Definition
Inflammation of achilles tendon at the insertion
Haglund syndrome triad
- insertional achilles tendonitis
- Haglund's deformity
- retrocalcaneal bursitis
Pathogenesis
1. Peritendonitis - inflammation of paratenon
2. Tendinopathy - combination of inflammation + tendinous degeneration
3. Combination
Anatomy
Triceps tendon
- medial and lateral gastrocnemius + soleus
- surrounded by paratenon which allows gliding and supplies nutrition
Insertion
- middle 1/3 calcaneal tuberosity
- 2 cm distal to the posterosuperior prominence
- 2 x 2 cm area
- 90o rotation distally
Retrocalcaneal bursa (x2)
- proper is between tendon and calcaneum
- superficial is between tendon and skin
Pathology
Tendon degeneration with loss of parallel structure and thickening
Etiology
Two groups
- overweight / middle aged / comorbidities (diabetes) / seronegative arthropathies
- also occurs in athletes 30s - 40s
Symptoms
Stiffness with prolonged rest
Pain at bone-tendon interface with activity
Painful to wear shoes
Examination
Localised tenderness & thickening at insertion
Bony lump / Haglund's deformity
Dorsiflexion may be limited
Haglund's deformity
X-ray
Insertional achilles tendon spurs
- also present in asymptomatic patients


Calcification of bone-tendon interface with spur
Haglund's Deformity
- bony protuberance of posterosuperior calcaneus


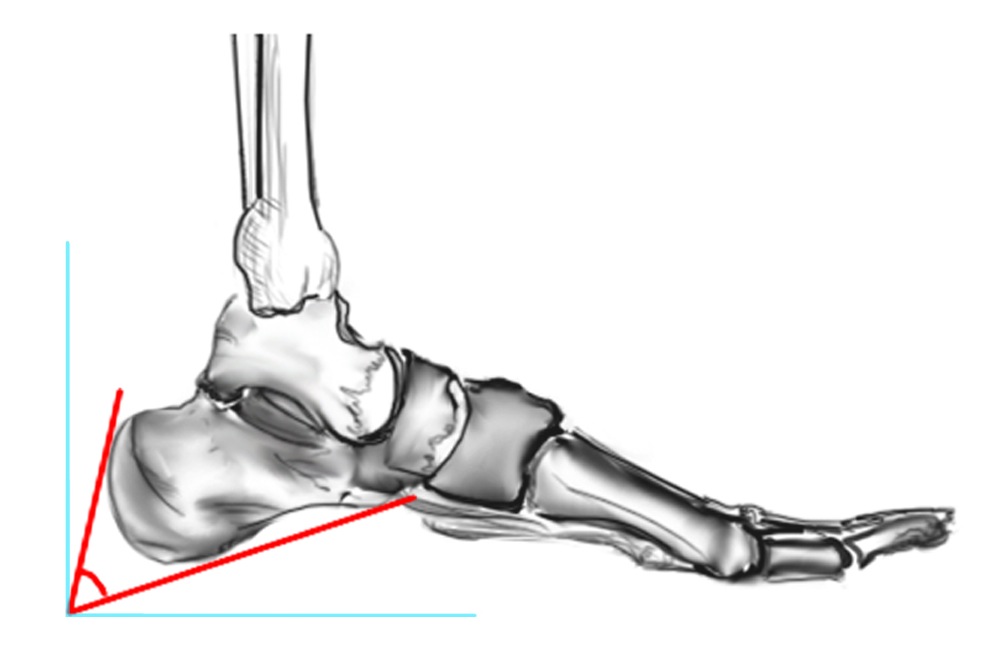
Pavlov's parallel pitch lines
- lateral weight bearing x-ray
- draw parallel pitch lines
- defines Haglund's deformity to be removed (above second line)

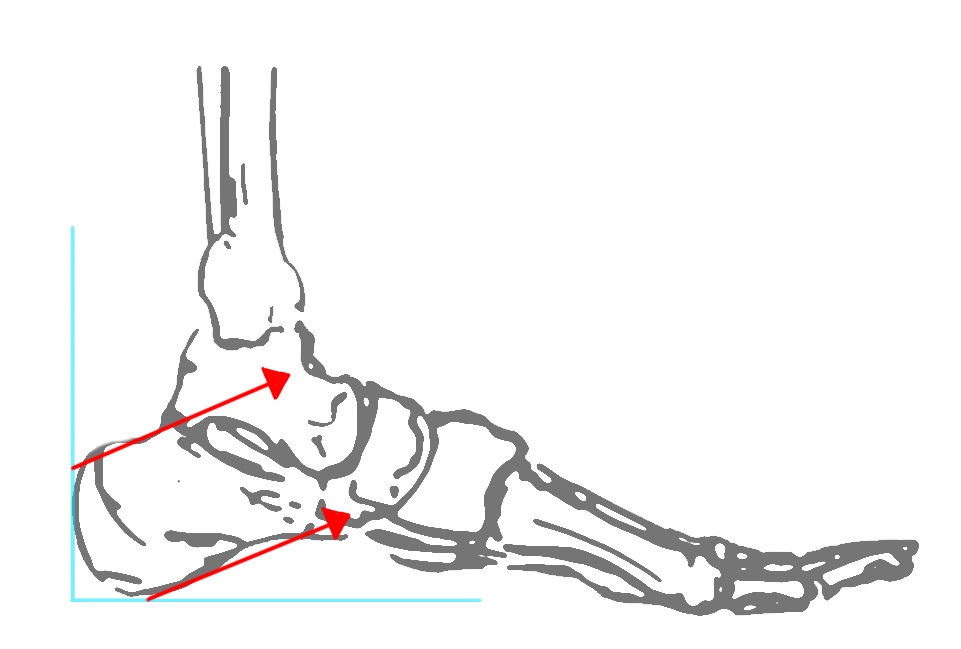
Fowler's angle - Normal < 70° / Abnormal > 80°
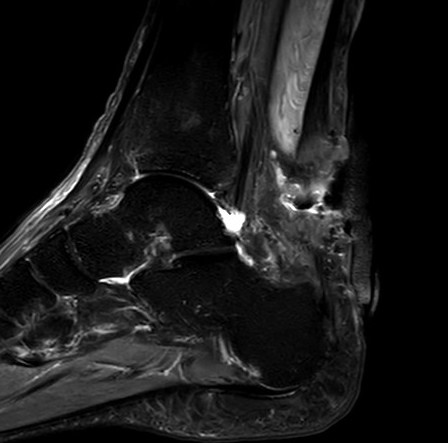
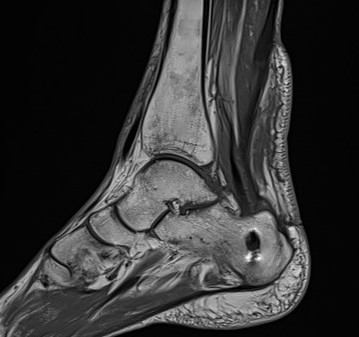
MRI


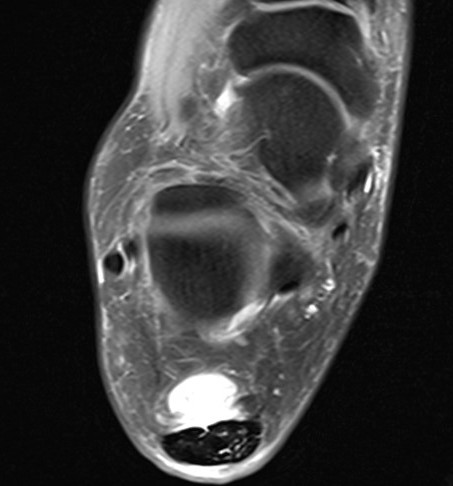
Retrocalcaneal bursitis with Haglund's
