Philosophy
Need the least amount of constraint necessary to obtain sufficient stability
Increasing constraint
Advantages
- increase stability
Disadvantage
- increase stress at implant host interface
3 Types
1. Unconstrained
A. Posterior cruciate retaining
B. Posterior cruciate substituting / Posterior stabilised
2. Constrained non hinged
3. Constrained hinged
CR / PCL retaining
Known Advantages
1. PCL acts as knee stabiliser
- prevents anterior dislocation of femur on tibia
- provided is correctly balanced
2. No risk of Cam jump / Post wear
3. Improved bone stock preservation on the femoral side
Theoretical Advantages
1. ? Improved knee flexion
Theory
- preserves femoral rollback / increases flexion
- posterior shift in the femoral-tibial contact point in the sagittal plane as the knee flexes
- posterior shift allows the posterior femur to flex further without impinging on the posterior tibia
- allow better flexion by allowing rollback
- kinematic studies show that this rollback is imperfect
- combination of rolling and sliding
Victor et al JBJS Br 2005
- II study of PS v CR
- showed improved femoral rollback in PS
Maruyama J Arthoplasty 2004
- RCT of PS v CR
- improved ROM in PS
2. ? Increased quadriceps strength, stair climbing and proprioception
Swanik et al JBJS Am
- RCT of CR v PS
- no detectable difference in proprioception or balance
3. Fewer patella complications
Disadvantages
1. More difficult to balance
