Definition
Full thickness tear (FTT)
- variable amount retraction from insertion
Partial thickness tear (PTT)
- incomplete
- bursal or articular sided
Epidemiology
Older patients
- average age 60
- uncommon < 40
- cadavers 30%
Milgrom & Schaffer JBJS Am 1995
- rotator cuff changes In asymptomatic adults
- 50% at 50 years
- 80% at 80 years
Anatomy
Blood Supply
Proximal from muscle belly
- suprascapular artery
- subscapular artery
Distal from bone
- branch of anterior circumflex humeral
Vessels more abundant on bursal side than articular side
NHx
1. Healing
- full thickness tears don't heal because of presence of synovial fluid
2. Progression
- tears do not necessarily extend
3. OA
- 5% FTT go on to cuff arthropathy if untreated
Pathogenesis
Chronic Tears
- 95%
- abnormal tendon
Acute tears
- trauma
- 5%
- normal tendon
Pathology
No evidence inflammation at tear site
- tendinosis / angiofibrotic dysplasia
Involvement
- most common involves supraspinatus
- infraspinatus / T minor maybe torn
- subscapularis seldom torn
Classification
1. Size
Cofield
- Small < 1 cm
- Moderate 1-3 cm
- Large 3-5 cm
- Massive > 5 cm
2. Extent
Partial Thickness
Quite common
- patients present with pain, not weakness
- difficult to differentiate from impingement
- MRI with gadolinium
A. Intra-tendinous
- in tendon
- no communication with bursa / joint
B. Articular side
- most common
- blood supply poor
- healing decreased by synovial fluid
- seen post traumatic in young
- probably due to intrinsic causes in elderly
C. Bursal side
- on subacromial surface
- less common
- likely to be secondary to impingement
Full Thickness
One tendon
- supraspinatus only
Multiple Tendons
