Definition
Displacement of proximal femoral epiphysis in the immature hip
- due to imbalance of mechanical and endocrine factors
Epidemiology
Age Peak Incidence : M 12-14; F 11-13; Slight downward trend due to earlier maturation of children
L hip > R
10 / 100 000
Bilateral SUFE
No endocrine abnormality
- 20% at time of of diagnosis
- another 20% during diagnosis
- up to 60% with long term follow up
Endocrine abnormality
- up to 75%
Risk Factors
Demographic Factors
- Increased Weight and Height (50% over 95th percentile weight; 50% over 97th percentile height); Average BMI 27
- Race : Increased risk in Black pts (4X) ; Polynesian ; Hispanics
- Sex : Male 2.5 x risk
- Family History - 7 % risk to other family members
Hip Mechanical Factors - increased shear forces
- increased slope (at adolescence growth plate goes from horizontal to vertical position)
- increased retroversion Southwick angle > 14
- reduced neck shaft angle
Endocrinopathies
Imbalance of
- Testosterone - causes physeal fusion
- Growth hormone - causes physeal hypertrophy / weakens
Causes
- hypothyroidism
- hypopituitary
- acromegaly or growth hormone supplementation
- CRF/ Renal Osteodystrophy
Other
Connective Tissue Disorders - Marfan's / Downs / Ehlos Danlos
Chemo therapy / DXRT
Pathology
Widened hypertrophic zone
- constitutes 60% of physeal width
Abnormality at Hypertrophic & Proliferative Zones junction
- failure occurs here
- disordered chondrocyte columns
- decreased number of cells
- cells smaller
- increased number of dead and degenerative cells
Head remains in acetabulum via L. Teres
- neck displaces anterosuperior on physis and ER
- head slips posterior / inferior on neck
Classification
Chronological
Acute < 3/52 symptoms
Acute on Chronic
Chronic >3/52
Morphological
Southwick Slip angle
- Wayne Southwick ; 1st Chairmen of Orthopaedics at Yale University
- lateral X-ray / frogs legs
- epiphyseal-shaft angle
- angle of interest is the angle of the affected side subtracted from the normal contralateral side ; if contralateral SUFE then 12 degres as normal
- <30° / 30- 50 / >50°
- mild / moderate / severe
Stability
Loder JBJS 1993
Stable
- able to weight bear / 0% AVN
Unstable
- unable to weight bear / AVN rates 10 - 60%
History
Overweight adolescent boy hip or knee pain; 30% present only with knee pain
Examination
Limps
Walk with ER (chronic) i.e increase in foot progression angle
Obligate abduction and external rotation with flexion
Limitation IR / Abduction
LLD (real and apparent)
X-ray
AP
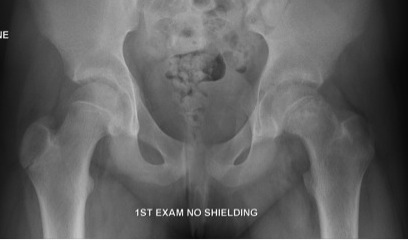
Trethowan Line / Kleins Line
- line along superior neck usually transects 20% head
- originally described as AP but can also be used as lateral
Widened physis
Inferomedial remodelling in chronic slip
Metaphyseal Blanch Sign of Steel
- Increased cresenteric density in the metaphysis due to overlapping of the metaphysis with the epiphysis
Capener's Sign
- the posterior acetabular margin normally cuts the medial corner of the metaphysis
- in a slip the whole of the metaphysis remains lateral to the acetabular margin
Frog Leg Laterals / Shoot through lateral

Shoot through lateral
- best to avoid frog leg lateral as may displace slip
Posteriorly displaced & angulated
Measure Southwick Angle
- calculate severity of slip
- also estimates risk of slip of other side / looking for retroversion
Management
Aims
1. Prevent further slip / obtain physis fusion
- 30% will continue untreated
2 Prevent deformity and OA
- MUA / ORIF / osteotomy
3. Avoid complications
Algorithm
Loder RT et al. What is the best evidence for treatment of slipped capital femoral epiphysis?
