
Fracture through bipartite sesamoid
Nonunion sesamoid fracture
Stress fracture - more chronic course and history
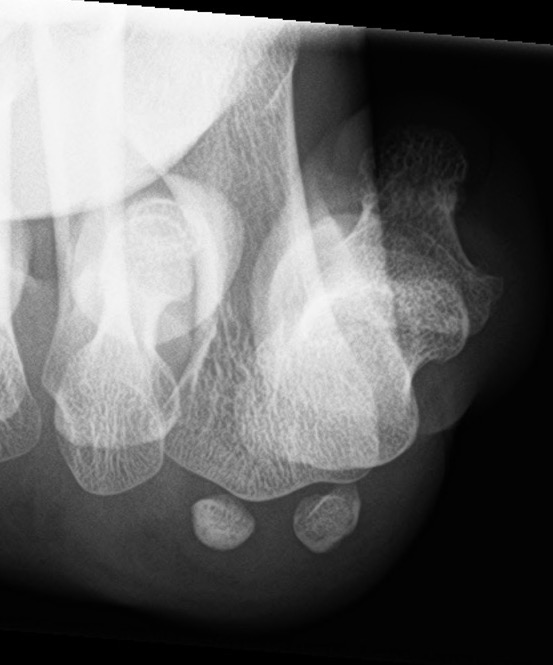
Imaging
Bilateral standing xray can help

Unclear if bipartite or stress fracture


Irregular borders suggest fracture rather than bipartite


Irregular borders suggest fracture rather than bipartite

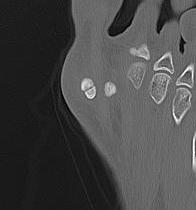
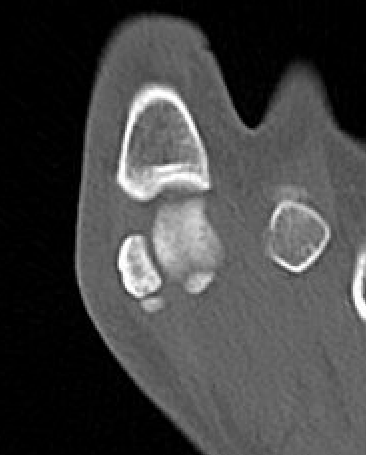
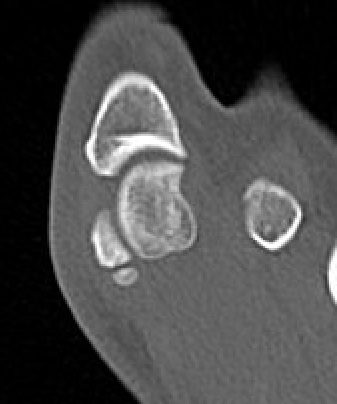
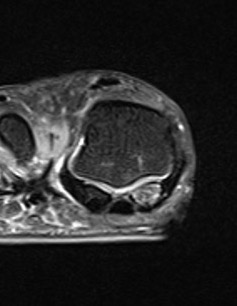
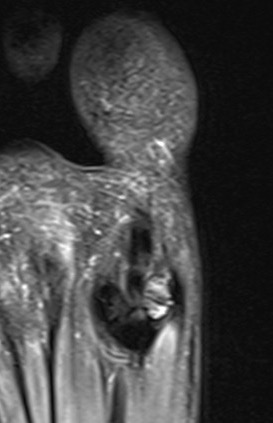
CT demonstrates irregular borders consistent with fracture of tibial sesamoid
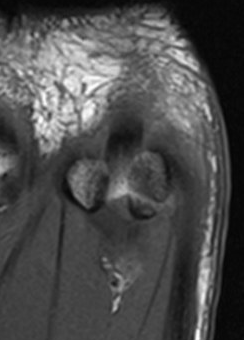
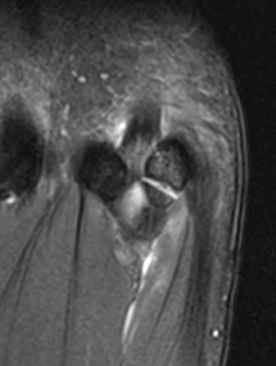