- more likely OA if multiple tendons involved
3. Topography
Sagittal Plane
Superior - SS alone
Anterosuperior - SS & SSC
Posterosuperior - SS & IS
Total cuff - All 3 tendons
Coronal Plane
A. Minimal retraction
- close to insertion
B. Moderate retraction
- humeral head

C. Significant retraction
- at glenoid
History
Pain
Weakness
- 2° to tear
- can be limited by pain
- can use LA to differentiate
History of injury, especially dislocation
- minimal pre-injury symptoms
- suggests acute tear of normal tendon
Chronic Tear 95%
- long history impingement
- no history of injury
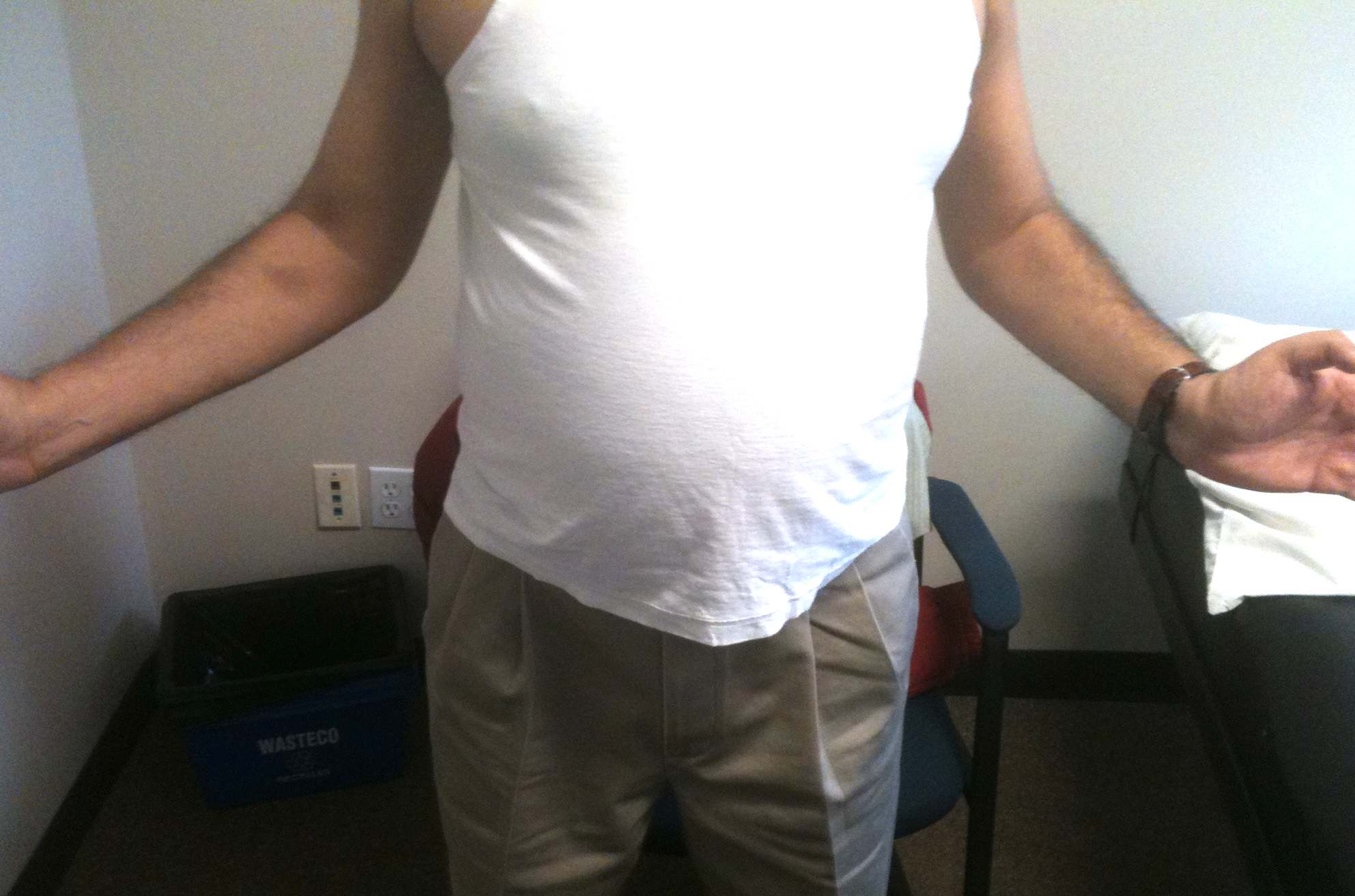
Examination


Wasting
- supraspinatus & infraspinatus
- rapid wasting with acute tears
- gradual wasting with chronic tears
Weakness related to
- size of lesion
- amount of pain
- grade 3 (MRC) or less indicates large tear
Supraspinatus
