Definition
Patients usually complain of subluxation rather than dislocation
- rarely requires reduction
Different entity to acute posterior dislocation usually
Epidemiology
Rare
Aetiology
1. Ligamentous laxity > 50%
- commonly associated with MDI
- posterior only 20%
- posterior & inferior 20%
- posterior / inferior & anterior 60%
2. Trauma
A. Repetitive microtrauma
- common
B. Macro-trauma
- uncommon
- seizures
- electrocution
- ECT
- alcohol related injuries
- MVA
Pathogenesis
1. Capsulo- ligamentous
A. Reverse Bankart lesion
- uncommon
- detached posterior labrum < 10%
B. Capsular laxity
- much more common
C. Posterior IGHL avulsion
- reverse HAGL
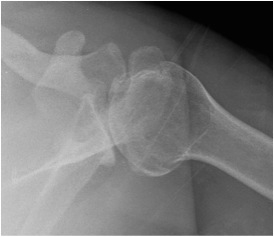
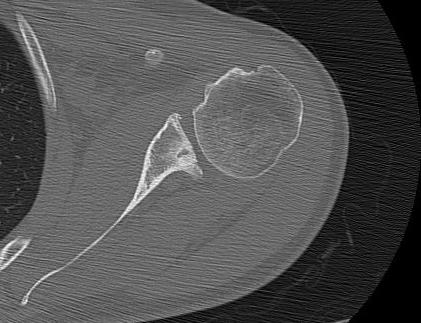
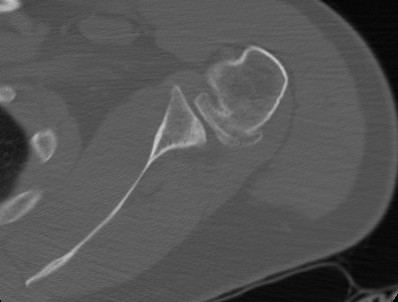
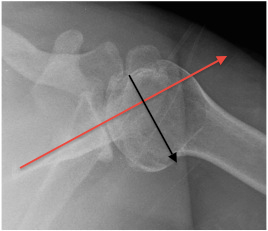
2. Bony
A. Humeral Head Defects
- reverse Hill-Sachs lesion
- defect in Ant humeral head
- seen in traumatic dislocations / chronic posterior dislocation
- can make humerus unstable
- compared with anterior Hill-Sachs which rarely does

B. Posterior glenoid deficiency
- seen in traumatic / chronic dislocations
C. Humeral head / glenoid retroversion
History
Must exclude voluntary dislocator
History of ligamentous laxity / other problems
Examination
Must assess for
- MDI / Ligamentous Laxity
- voluntary dislocator
Tender posterior joint line
- fairly specific for OA rather than instability
ROM
- loss of ER (in locked posterior dislocation)
Ligamentous laxity
Sulcus sign