- PCL often scarred
- tight in flexion / limited flexion / anterior lift off
- can downsize femoral component, increase posterior slope, recess PCL
2. Increased wear in early designs
- without ACL, rollback is a combination of roll and slide
- for rollback to occur the tibial PE must be relatively flat
- this created high contact stresses and rapid poly wear and failure
New designs
- increased conformity
- congruent PE insert allowing less rollback
- reduces contact stresses on PE
- relegates PCL to a static stabiliser to prevent anterior dislocation of the femur
- increased knee flexion is then obtained by having a posterior offset centre of rotation (4-6mm) and recreation of normal posterior slope
Can actually get paradoxical rollback
- actually rolls forward
- increases anterior wear
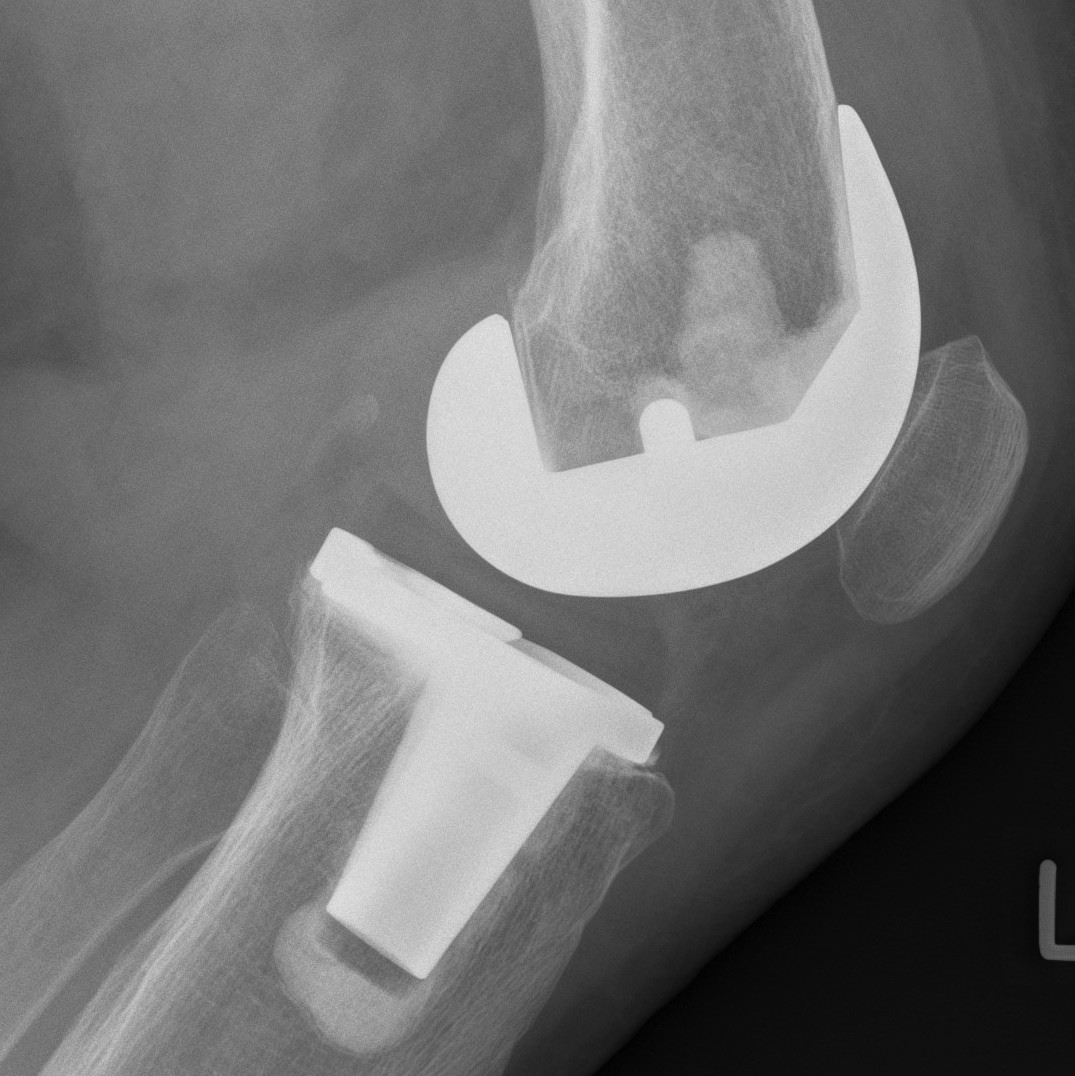
PC substituting / PS
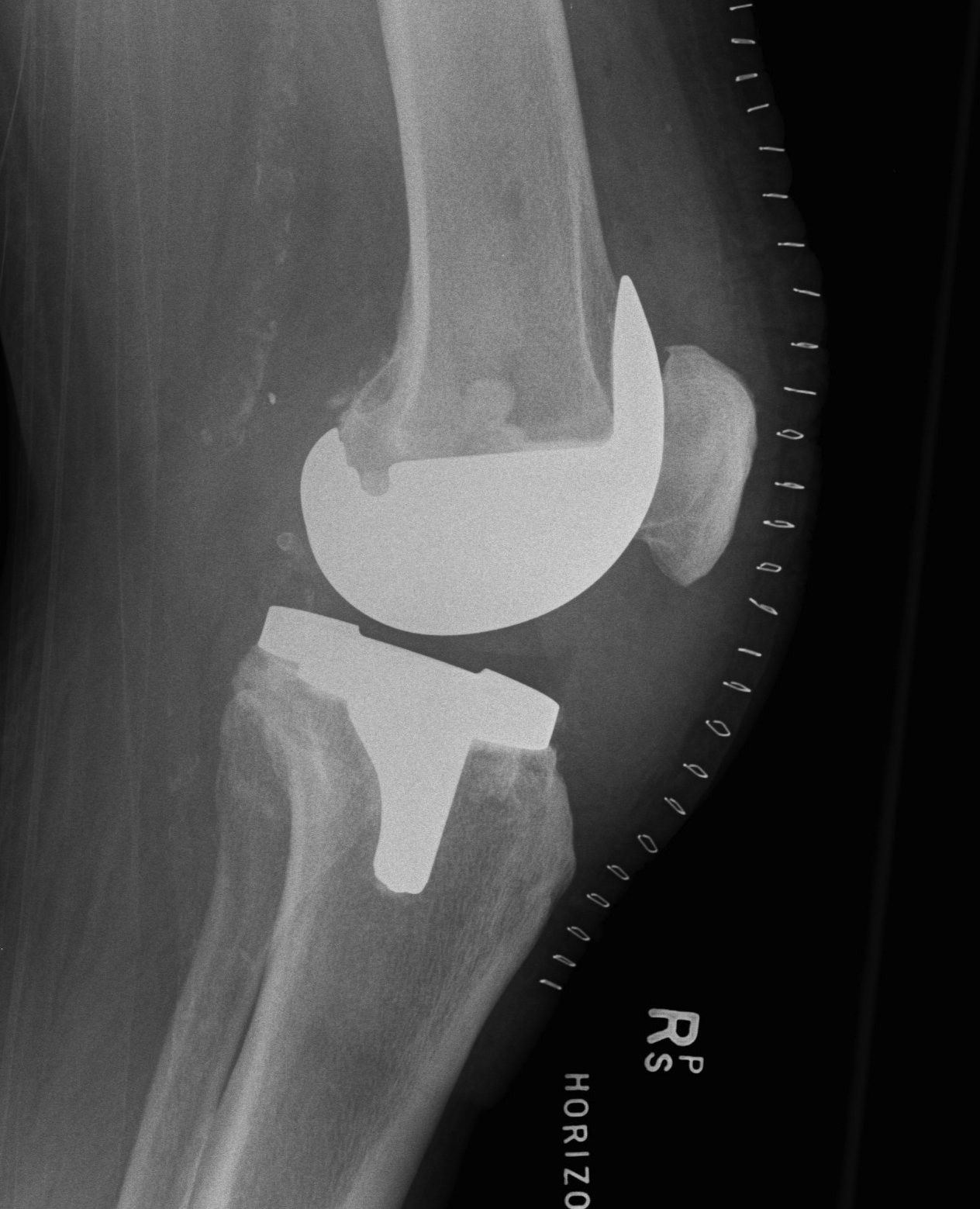
Design
1. Tibial PE post with a femoral cam
- femoral cam engages the post at a designed flexion point
- prevents femur translating anteriorly
- with further flexion get rollback
2. Deeply dished articular surfaces
- increased conformity
3. "Third condyle"
- limits excessive tibial translation
Known Advantages
1. Eliminate risk PCL rupture
2. Easier to balance / correct severe deformity
Theoretical Advantages
1. ? Reduced wear
- increased conformity
- because rollback is mechanically controlled, can have congruent articular surfaces
