


Definition
Painful restriction of dorsiflexion of the great toe secondary to dorsal osteophytes
Osteoarthritis of the great toe MTPJ
Epidemiology
Middle Age
Male more common
Etiology
Idiopathic most common
Long first ray
Trauma - cartilage injuries, hyperextension injuries
Inflammatory - gout, rheumatoic, seronegative arthropathies
Clinical
Pain with walking
Numbness - impingement on medial branch superficial peroneal nerve
Enlarged MTPJ
Dorsiflexion restricted and painful
- normal 75 degrees dorsiflexion
- normal 35 degrees plantarflexion
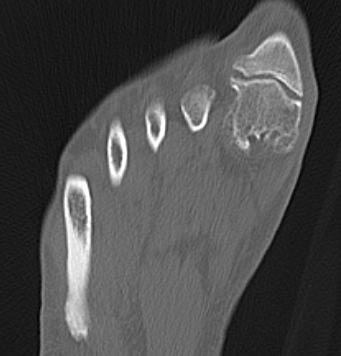
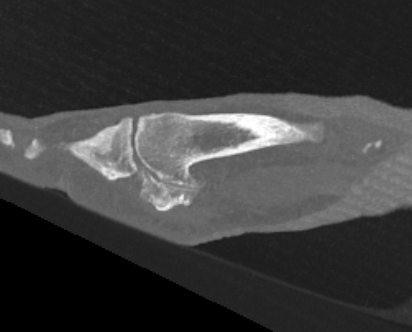
X-ray
Osteoarthritis
- joint space narrowing
- dorsomedial osteophyte



