
Goals
1. Maintain function
2. Reduce pain
3. Prevent or treat pathological fracture
Pathological fracture
- Retrospective cohort study 1064 patients who had femoral nailing for completed pathological fracture vs prophylaxis
- 90 day survival rate same
- 1yr survival rate worse in completed (38%) vs prophylactic (46%)
- Completed pathological fractures associated with more blood loss, more transfusions, longer anaesthetic times and more re-operations (OR 2.5)
- No difference in 30d complication rate
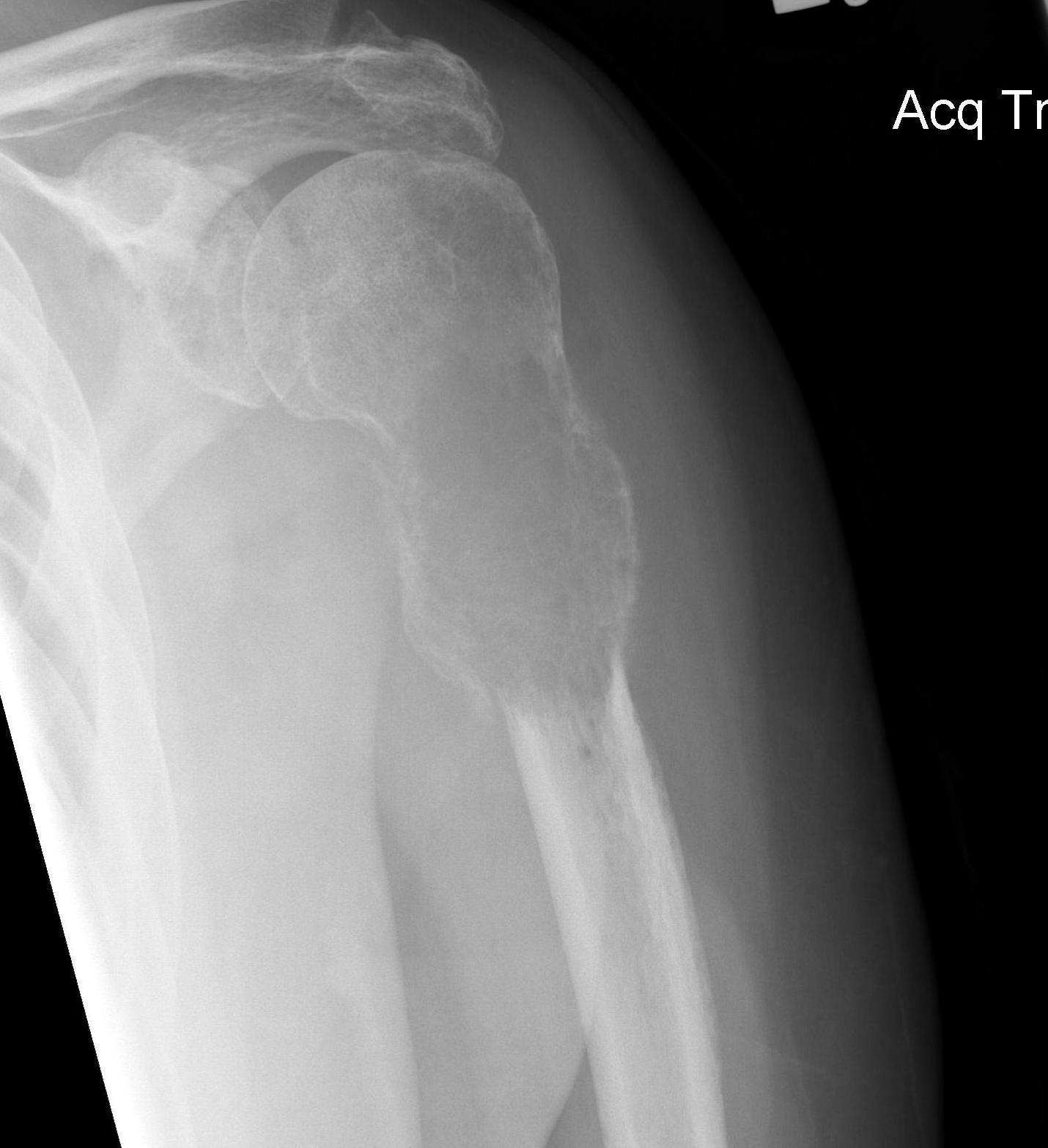
Mirels prediction system for pathological fracture
- quantify risk of pathological fracture
- weighted scoring system
- non fracture group mean score 7
- fracture group mean score 10
- score of 9 fracture risk 33%
Four risk factors
| 1 | 2 | 3 | |
| Site | Upper limb | Lower limb | Peritrochanter |
| Pain | Mild | Moderate | Mechanical |
| Lesion | Blastic | Mixed | Lytic |
| Size | < 1/3 | 1/3 - 2/3 | 2/3 |
Guidelines
Suggest surgical intervention score 9 or more
- 7 or less: radiotherapy
- 8: fracture risk is 15%
Validity
Howard et al Bone Joint J 2018
- reliability of Mirels
- moderate inter-rater and intra-rater reliability
CT based structural rigidity analysis (CTRA)
- 125 patients compared CTRA with Mirels
- CTRA more sensitive (100% v 67%) and specific (61% v 48%)