1. Patient's arm held elevated at 90°
- arm in 30° forward flexion with thumb down
- test resistance to inferior pressure
- palpate
2. Drop arm sign
- passively abduct arm
- get them to put it back to their side slowly
- apply small amount of pressure
- will drop arm at 30o
3. Shoulder hiking
- usually means massive cuff tear

Infraspinatus
1. Resisted ER
2. Lag
- put in arm in maximum ER
- ask patient to hold that position and release arm
- unable to maintain ER / arm lags
3. Hornblowers
- abduct and ER arm
- arm drops as unable to maintain ER
- Teres minor
Involvement of IS can often indicate a large or massive tear
Subscapularis
1. Gerber lift-off test
- IR hand to back pocket
- patient should be able to maintain hand away from bottom if SSC intact
- need sufficient IR for this test
- otherwise need belly press test
2. Belly press test
- fists on belly
- elbows forward / to eliminate deltoid
- resist force lifting fists away from belly
3. Increased ER compared with other arm
HCLA
Improves pain and allows physio
Diagnostic
- ensures pain from shoulder pathology
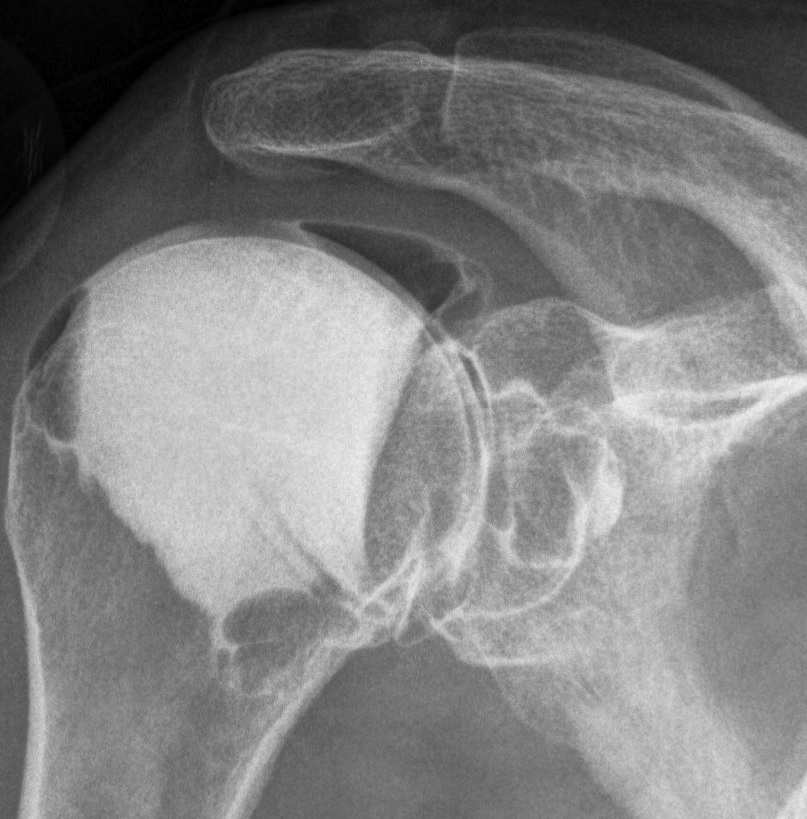
Xray
Views as for impingement
- assess acromion / GHJ OA / high riding head
Ultrasound
Advantages
- non invasive
- cost effective
- dynamic image
- can be used in orthopedic office
- useful and simple for assessment of cuff integrity post surgery
Disadvantage
- user dependant
- accuracy increases with skill and experience
- may miss small tears / partial thickness tears
- still images not easily interpreted by surgeon (c.f. MRI)
Evidence
O de Jesus Am J Roentengology meta-analysis MRI v MRA v US
- MRA most accurate
- MRI and US comparable
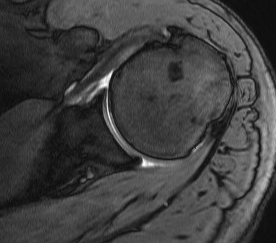