Mild to moderate OA


Severe OA
Management
Non Operative
Options
Orthotics
- stiff soled shoes to limit toe bending
- rockerbottom sole
- wide toe box
Cortisone
Grice et al Foot Ankle Int 2017
- 22 patients treated with cortisone
- pain relief for 3 months
Hyaluronic acid
Pons et al Foot Ankle Int 2007
- RCT 40 feet with painful hallux rigidus
- HA versus cortisone
- improved pain and function in HA group at 3 months
Munteanu et al Ann Rheum Dis 2011
- RCT of HA versus saline in 151 toes
- no difference in pain at 3 months
Operative
Options
Cheilectomy
Arthrodesis
Joint replacement
- systematic review of arthrodesis versus joint replacement
- 33 studies and 1200 patients
- improved functional outcome with arthrodesis
- arthrodesis: complication 23%, revision 4%
- joint replacement: complications 26%, revision 11%
Other
Resection arthroplasty / Keller's procedure
- indicated in elderly, associate with cock up toe deformity
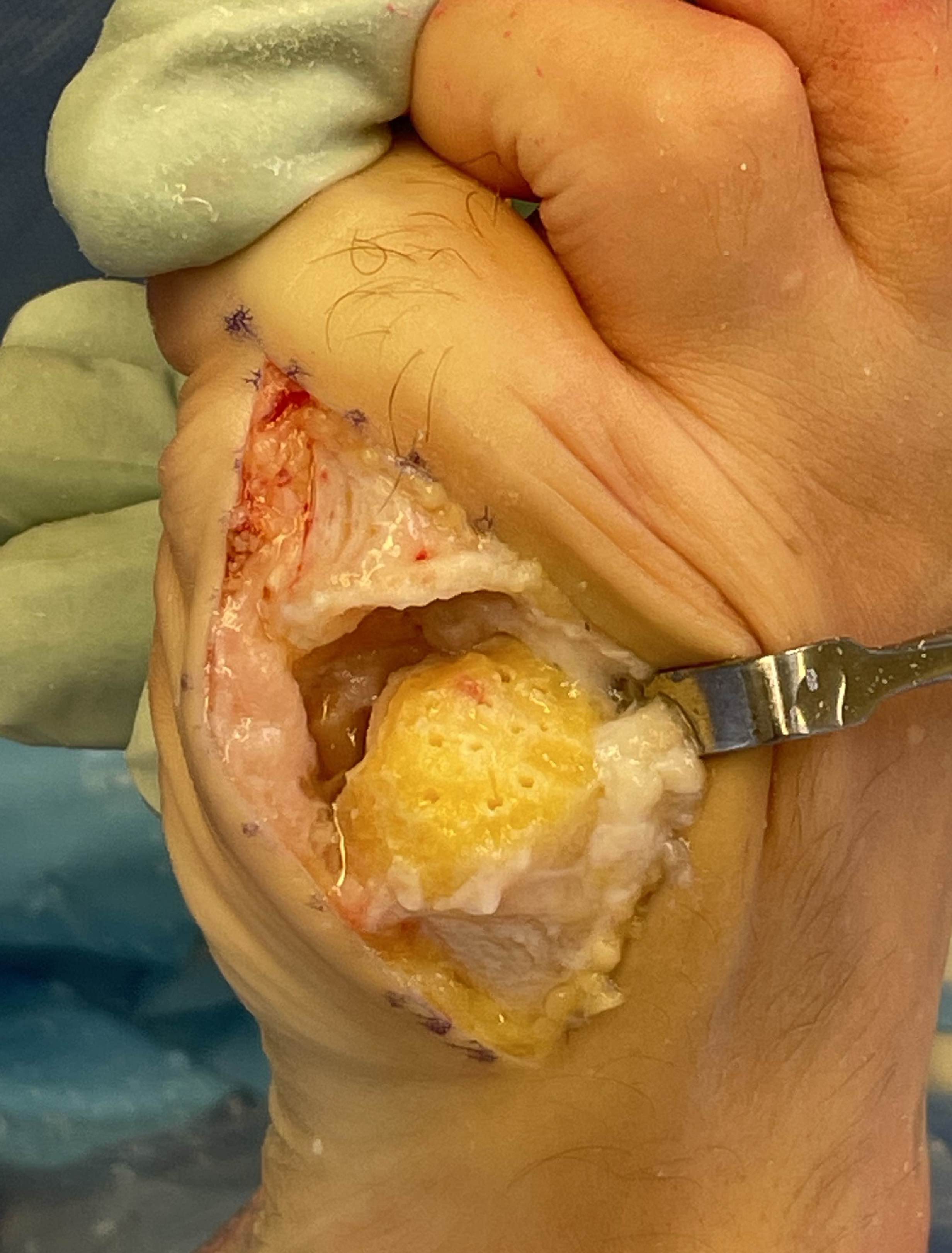
Interposition arthroplasty
- insertion of biological spacer
- Butler et al Foot Ankle Spec 2022
- Vumedi surgical technique video
Metatarsal osteotomy
- dorsal closing wedge Moberg osteotomy
- Roukis et al J Foot Ankle Surg 2010
Cheilectomy
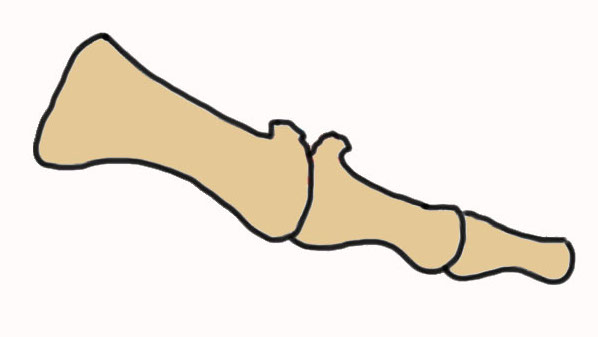
Concept
- removal of dorsal osteophytes
- increase painless dorsiflexion range
Indication
- for adults with minimal degenerative changes
- normal joint space in plantar half MTPJ
Options
- open
- MIS
Technique
Approach
- dorsal approach
- medial approach
AO surgery reference dorsal approach
AO surgery reference medial approach
Remove ~ 1/3 of dorsal metatarsal head
- remove osteophytes from base of P1


Results
- systematic review of cheilectomy
- ROM improved 51 degrees (better with open surgery v MIS)
- VAS improved by 73% (better with open surgery)
- residual pain 7% (more common open surgery)
- nerve injury 4% (more common MIS)
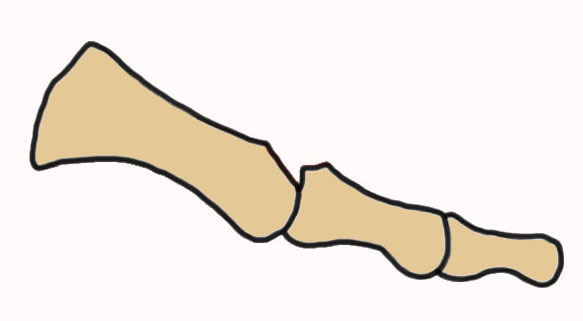
Arthrodesis
Indication
- advanced OA
- young, active patient


