Definition
Mid-substance calcification of the rotator cuff
- part of a metaplasia secondary to hypoxia


Aetiology
2 groups of patients
1. Degenerate Calcification
Dystrophic calcification of degenerative cuff
- necrotic fibrillated fibres act as nucleus for calcium
- occurs at the cuff insertion
- usually smaller
These patients do not have calcific tendonitis
- older patient group
- different histology
2. Calcific Tendonitis
Cause
Reactive Hypoxic Calcification Theory
Cells undergo metaplasia to fibrocartilaginous cells
- fibrocartilage cells accumulate intracellular calcium
Codman proposed cuff hypoxia as the causative factor
Classification
1. Pre-Calcific stage
Fibro-cartilaginous metaplasia
- tenocytes transformed to chondrocytes
- hypoxia
2. Calcific Stage
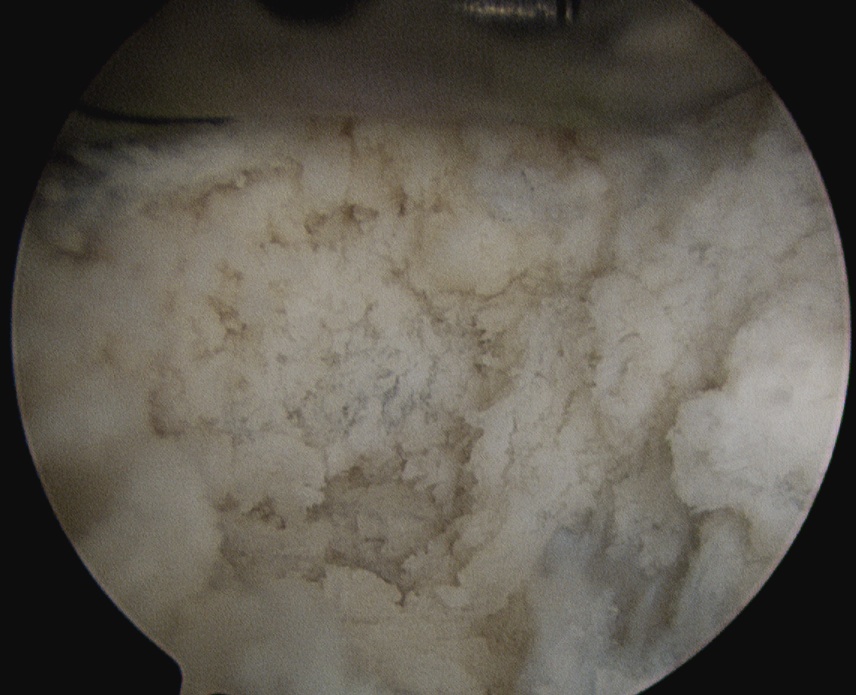
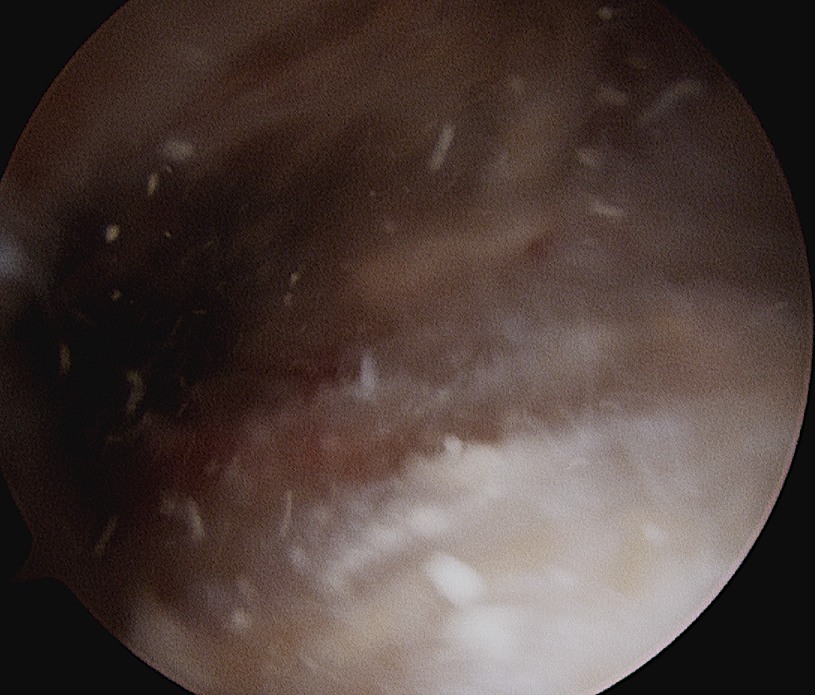
A. Formative Stage
- no or chronic pain
- "Chalk" appearance
- calcium crystals in matrix vesicles
- crystals may be in the form of phosphates / carbonates / oxalates / hydroxyapatite
