Definition
Progressive and chronic disorder associated with cord cavitation & gliosis
Effects
Muscle wasting
Dissociate anaesthesia
Scoliosis
Neuropathic arthropathy
Epidemiology
M > F
No familial tendency
Aetiology
1. Idiopathic
2. Hindbrain Herniation / Arnold- Chiari Malformation
- abnormal pressure & circulation of CSF
3. Post-Traumatic
- occurs in 3%
- ? due to subarachnoid block 2° to adhesive arachnoiditis
- more common in complete tetraplegics
- delayed presentation of deterioration
- 3/12 - 30 years
4. Arachnoiditis
5. Intramedullary Tumour
6. Extrinsic Compression With central cord necrosis
7. Necrotic Myelitis
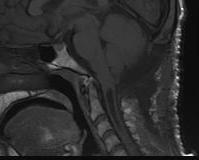
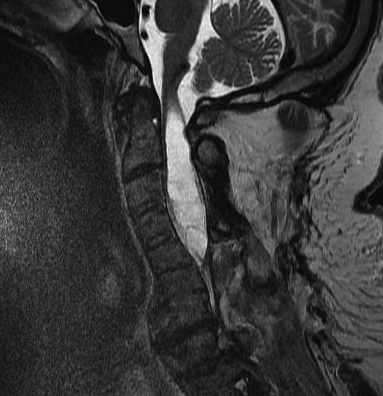
Arnoldi-Chiari Malformation
Congenital abnormality of Cerebellar Tonsils
- herniation of medullary tonsils through foramen magnum into cervical canal
- block CSF flow through foramen Lushka & Malgagne blocked
- often need AV shunt
Type I
- communicating

Type II
- non communicating
- usually larger and associated with spina bifida
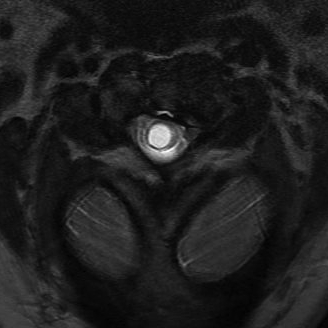
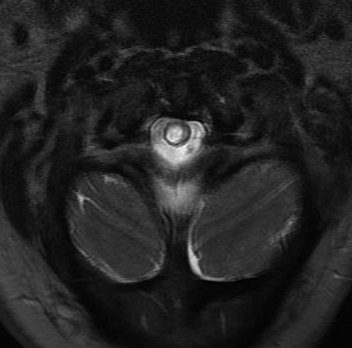
Pathology
Cord damage
- anterior dissection of cavity with interruption of decussating spinothalamic fibres
- effects pain & temperature
- extension into lateral corticospinal tracts
Most common in lower C Spine
- may progressively extend up to medulla & down to lumbar
- fluid-filled tubular cavity
- separate from but usually communicating with central canal
Spastic Paraparesis
- involvement of 2° order neurones
Pain with causalgia
Consequences
Dissociative sensory loss
Spastic paraparesis
Neuropathic joints especially GHJ
Scoliosis as syrinx is irritative
- scoliosis not due to muscle imbalance as neurology most commonly normal
Histology
Cystic space
- lined by thick layer of glial tissue
- gliosis with tendency to infiltrate white matter
Associations
Craniovertebral anomalies
Platybasia
Hydrocephalus
Myelomeningocoele
Cause of deterioration in Spina Bifida
Shunt malformation
Arnold Chiari
Cord Tether
Diastomatomyelia
Neuroenteric cyst
Syrinx
Clinical Features
Classic Triad
1. Dissociate sensory loss in cape distribution
- loss of pain and temperature
- preservation of light touch (dorsal columns)
- arms and trunk with cervical
- legs with lumbar
2. Muscle wasting / weakness with diminished reflexes
- in UL due to direct pressure on anterior horn cells
3. Atypical high thoracic kyphoscoliosis
Site of syrinx
1. Cervico-Thoracic
- dissociate sensory loss in arms & trunk
- weakness & wasting of arms
- absent abdominal reflexes


2. Lumbar
- dissociate lumbosacral sensory loss
- weakness & wasting of legs & pelvic girdle
- diminished reflexes / Babinski negative
- impaired bowel & bladder function
3. Cervico-Medullary
- AKA syringobulbia
- palatal & vocal paralysis / dysarthria
- nystagmus / dizziness / tongue weakness
X-ray
Spine
Base of skull
MRI
Most sensitive investigation
- main differential is oedema
- need T1 image
Look for obstructions
- ACM
- spinal cord tumours
DDx
Amyotrophic Lateral Sclerosis / Motor Neurone Disease
MS
Cervical Myelopathy
Thoracic Outlet Syndrome
Klippel-Feil Syndrome
Cord Tumour
Brainstem Infarct
Operative Management
Indications
Rapid progression of neurology
Short History
Respiratory compromise
Pseudobulbar Palsy
Pre-spinal corrective surgery
Technique
Shunt
- Syringo-Cisternal
- Syringo-Peritoneal
Suboccipital decompression & C1-2 laminectomy
Orthopaedic Implications
Neuropathic Joints
Syrinx is most common cause of UL charcot joint
- shoulder
- elbow
- hot swollen joint may be first presentation of syrinx
DDx
- infection
- peripheral neuropathy - DM / Leprosy / Tabes dorsalis
Scoliosis
Scoliosis is usually 1° Presentation of syrinx
- curve is idiopathic type
- often left sided thoracic
- corresponds with level of syrinx
Males > Females
- 25% if < 10 year old
- 20% males with scoliosis have syrinx compared with 2% of girls
Neurological deficit usually subtle or absent
- axillary sensation absent
- absent abdominal reflexes
Treatment
- must correct syrinx first
- malignant progression if syrinx untreated
- cyst rupture during scoliosis surgery may be fatal
- progresses like idiopathic once syrinx treated