Screw fixation


Plate fixation



Screw + plate fixation
Technique
Vumedi surgical technique 1st MTPJ fusion medial approach video
Vumedi surgical technique 1st MTPJ fusion dorsal approach video
Vumedi surgical technique MIS 1st MTPJ fusion video
Approach
- dorsal approach
- medial approach
Position
- 10 - 15° valgus
- 10- 15° dorsiflexion relative to plantar surface / 20 - 25° relative to metatarsal shaft
Fixation
- screws / plate / screws + plate


Results
- 4 year follow up of 60 1st MTPJ fusion
- screw + plate
- 93% fusion
- remainder painless pseudoarthrosis
- 72% very satisfied, 18% satisfied
- 99 1st MTP arthrodesis
- plate verus plate + lag screw
- improved sagittal plane stability with addition of screw
Complications
Gaudin et al Orthop Traumatol Surg Res 2018
- 158 cases of revision 1st MTPJ arthrodesis
- 54% for painful hardware
- 14% nonunion
- 8% malunion
- 11% claw toe / metatarsalgia
- 8% IPJ disorders
Joint replacement
Options
Hemiarthroplasty
Stryker Cartiva synthetic cartilage implant - recalled due to safety concerns
Total joint arthroplasty
- silastic implants
- press fit metal / polyethylene

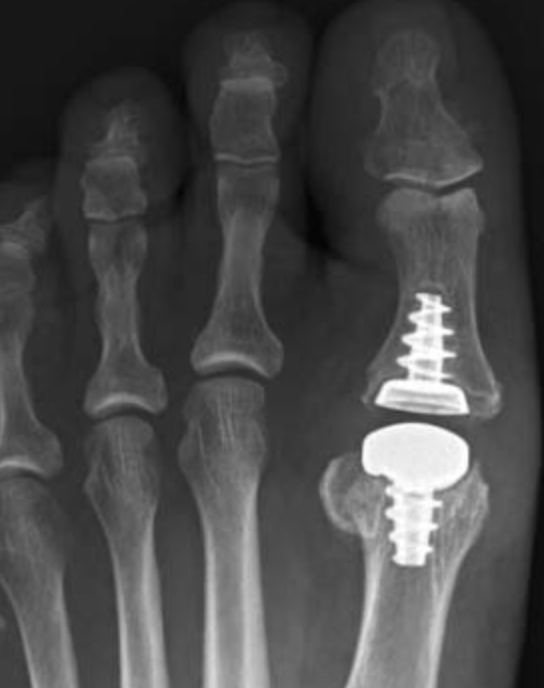

Anika Toe Motion Implant System
Technique
Vumedi total toe arthroplasty video
Total toe replacement
- 47 patients reviewed at mean of 10 years
- screw in metal Toe-Fit Plus implant
- 51% reported satisfactory results
- 23% ongoing pain
- 21% removal of implants
Clough et al Bone J Journal 2020
- 108 cases silastic joint replacement
- mean follow up 5 years
- 97% survival
- 90% satisfaction
Hemiarthroplasty
Stibolt et al Foot Ankle Spec 2019
- systematic review of hemiathroplasty versus total toe arthroplasty
- improved function and ROM with hemiarthroplasty
Cartiva synthetic cartilage implant
Baumhauer et al Foot Ankle Int 2016
- RCT of synthetic cartilage implant versus arthrodesis
- 152 implant patients with 2 year follow up
- 9% revision rate to arthrodesis at 2 years
- similar outcomes to arthrodesis, but with maintenance ROM
Butler et al Eur J Orthop Surg Traumatol 2024
- systematic review of synthetic cartilage implant v cheilectomy v arthrodesis
- complication rate: Cartiva 28%, cheilectomy 12%, arthrodesis 24%
Stryker Cartiva Implant Recall