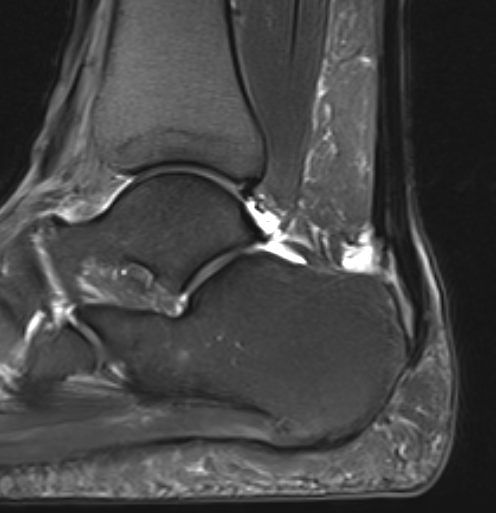
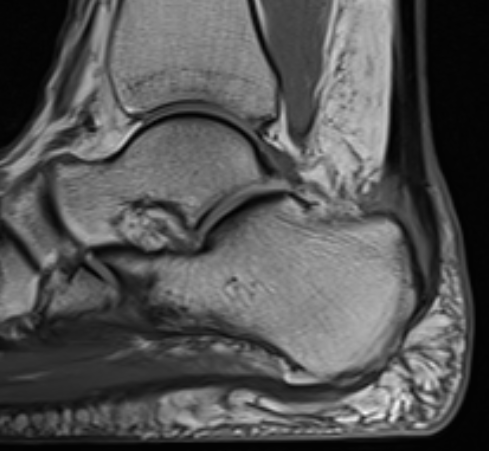
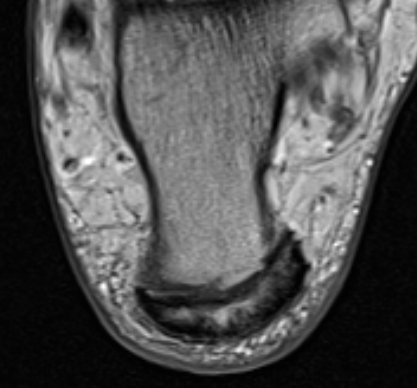
Partial tearing at insertion with retrocalcaneal bursa
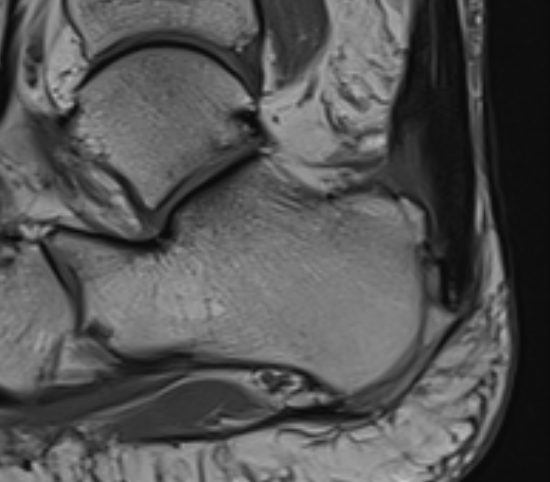
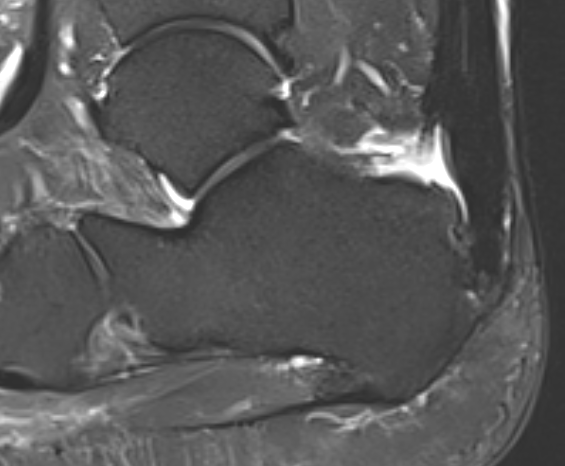
Tendon thickening, Haglund's deformity and retrocalcaneal bursa
MRI grading
- Grade I: 6 - 8 mm thickening
- Grade II: > 8 mm tendon thickness with < 50% tendon degeneration
- Grade III: > 8 mm tendon thickness with > 50% tendon degeneration
Nonoperative Management
Eccentric exercises
Ko et al BMC Musculoskeletal disorders 2023
- meta-analysis of 9 studies and 400 patients with insertional tendinopathy
- evidence for short term pain relief for eccentric exercises
Night splints
de Vos et al Br J Sports Med 2007
- RCT of eccentric exercises +/- night splints for non insertional tendinopathy
- no advantage with addition of night splint
Extra-corporeal shockwave therapy