- reduces contact stresses on the tibial poly
Disadvantage
1. Risk of Cam jump
- must have good balancing
- if loose flexion gap femur can jump over the tibial post
- this can also occur with good balancing
- in hyperflexion, the femur will impinge on the tibial post and be levered over
- may wish to have CR if postoperative flexion is anticipate to be > 130o
2. Increased loss of bone stock
- due to making cuts for box in femur
3. Increased wear of tibial post in femoral cam
- theoretic risk
4. Increased patella clunk (older designs)
Indications
1. Previous patellectomy
- better outcomes with PS c.f. CR


2. Inflammatory conditions
- risk late PCL rupture
3. Previous PCL rupture
4. Over-release of PCL during surgery
5. Difficult balancing
- valgus knee
- severe varus knee
Results
ROM
Harato et al Knee 2008
- multicentred RCT of PS v CR Genesis II at 5 year follow up
- no difference in functional assessment, patient satisfaction or complication
- improved ROM in PS
Survival
Australian Joint Registry 2010
- significantly higher revision rate with PS
9 year survival rate
- minimally stabilised 4.8%
- posterior stabilised 6.0%
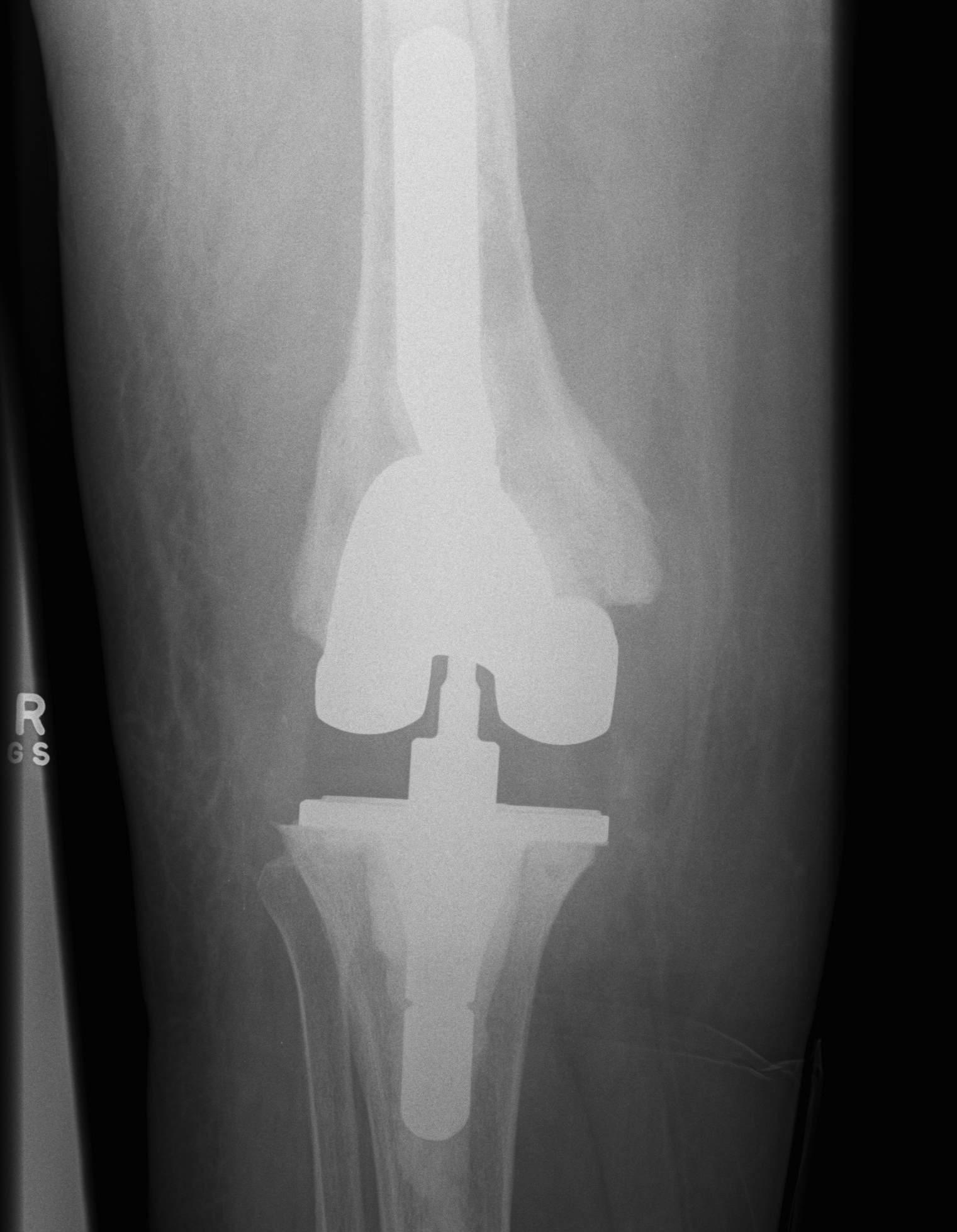
2. Constrained Non Hinged / Varus Valgus Constrained (VVC)


Design
1. Large metal reinforced post in deep femoral box
- provides greater coronal plane stability
- variable varus/valgus stability as well as rotation
- permit 2-3o of varus-valgus movement