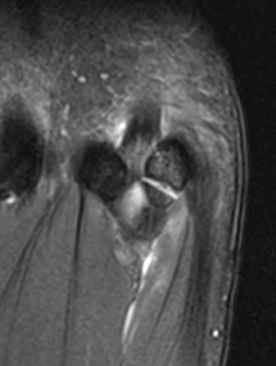
Edema on T2 MRI indicates likely acute fracture
Nonoperative management
Complications
- nonunion
- AVN
Operative management
Options
Open reduction and screw fixation
Bone graft nonunion
Excision of fragment
Arthroscopic bone grafting sesamoid nonunion PDF
Sesamoid stress fracture
No acute injury / history of chronic pain with overuse

Tibial sesamoid stress fracture in a marathon runner
Sesamoid Avascular necrosis
Etiology
Overuse
Stress fracture
Nonunion fracture
Xray
Enlarged / deformed / sclerotic with mottling / fragmentation
Management
Orthotics / activity modification / NSAIDS
Isolated sesamoid resection
Sesamoiditis
Clinical
Painful inflammatory condition of sesamoids secondary to repetitive trauma
Most common teens / young adults
Inflammation & bursal thickening may be present
Normal xray
Management
Orthotics / activity modification / NSAIDS
Isolated sesamoid resection
Sesamoid osteoarthritis
Management
Management
Orthotics / activity modification / NSAIDS
Isolated sesamoid resection
Nerve Impingement
Clinical
Medial branch plantar digital nerve on medial sesamoid
Lateral branch plantar digital nerve on lateral sesamoid
Management
Orthotics / activity modification / NSAIDS
Isolated sesamoid resection +/- neurolysis
Isolated sesamoidectomy


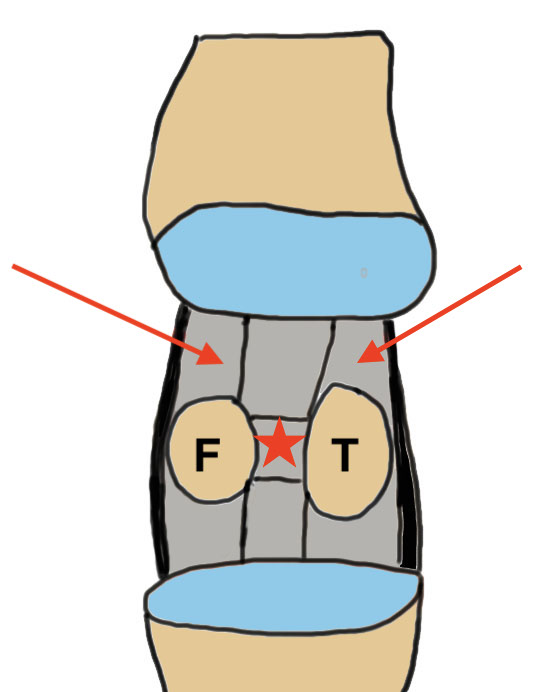
Principles
1. Avoid excising both - risk Cock Up deformity
2. Avoid incision directly over sesamoid - painful scar
3. Repair adductor hallucis if excising lateral sesamoid
Results
Shimozono et al J Foot Ankle Surg 2018
- systematic review of sesamoidectomy
- 10 studies, 196 procedures
- 94% RTS, with 90% at previous level
- 23% complication rate
- 3% revision rate
Saxena et al Foot Ankle Int 2003
- 26 sesamoidectomies
- 1 hallux valgus from tibial sesamoidectomy
- 1 hallux varus from fibular sesamoidectomy
- 2 neuromas
- one loss of flexion
Saxena et al J Foot Ankle Surg 2022
- 70 sesamoidectomies in athletes
- 5.7% complication rate
- 2 cases mild flexion weakness
- 1 wound issue, 2 DVT
- no hallux valgus / varus
Options
Open
Arthroscopic
Tibial sesamoidectomy
Open
3cm plantar medial incision
- medial branch plantar digital nerve identified & retracted
- open capsule
- release inter-sesamoid ligament
- shell out sesamoid from capsule & plantar plate with knife
Arthroscopic
Arthroscopic sesamoidectomy PDF
Fibular
Dorso-lateral approach
- first webspace web space
- identify & protect branch SPN
- interval between adductor hallucis & joint capsule opened
- release adductor hallucis from lateral sesamoid
- release inter-sesamoid ligament
- shell out sesamoid from capsule & plantar plate with knife
- repair adductor hallucis tendon to lateral capsule
Plantar incision
- 4cm incision between 1st and 2nd metatarsals
- identify and retract NV bundle lateral
- release adductor hallucis from lateral sesamoid
- release inter-sesamoid ligament
- shell out sesamoid from capsule & plantar plate with knife
- repair adductor hallucis tendon to lateral capsule