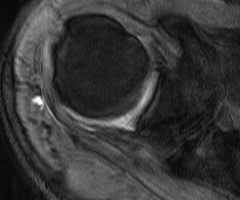
Normal
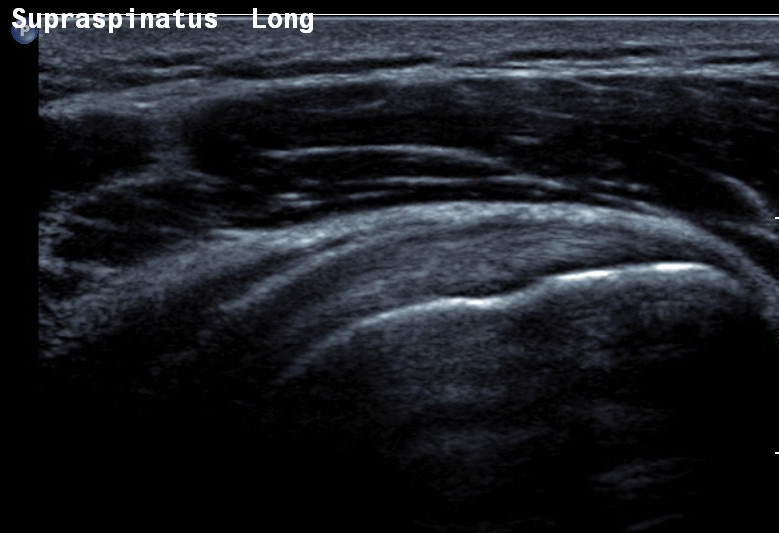
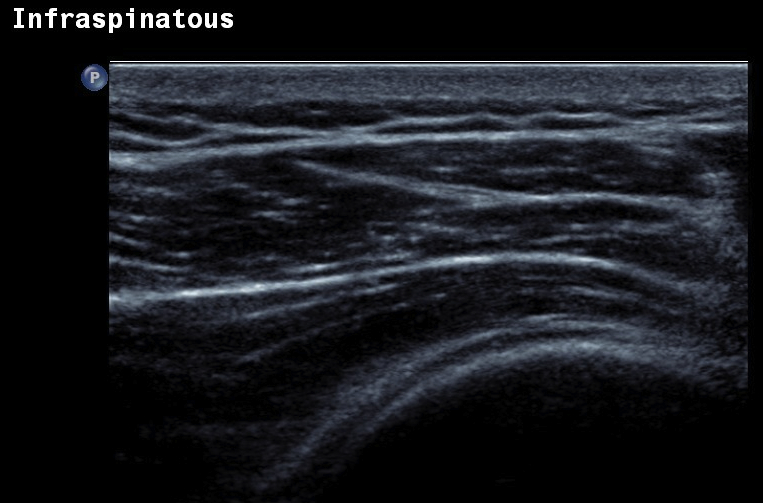
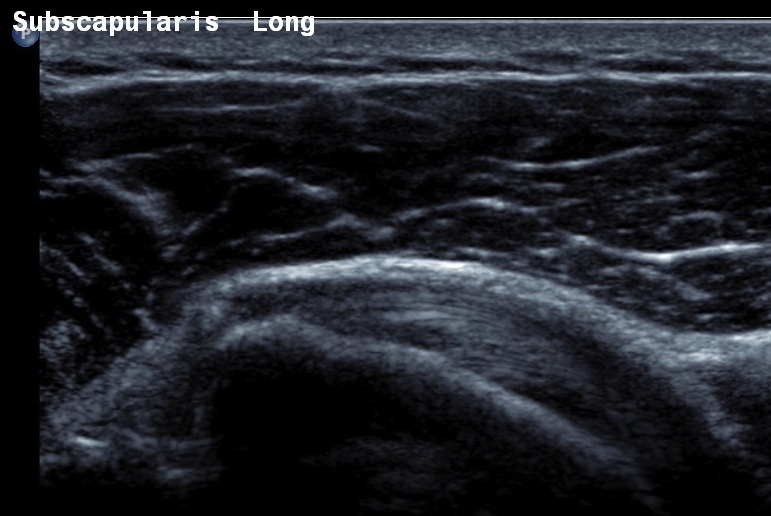
Tears

Arthrogram
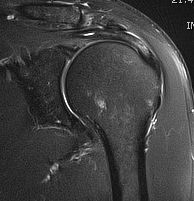
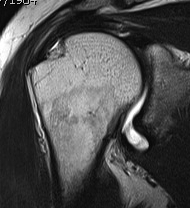
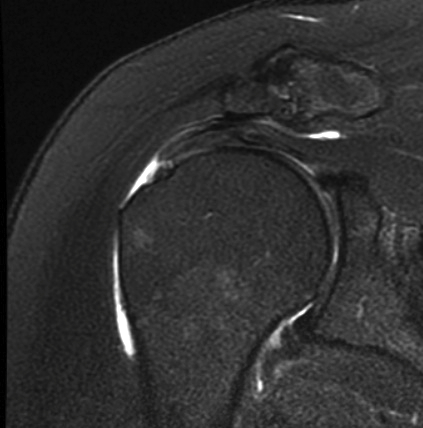
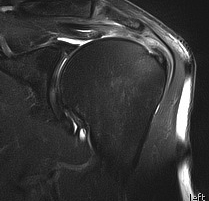
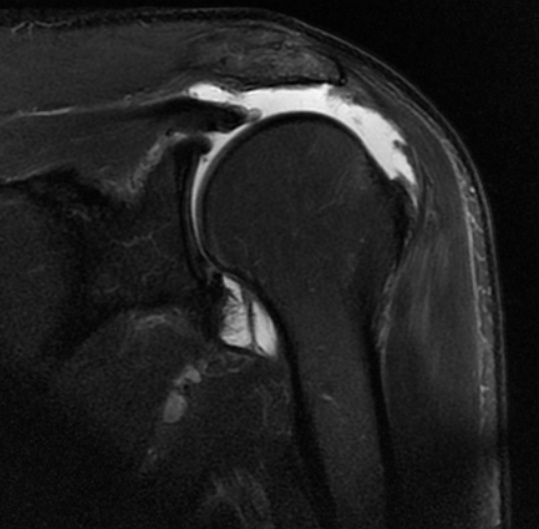
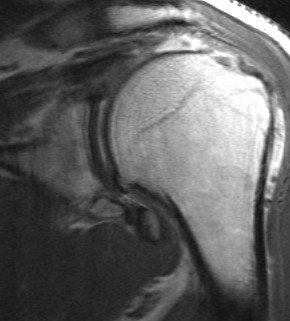
MRI
Look for
- SS / IS / SSC / biceps
- PT v FT
- size of tear
- retraction
- atrophy / fatty infiltration

Partial thickness tears
- best seen on T1 with gadolinium
- see if communicates from GHJ to SA space
For more MRI see
- massive tears
- partial thickness tears
- full thickness tear
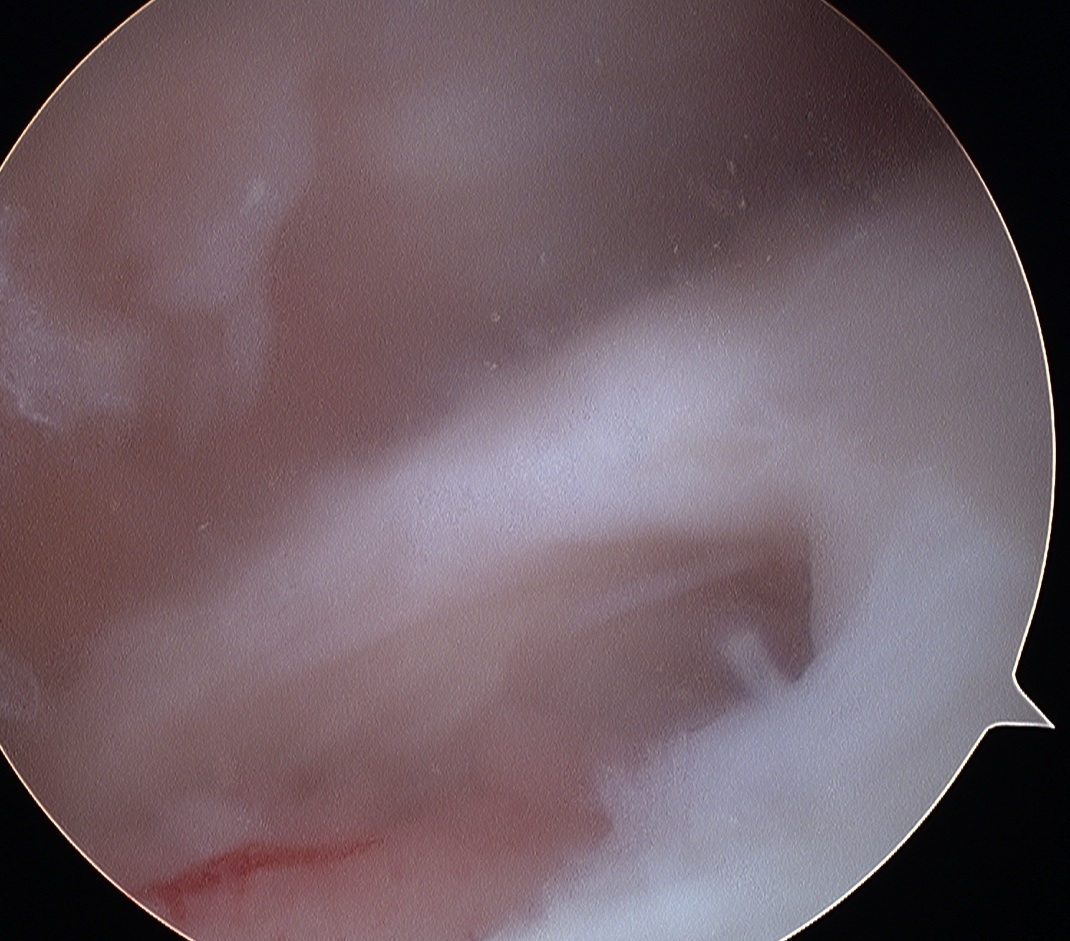
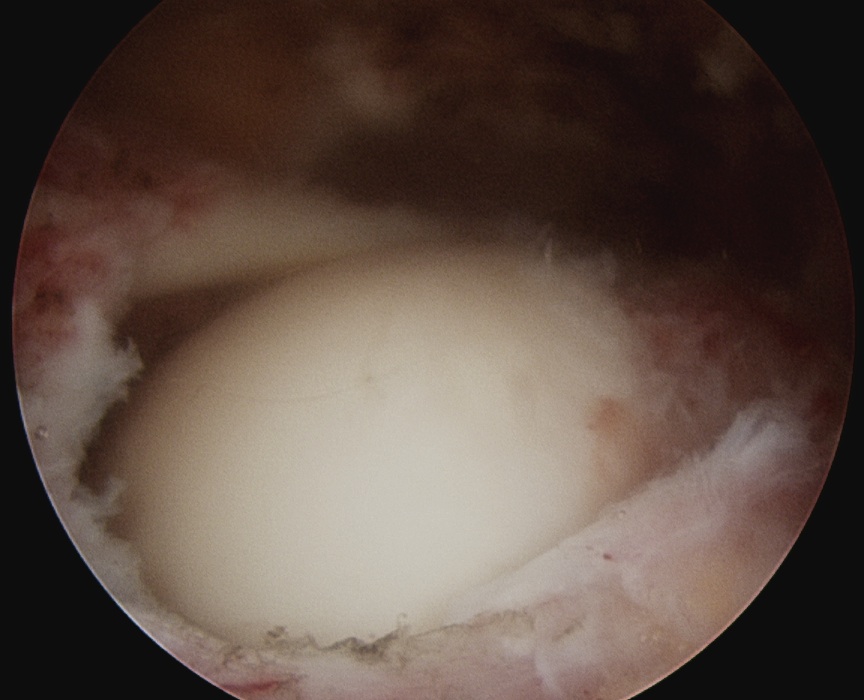
