Ossification
Distal tibia
- appears by 2 years
- closed at maturity
- asymmetrical closure
- central initially, then posteromedial to anterolateral
- accounts for Tillaux and Triplanar fractures
Distal fibula
- appears by 2 years
- closes 2 years after distal tibia
Medial Malleolar Extension
- begins age 7
- closes age 10
Types of Fractures
SH I
SH II
SH III - medial malleolus / Tillaux
SH IV
Triplanar
SH V
Salter Harris I


Incidence
15% of distal tibial physeal fractures
Distal fibular most common
Mechanism
Through zone hypertrophy
Management
Operative if require realignment
Salter Harris II


Epidemiology
40% of distal tibial physeal fractures
Pathology
Thurston-Holland fragment
- large metaphyseal component
Non operative Management
Acceptable distal tibial alignment
Short leg case 6 weeks
Operative Management


Unacceptable alignment
Attempt closed reduction
- sometimes anterior periosteum can block reduction
- anterior approach / remove periosteum / reduce fracture
Unstable reduction
- screws into Thurston Holland fracture if large enough
- if fragment too small need fixation across medial malleolus into metaphysis
Late presentation 7-10 days
- may be best left
- prevent damage physis
- later osteotomy if needed
Complications
LLD
- complete growth arrest
Angular deformity
- partial growth arrest
- uneven Harris growth lines
Salter Harris III / Medial Malleolus


Issues
2 problems
- articular disruption
- possible physeal bar
Management
ORIF any > 2mm step
- physeal cannulated screws
Complications
Joint incongruity
Growth arrest
Salter Harris III / Tillaux



Definition
- SHIII of anterolateral distal tibia
- epiphyseal avulsion of AITFL
- supination / ER injury
Incidence
- usually near skeletal maturity
- transitional fracture
- as distal tibial physis is closing
- anterolateral fragment is last to close
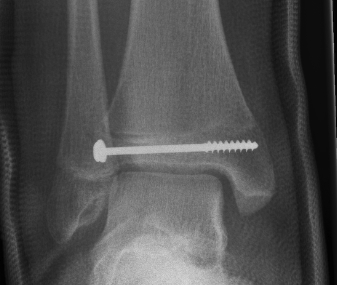
Management
ORIF
- reduce articular step / prevent physeal bar
- anterolateral incision to reduce
- either anterolateral 4 mm cannulated screw or
- place screw percutaneously from medial side
Salter Harris IV
Incidence
- 25%
- usually associated with triplanar
Complications
- bony bar
- articular step
Management
ORIF > 2 mm step
- restore articular surface
- reduce risk of bar
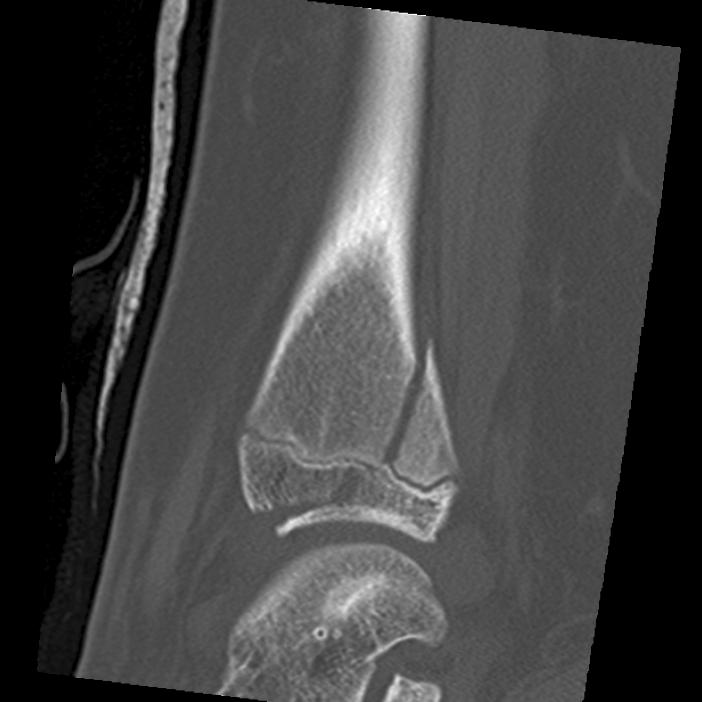
Triplanar Fracture

Definition
- fracture in coronal, sagittal and transverse planes
- 2, 3 or 4 part
Varieties
2 part
- can be medial or lateral based of site of main distal fragment
- typically anterolateral epiphysis attached to posterior metaphysis
- anteromedial intact distal tibia
3 part
- additional separate anterolateral epiphysis / Tillaux
4 part
- additional separate metaphyseal fragment
Extra-articular
- fracture extends into medial malleolus
Xray
Type III / Tillaux on AP
Type II on lateral
CT
Type III on coronal
Type II on sagittal
3 point star on axial
Management
ORIF
- > 2mm displacement
- usually anterolateral approach to reduce
- epiphyseal medial-lateral screw
- metaphyseal AP screw
Complications
Growth arrest 10%
Salter Harris V
Usually late diagnosis
Growth arrest / LLD