Management
Aims
1. Appropriate patient selection / estimate life expectancy
2. Stabilize fracture / metastasis and allow full weight bearing
3. Radiotherapy
Estimate life expectancy
Need to live longer than time for recovery from the operation (> 6 - 8 weeks)
Estimates
- online Bayesian Belief Network
- estimates 1, 3, 6, 12, 18 and 24 month survival in patients undergoing surgery for skeletal metastases
- 10 prognostic factors
- age / sex / type of cancer / visceral mets / number of bony mets / lymph nodes mets / path # / Hb / WCC
- 208 patients
- updated PATHFx version 3.0 model demonstrates external validity
Karnofsky performance scale
Ranges from 100 (full function) to 0 (death)
- 80 - 100%: able to work
- 50 - 70%: unable to work, able to live at home, mostly independantly
- 30 - 40%: unable to care for self
- 20%: very sick, active supportive treatment required
- 10%: moribund
Results
Razvi et al Ann Palliat Med 2019
- 170 patients metastatic disease
- estimated clinical survival using Karnofsky
- 75% over-estimated by average 19 weeks
Surgical fixation
Obtain stability / allow load bearing / prevent fracture / obtain union
Location specific
See www.boneschool.com/metastasis/specific management
Radiotherapy
Nonoperative
Chow et al Radiother Oncol 2019
- meta-analysis of single versus multiple radiotherapy / fractions