Paantjens et al Sports Med Open 2022
- evidence for shock wave therapy in noninsertional tendinopathy
- limited evidence for shock wave therapy in insertional tendinopathy
Injections
Cortisone
Risk of tendon rupture
PRP
- systematic review of PRP for achilles tendinopathy
- evidence of short term improvement in pain
Operative management
Options
Open debridement and decompression
Arthroscopic debridement
Zadek's osteotomy
- systematic review of open versus endoscopic debridement for Haglund's deformity
- both effective
- shorter operative times / reduced complications / better cosmesis with arthroscopic
- complication open surgery: 12%
- complication endoscopic surgery: 5%
Open debridement and decompression
Technique
Arthrex - Achilles SpeedBridge™ System
Vudmedi surgical technique video
Patient prone
- elevate ankle to allow dorsiflexion
- identify and preserve sural nerve
- central tendon split
- resect retrocalcaneal bursa
- resect posterosuperior calcaneum / Haglunds deformity
- +/- release achilles tendon insertion
- > 50% release needs repair
- +/- augment with tendon reconstruction

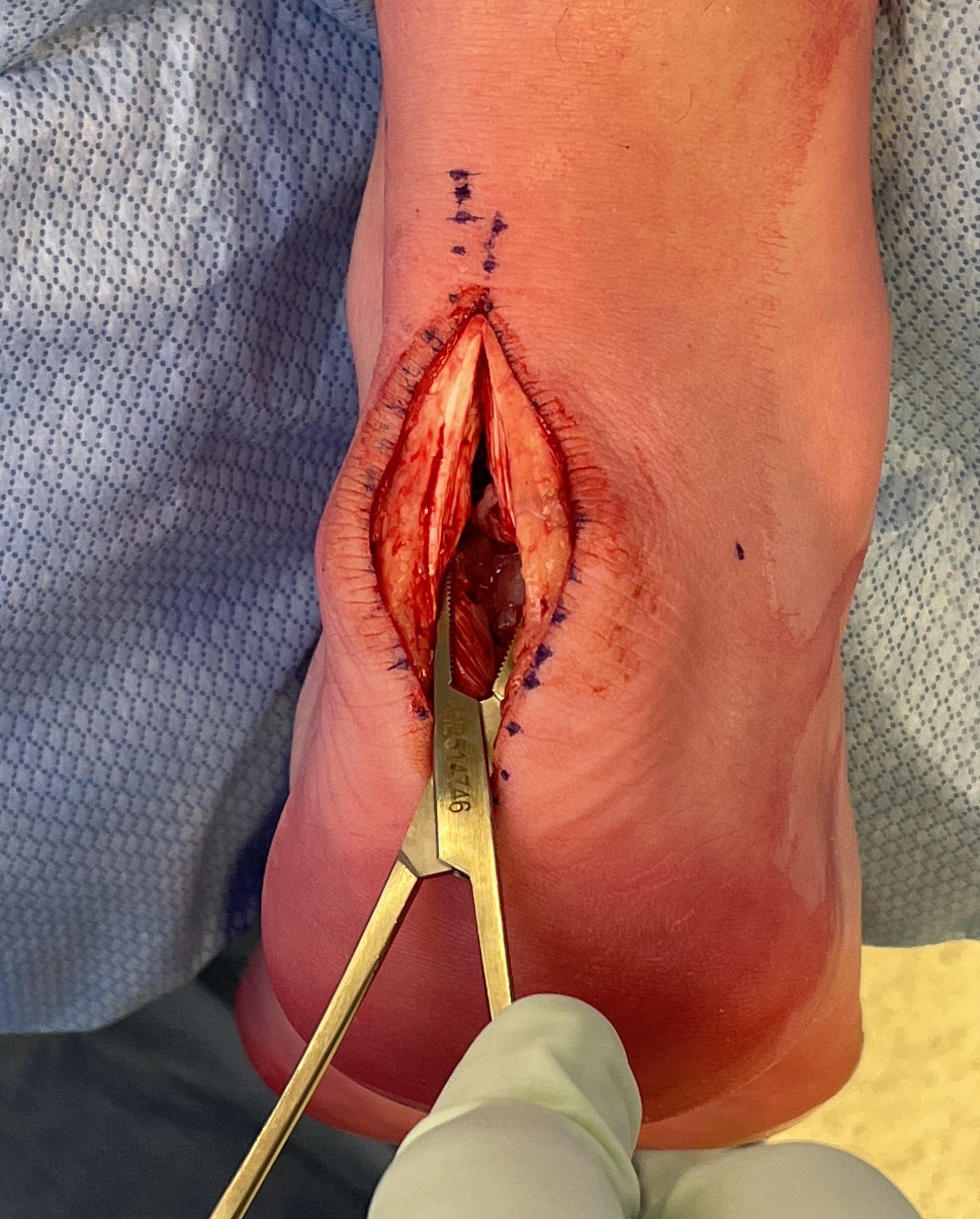
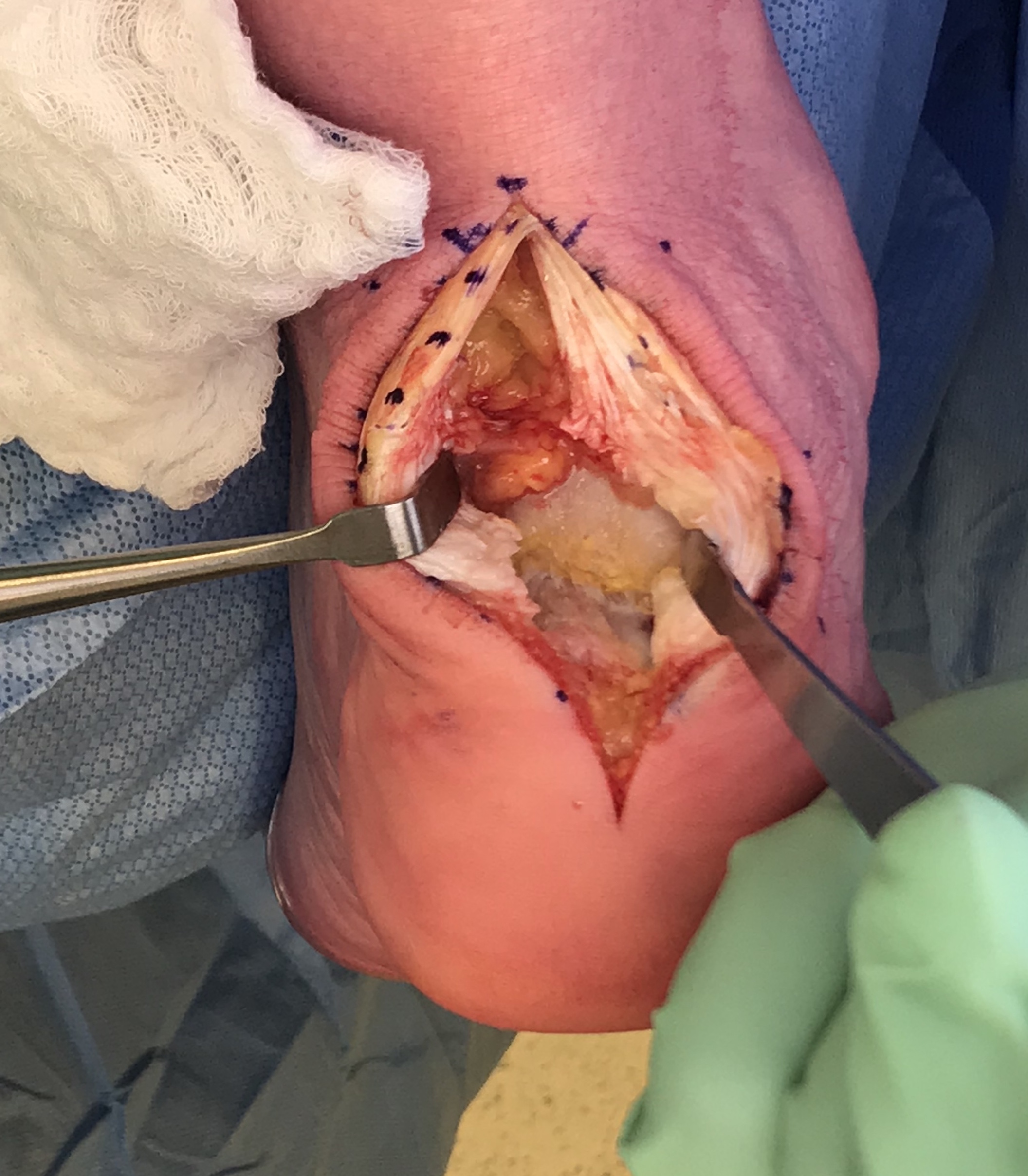
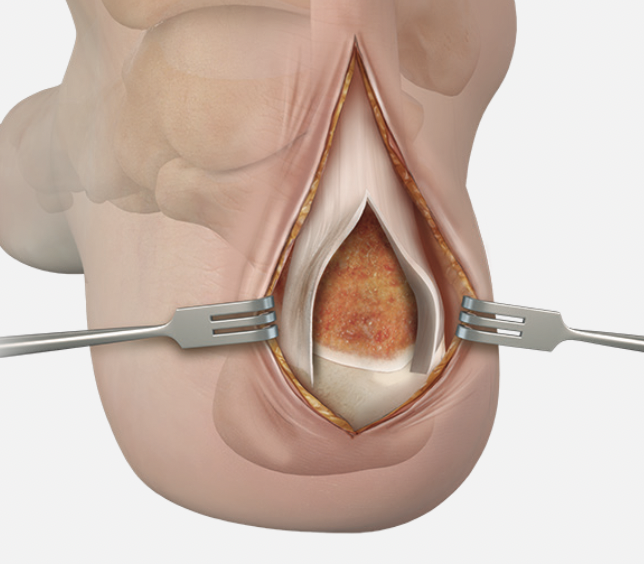
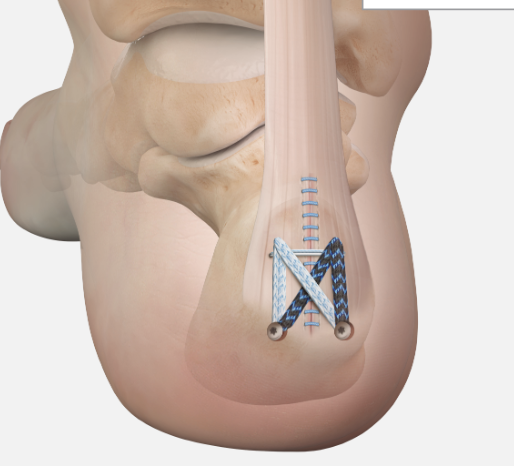
Arthrex speedbridge system
Results
- open calcaneoplasty and bursectomy in 41 feet
- 90% complete or significant relief of symptoms, 10% felt improved, none worse
Hunt et al Foot Ankle Int 2015
- RCT of decompression +/- FHL transfer in 39 patients
- no evidence of improved outcomes with addition FHL transfer
Sabaghzedah et al Foot Ankle Orthop 2024
- RCT decompression +/- FHL transfer in 40 patients > 50y
- FHL transfer may improve, but not clinically significant
- FHL transfer takes longer, with more incisions
Complications
Nerve injury / numbness / posterior heel pain
Wound infection / wound breakdown



Tendoachilles rupture

Rupture of the achilles tendon insertion after open debridement and repair


Salvage with turndown and FHL transfer
Endoscopic Calcaneoplasty
Indications
Haglund's deformity + retrocalcaneal bursitis
Technique

Vumedi surgical technique video
Results
- endoscopic calcaneoplasty in 81 patients
- 75/81 (93%) good or excellent results
Zadek osteotomy
Dorsal closing wedge osteotomy
Technique

Results
Black et al Foot Ankle Spec 2023
- systematic review of 8 case series of Zadek osteotomy
- mean AOFAS improved from 56 to 93
- symptomatic hardware 3%
- DVT 1%
- nonunion 1%
Bakaes et al Foot Ankle Orthop 2024
- systematic review of open versus percutaneous Zadek's osteotomy
- both effective for insertional tendionopathy with Haglunds
- complication rate open: 10%
- complication rate percutaneous: 6%