B. Resting Stage
- fibrocartilage surrounds deposits
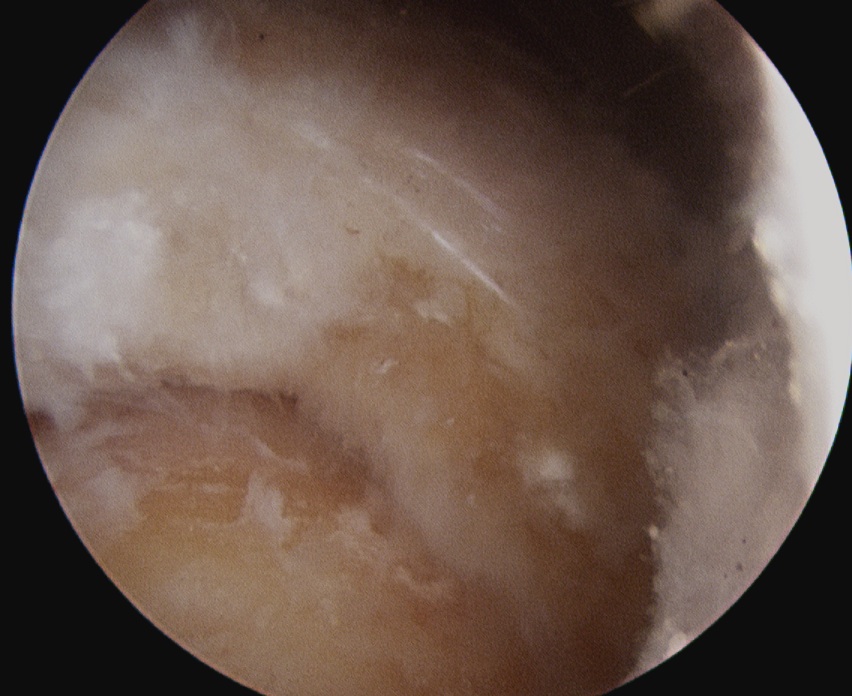
C. Resorptive Stage
- acute pain
- "Toothpaste" or fluffy appearance
- macrophage resorption / calcium granuloma
3. Post-Calcific Stage
Area heals to scar
- granulation tissue fills space left by calcium
- Type III collagen -> Type I
Epidemiology
Accounts for 10% all consultations for painful shoulder
Peak 40 years
- diabetes
- F > M
SS most common tendon
- IS less common
- SSC rare
Asymptomatic patients can have cuff calcium on xray
Clinical Presentation
Usually acute pain
- Resorption Stage
- background of absent to mild chronic pain of the Formative Stage
Patients may present to ED
- severe pain
DDx infection
DDx
Cuff / Biceps Tendinopathy
Freezing Shoulder
Brachial Neuritis
Septic Shoulder
Gout / CPPD
IHD
X-ray


Calcium typically supraspinatous
- mid-cuff
- 1-1.5 cm from insertion
- 1-1.5 cm in size
ER AP Xray
- shows SSC


IR AP Xray
- shows IS & Tm