- indicates MDI
Anterior apprehension
- indicates MDI
Posterior stress test
- supine
- adduct, forward flex and IR arm
- posterior force
- apprehension test
Load and Shift / Posterior Drawer
Altchek Grading
Grade 0 No translation
Grade 1+ Up to glenoid rim
Grade 2+ Beyond rim with spontaneous reduction
Grade 3+ Translation beyond rim without spontaneous reduction
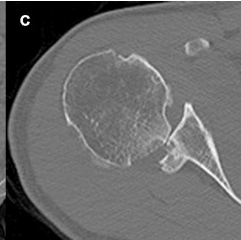
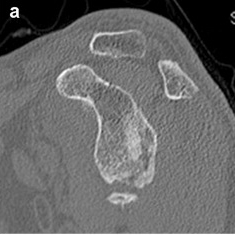
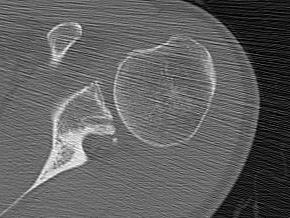
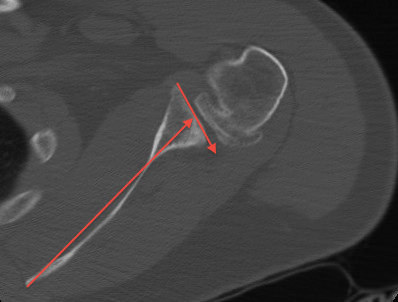
CT
1. Define extent of Hill Sach's lesion
2. Glenoid bone defect
3. Glenoid version
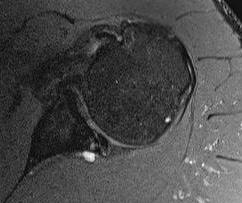
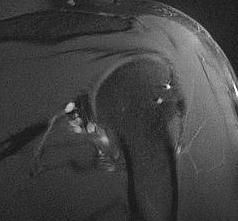
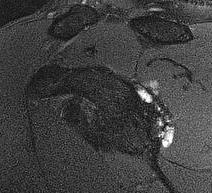
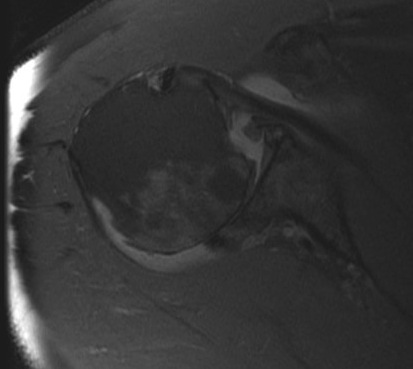
MRI
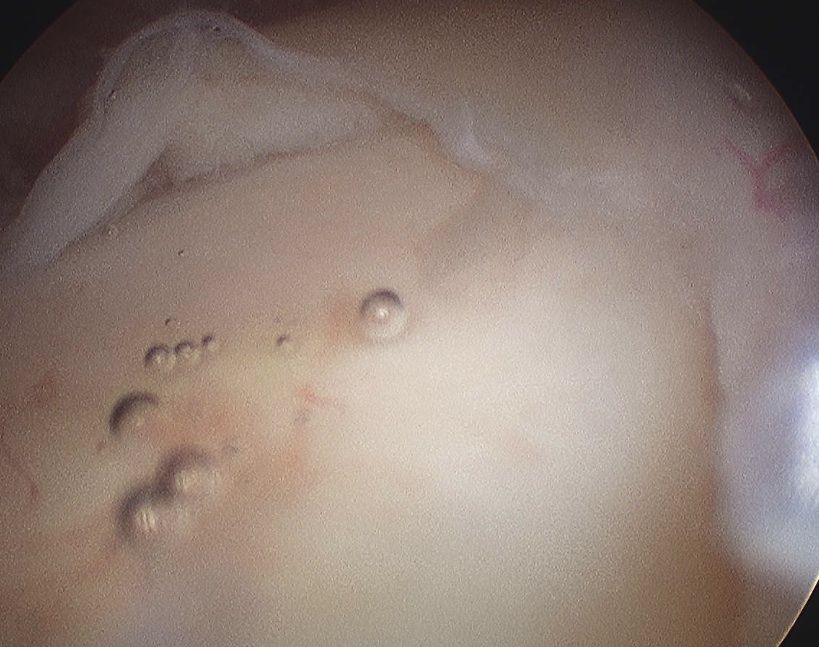
Posterior bankart lesion
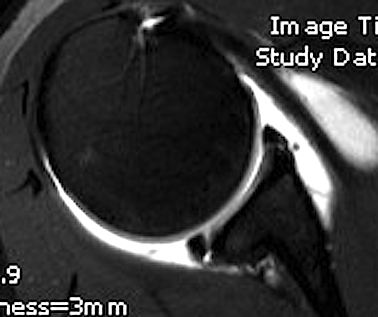
Posterior labral cysts
Management
Non-operative
Not infrequently little functional problems
Prolonged initial physical treatment for all patients
- minimum 12 months
- treat similar to MDI patients
- Matson & Rockwood 80-90% success rate
Operative
Indications
- failed non-operative management
- moderate to severe disability
Contra-Indications
- MDI
- voluntary dislocator
- ligamentous laxity
- minimal functional impairment
Pathology
1. Posterior Bankart lesion
Options
- arthroscopic / open reconstruction
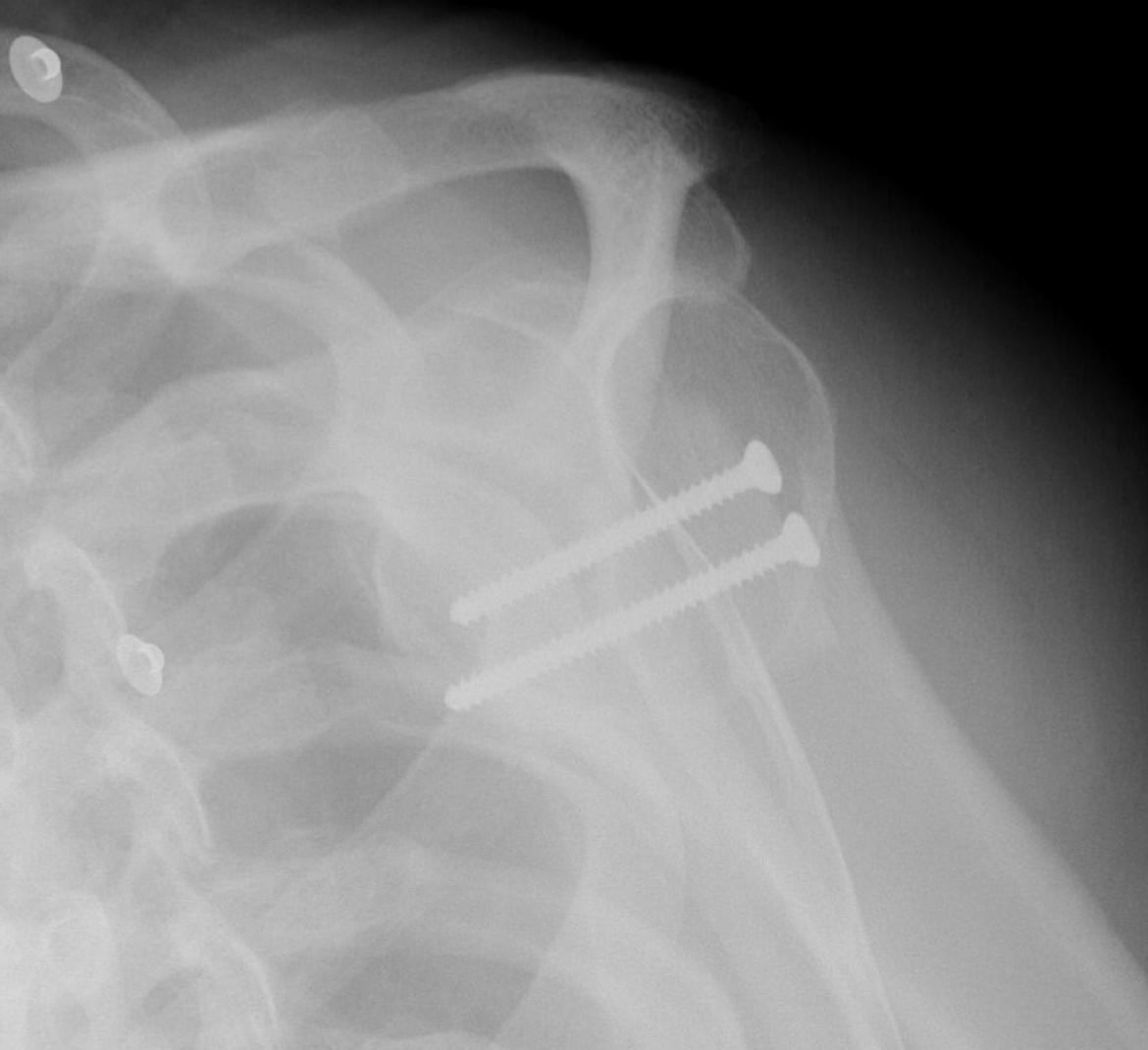
Failure / Bony Block Revison
- posterior approach