- 2o of internal/external rotation
2. Stems
- transmit the increased stresses away from the fixation interfaces to diaphysis
- otherwise increase risk of early loosening



Indications
- severe valgus deformity
- collateral ligament deficiency
- bone defects
- irreconcilable flexion-extension imbalance after PS implant
Disadvantage
- increased bone loss
- potentially higher rate of aseptic loosening
- fracture of the tibial stem
- recurrent instability
Types
Total Condylar III / TCIII (Depuy)
CCK / Condylar constraint knee
Legion (S&N)
Results
Lachiewicz et al J Arthroplasty 2006
- 10 year follow up of CCK in primary TKR
- severe valgus with incompetent MCL / severe FFD unable to be balanced
- only 2 / 54 revisions or 10 year survival 96%
- 86% good or excellent results
3. Constrained Hinged / Rotating Hinged
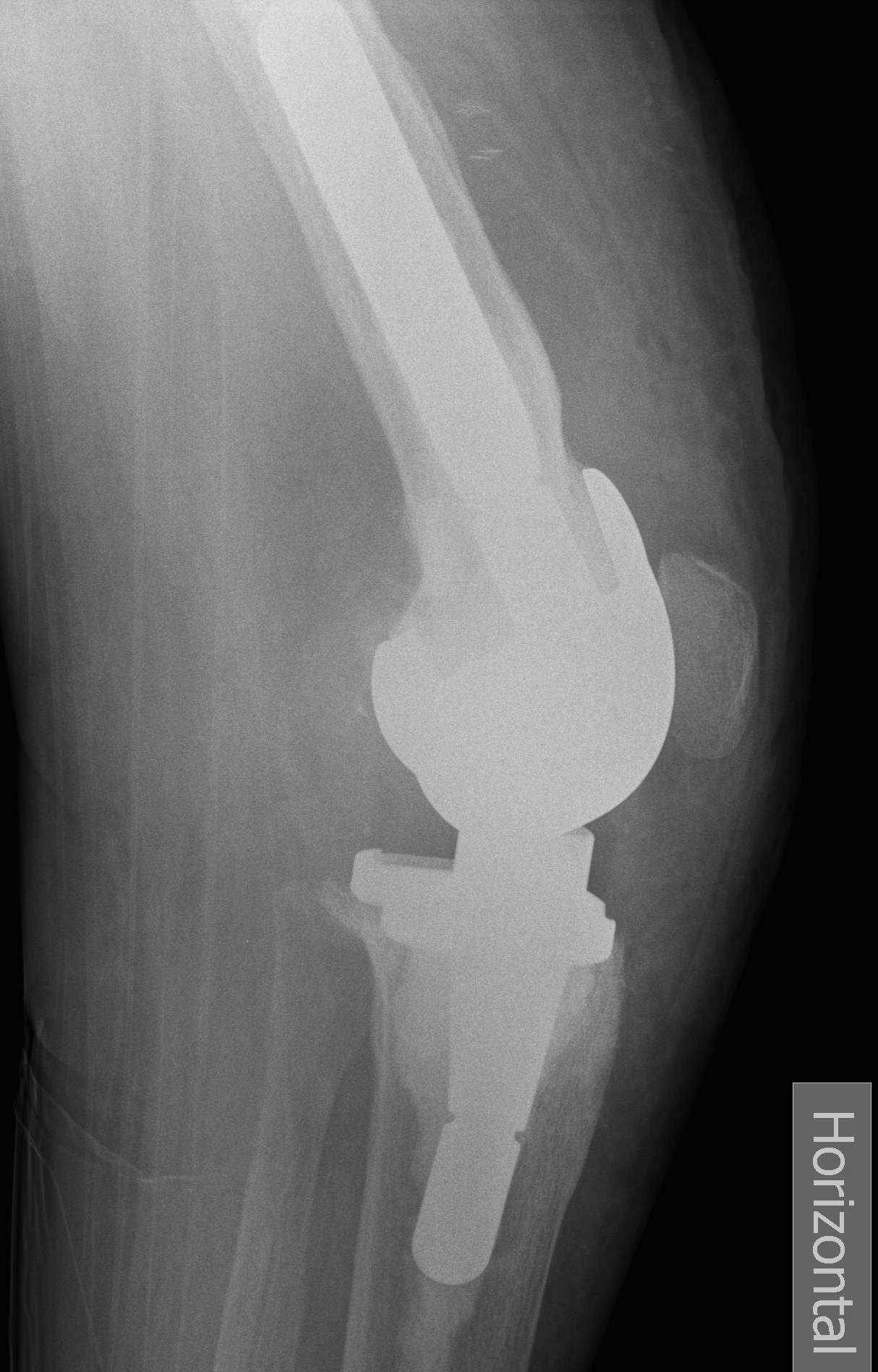
Design
1. Uniplanar hinge
- prohibited rotational motion
- high rate of aseptic loosening
- historical
2. Rotating Hinge
- linked with an axle
- restricts varus-valgus and translation
- permit rotation of the tibial bearing about a yoke on the tibial platform
- again need long stems to disperse forces
Disadvantage
- increased bone resection
- increased risk of aseptic loosening
- unusual breakages / dislocations / failures
Indications
- severe collateral instability
- severe bone loss
Results
Petrou et al JBJS Br 2004
- 100 rotating hinge prosthesis followed up for average 11 years