Painful Resorptive / Type 1
- fluffy, with poorly defined margin
- irregular density
- can rupture into bursae as a crescent like streak
Chronic Formative / Type 2
- discrete, well defined deposit
- uniform density
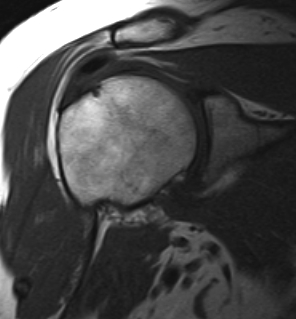
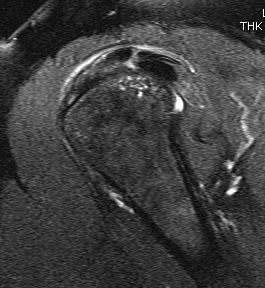
MRI
Low signal on T1
Oedema on T2
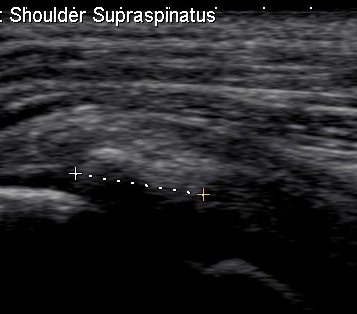
US
- more sensitive than Xray ~100%

Bloods
Check serum glucose / uric acid & iron
Management
Non operative Management
Options
1. NSAIDS
- may impair resorption
2. HCLA
- no effect NHx
- may impair resorption
3. ECSW Therapy
4. Ultrasound guided needling and aspiration
Extracorporeal shock wave therapy

Peters Skeletal Radiol 2004
- RCT
- 90 patients
- treatment group complete resolution in 86%, reduction in size in 13.4%
- control group 0 disappeared completely, 9% partial reduction
- significant reduction in pain and improvement in function at 4 weeks
- no adverse affects
Effectiveness directly related to energy
- 0.44 mJ/mm3