Journal of Pediatric Orthopaedics. 2012 Sept : 32 (Suppl 2) S158 - 65
Stable : Insitu Pinning current gold standard
Unstable : Two schools of thought
1) < 24 hours old
- Consider treatment as a surgical emergency
- urgent reduction (gentle traction, flexion and internal rotation) +/- joint decompression
- probably results in lowest AVN rates (Petersen et al - refer below)
- alternatively consider discussion with tertiary paediatric referral centre
2) > 24 hours
- Discuss with specialist paediatric centres
- possibility of surgical dislocation and realignment i.e. Modified Dunn Procedure
In Situ Pinning
Gold Standard (Techique refer below)
CT post operatively
- ensure no screw protrusion
TWB 6/52
Serial Xray
- ensure epiphysis doesn't grow off screw
- screw can break / can lose position
- observe til physis closes
- no indication to remove pin
Results
Weinstein et al JBJS Am 1991
- 40 year follow up of 155 hips
- some pinned in situ / some realigned / some reduced
- rates of OA / AVN / chondrolysis increased with severity of slip
- rates of OA / AVN / chondrolysis increased with reduction / realigned
- regardless of severity of slip, pinning in situ had best results with lowest complications
Closed Reduction Prior to Pinning
Disadvantage
Traditionally associated with higher risk AVN
Advantage
Theorectical
- may decrease AVN in severe, unstable hips
- prevent severe deformity / late OA
Indication
Acute & unstable < 24 hours
Results
Peterson et al J Paediatr Orthop 1997
- 91 cases of severe, acute, unstable slips
- 42 closed reduction < 24hrs AVN 7%
- 49 closed reduction > 24hrs AVN 20%
- hypothesised that had acute obstruction of epiphyseal vessels
- timely decompression allows revascularisation
- treat an acute unstable slip as per a fracture
- these have up to 50% AVN rate anyway
- emergency operation
Chen et al J Paediatr Orthop 2009
- 30 acute, unstable slips
- 25 closed reductions and 5 open reductions with release hematoma
- 4 cases of AVN
Open Reduction Prior to Pinning
Indications
- severely displaced slips
Reasoning
- moderate or severe slips do poorly in long term
- best treatment is intra-capsular reduction or osteotomy
- risk AVN either way
- acute open reduction easier
- also decompress hip
Modified Dunn Procedure
Ziebarth et al. Capital realignment for moderate and severe SCFE using a modified dunn approach.
Clin Orthop Relat Res. 2009; 467(3): 704 - 16
- Ganz type transtrochanteric approach
- Z shaped capsulotomy to preserve superior vessel along neck, along anterior acetabulum and inferior neck
- capsule banana skinned off neck
- hip dislocated via adduction and external rotation and transection of the round ligament
- epiphysis taken off neck, still attached to capsule
- intraoperative monitoring of epiphyseal perfusion via 2mm hole drilled in the anterior neck or via insertion of ICP monitor into the epiphysis
- neck debrided to avoid tensioning of posterior vessels
- head replaced and pinned as per normal
Results
Sankar WN et al. The modified Dunn procedure for unstable slipped capital femoral epiphysis: a multicentre prospective.
JBJS (Am). 2013; 95:585- 91.
- 26% Rate of AVN
- 15% Revision of metalwork rates
- therefore capable of restoring anatomy but ongoing risk of AVN and metalwork complications.
Prophylactic Pinning
Issues
Can justify but may cause complications
- i.e. chondrolysis, subtrochanteric fracture secondary to screw
Incidence bilateral slips
- unknown
- may be > 35%
- high incidence of asymptomatic and mild contralateral slips
Major indications
- young i.e < 10 years
- unreliable parents
- geographic isolation
- Secondary SUFE eg endocrinopathy
Technique of Pin in Situ
Vumedi Insitu Pinning technique
https://www.vumedi.com/video/in-situ-fixation-for-stable-slipped-capital-femoral-epiphysis/
Set up
1. Supine on radiolucent table
- very easy to set up
- much faster if pinning both sides / reduced set up
- theoretical risk of displacing slip / inadvertant manipulation
- lateral by flexing and full ER of hip / frog legs
2. Traction Table
- easy to get AP and lateral
- need 2 set ups for bilateral pinning
- takes longer in this regard
Technique
Draw anterior and lateral lines
- get AP, draw line mark using radiopague ruler to centre of head
- get lateral, repeat
- intersection of points is incision site
Stab incision
- guide wire percutaneously to neck
- more anterior entry point on femoral neck required the more the epiphysis is displaced posteriorly
- more anterior entry point ensures less likely to start at a subtrochanteric position and risk stress fracture
- central in head on both views
- ensure don't penetrate head
- cannulated drill
- 6.5/ 7.0/ 7.3 screws
- 8-10 mm or 4-5 threads across physis
- do far and away screening / approach withdraw; circumferential screening
- this ensures screw is not in joint