- average patient age 70
- good or excellent results in 91%
- 15 year survival 96%
- one supracondylar fracture / one dislocation / 2 deep infections
Constraint Algorithm
1. Severe varus > 15o, intact collaterals
Laskin Clin Orthop 1996
- improved pain scores and survivorship for PS over CR
- due to improved balancing and correction of deformity
2. Severe Valgus
PS if MCL intact
- VVC if MCL severely attenuated or ruptured +/- MCL reconstruction
- if very unstable in both flexion and extension, may need rotating hinge
- difficult to know exact indications for VVC v hinge
- judgement call (age, bone stock etc)
3. RA
- concern re late PCL instability and recurvatum
Hanyu J Arthoplasty 1997
- recommend PS
- however, be mindful that this group also has an increased rate of late dislocation over the tibial post
- 6.5% at 8 and 10 years post op
4. Patellectomy
- better functional and pain scores if use PS rather than CR
5. MCL attenuated (i.e. valgus knee)
A. Use PS and load the lax side
- mild to moderate
B. PS + MCL advancement / imbrication / reconstruction
- moderate to severely attenuated
- can make balancing difficult
C. VVC / rotating hinge
6. Intra-operative MCL injury
Either avulsed (femur) or cut mid-substance
- can use VVC but unlikely to have on hand
- use PS
- reattach / repair / augment MCL
- postoperatively hinge brace 6/52
Leopold JBJS Am 2001
- 16/16 patients no coronal plane instability with this treatment