Needle aspiration and irrigation
Aim
- drain a substantial portion of the calcium
- stimulate resorption of remainder
Indications
- resorption phase (soft, toothpaste material)
Contraindications
- small deposits
- formative phase (hard, chalky material)
Technique
- US guided procedure under LA
- one needle into deposit, inject saline
- one needle into deposit, aspirate
- create inflow outflow
- want minimal punctures for this to work
- distinguish Formative vs Resorptive
Complications
- very painful for first 2-3 days
Results
Aina et al Radiology 2001
- excellent results in 74%
Serafini et al Radiology 2009
- non randomised controlled trial
- patients treated better at 1 month / 3 months and 1 year
- no difference long term
Krasny JBJS Br 2005
- prospective RCT
- improved results by performing US needling followed by ECSW therapy
- c.f. ECSW alone
Operative Management
Indications
- severe disabling symptoms > 6 months
- failure of needling / ECSW
Issues
Acromioplasty
- unknown
- alone has been shown to improve patients symptoms
- do so if any acromial or GT evidence of impingement
Marder et al J Should Elbow Surg 2011
- retrospective comparision of 2 groups
- calcium excision v excision + SAD
- SAD much longer time to return to non painful shoulder activity
Options
Open
Arthroscopic and mini open
Arthroscopic
Arthroscopic Technique
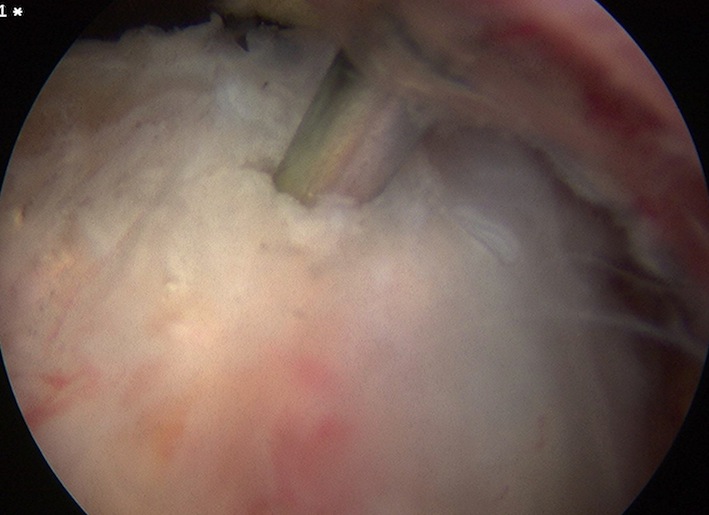
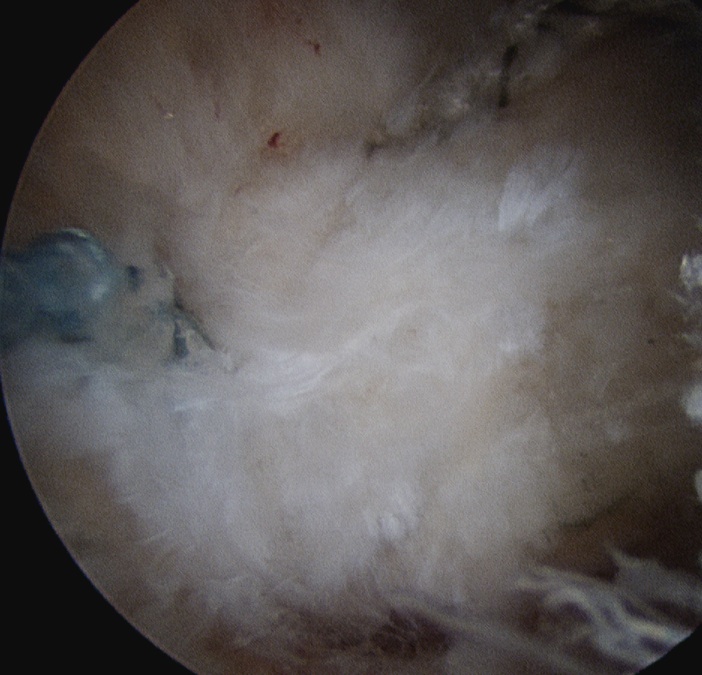
Find Calcium
- remove bursa with shaver
- deposit may be obvious
- however may have to use needle
- get cloud of calcium when find deposit
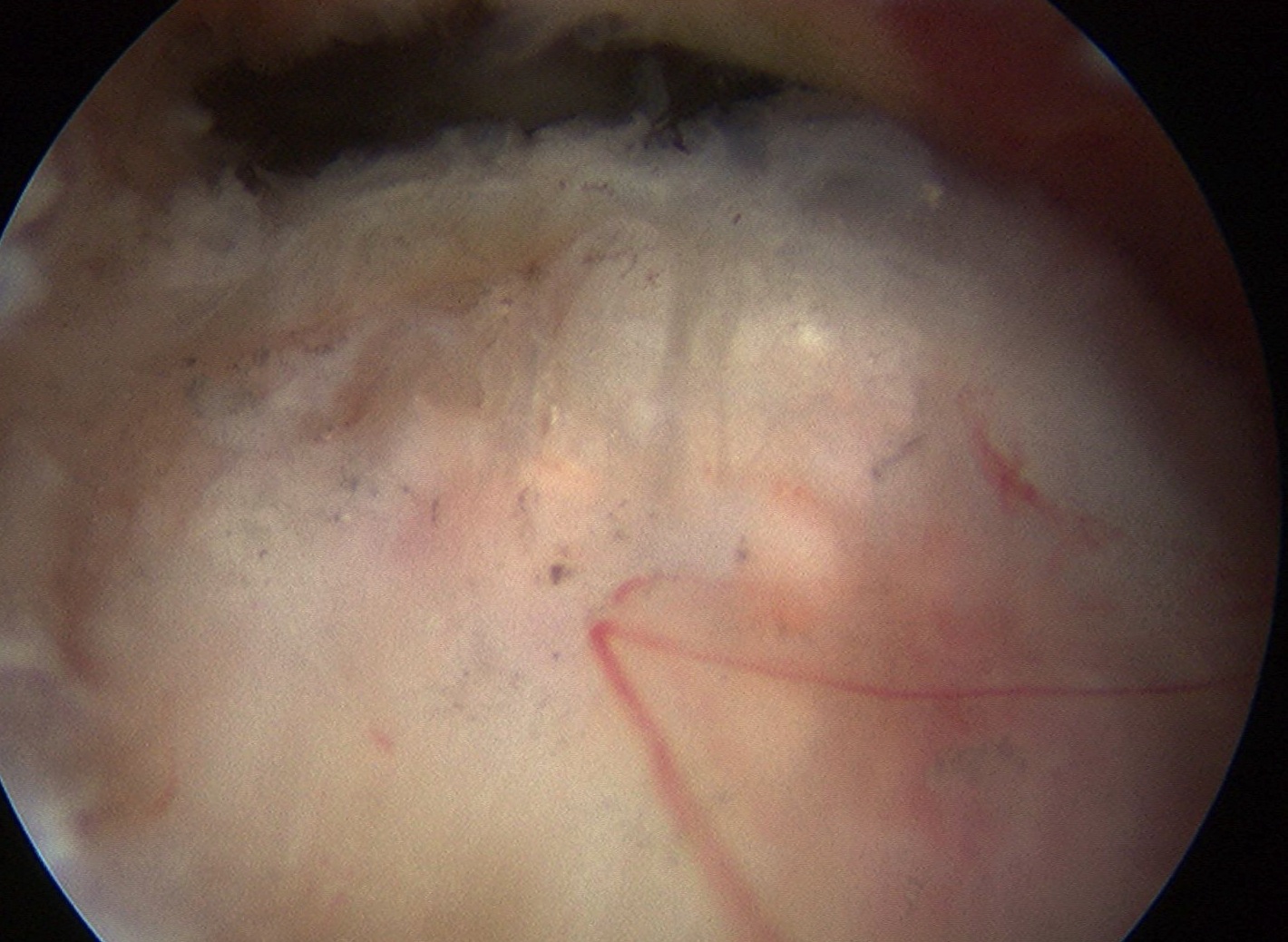
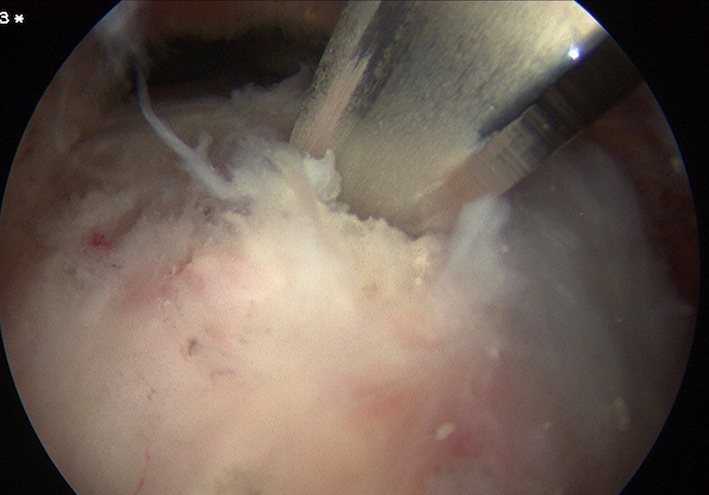
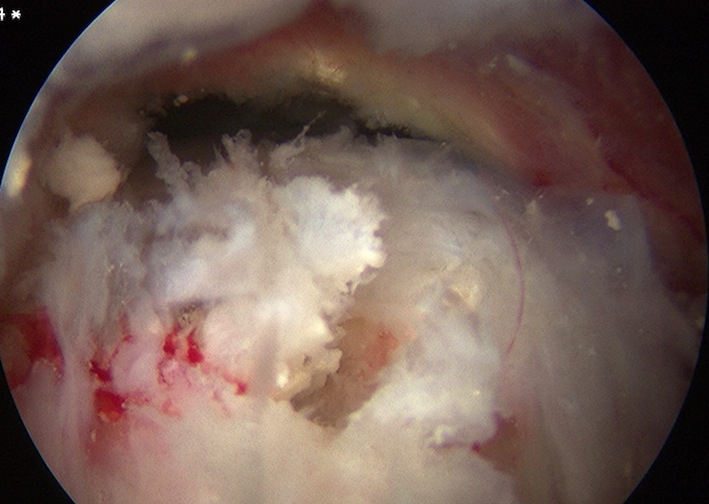
Attempt to longitudinally split tendon
- curette calcium
- lavage +++ to prevent secondary stiffness
- usually don't repair tendon to prevent stiffness
May need to remove entire diseased section and repair
Complications
Secondary stiffness
Pain
- secondary to calcium deposits
- careful shoulder washout at the end of the case