- no increased efficacy with multiple regimens
- good pain relief
Postoperative
Typically minimum 2 weeks post surgery to minimize wound healing complications
- systematic review of postoperative radiotherapy after surgery for metastasis
- reduces local recurrence and provides effective pain relief
Kraus et al Adv Radiat Oncol 2021
- postoperative radiotherapy
- no difference between single or multiple regimens
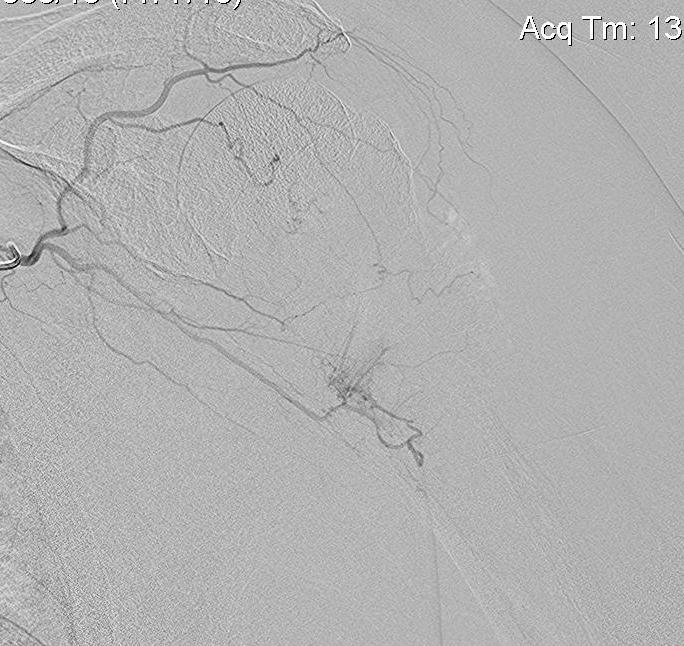
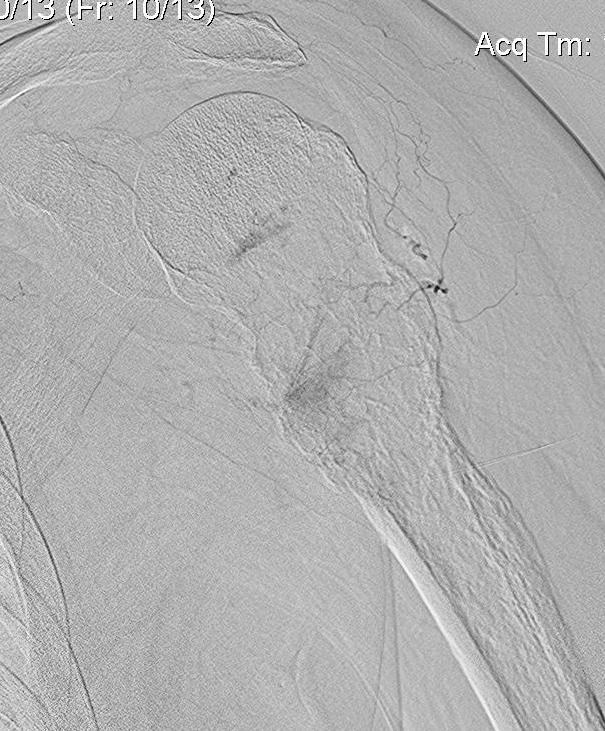
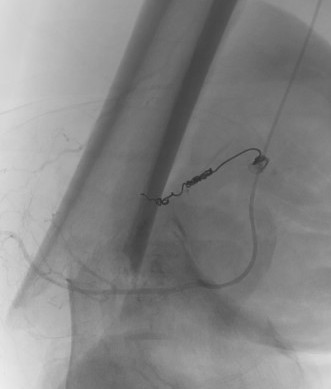
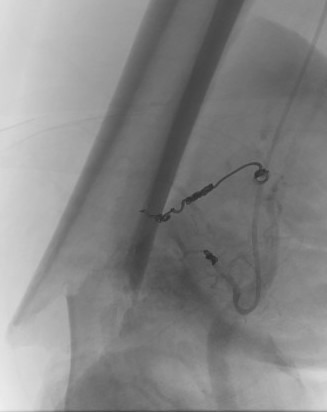
Pre-operative Arterial Embolization
Indications
- renal cell carcinoma
- thyroid carcinoma
Results
- embolisation of RCC metastasis in 107 patients
- success in 96%
- all patients had variable ischemic pain for 2 - 4 day
- 41 cases with embolization prior to surgery compared to 41 cases without
- embolization reduced blood loss, transfusion, and surgical times

Medical treatment
Bisphosphonates
O'Carrigan et al Cochrane Database Syst Review 2017
- bisphosphonates in breast cancer
- 44 RCT's and 37,000 patients
- reduce risk of skeletal metastasis, reduce bone pain, and increase overall survival
Denosumab (monoclonal antibody to RANKL)
- denosumab
- evidence reduces hypercalcaemia of bony metastasis
- can slow bony metastasis progression