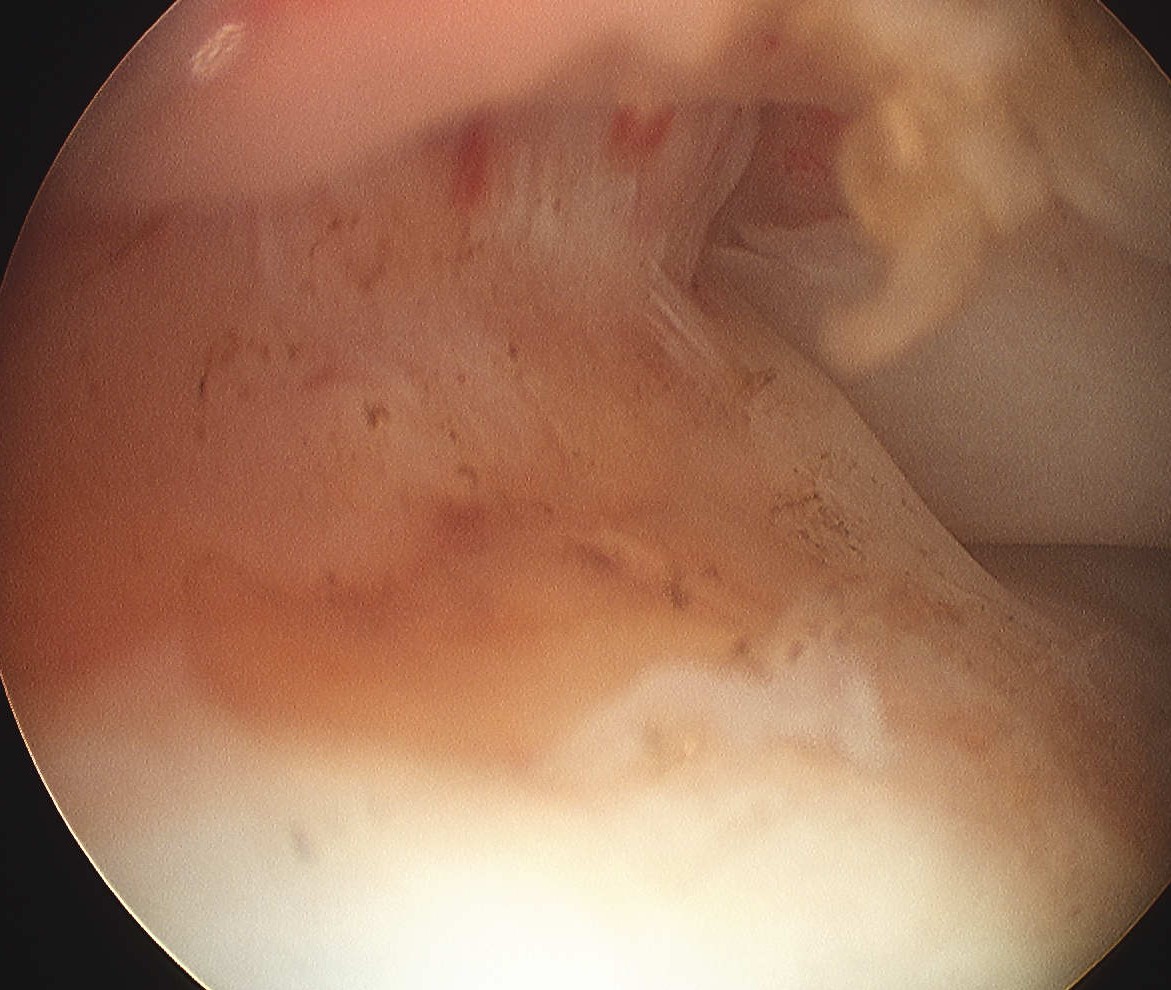
Arthroscopy
Gold Standard
- assess for partial articular tears in GHJ
- assess for bursal sided tears in subacromial space
Management Guidelines
1. Repair all acute full thickness tears
2 Repair chronic full thickness tears
- young patients
- after failure non operative management
- with disability 2° weakness or pain
3. Observe chronic tears with no disability
- especially in elderly
- Prospective cohort study (n=452) with symptomatic, full-thickness, atraumatic cuff tears
- 6-12 weeks of standardised rehab, then followed for 10y
- only 27% elected for surgery (most in first 6 months)
- low expectation of rehab, workers comp., and high functional demand predicted later surgery
Non-operative Management
As per impingement
- satisfactory outcome in 50%
- no symptoms of pain or weakness
- both PT and FT tears