- detach infraspinatous
- expose capsule
- divide capsule medial to glenoid
- take 2 cm long x 1 cm thick iliac crest
- secure to glenoid with 2 x small fragment screws
- reattach capsule lateral to bony block


2. Capsular laxity
Options
- posterior capsular shift arthroscopic or open
- reverse Putti-Platt
Open capsular plication
Bigliani and Flatow July 1995
- 35 patients
- If primary operation 23 of 24 successful
- 89% stable at 5 yrs
Reverse Putti-Platt
Technique
- posterior approach
- posterior imbrication of IS & Tm
- combine with posterior capsule imbrication
- shorten tendon 1cm = 20°
- limit IR to 20o
3. Humeral Head Defect

1. HS < 25%
- leave
2. HS > 25%
- transfer SSC + LT (McLaughlin)
- OC allograft
3. HS > 40%
- hemiarthroplasty / TSR (older patient)
- OC allograft (younger patient)
4. Posterior Glenoid Defects
Option
- posterior glenoid bone graft


Results
Meuffels etal JBJS Br 2010
- 18 year follow up of 11 patients treated with posterior bone block
- 36% had had recurrent dislocation
- half would not have the surgery again
- all had evidence of OA
5. Retroverted Glenoid Version / Static Posterir Shoulder Subluxation
Issue
- posterior shoulder subluxation > 65%
- shoulder OA
- young age
- glenoid osteotomy
Option
- posterior opening wedge glenoid osteotomy
- rarely indicated & technically hard
Indication
- congenital retroversion of glenoid > 30o
Technique
- only 5 mm medial to glenoid rim otherwise injure SS nerve
- must prevent penetration of glenoid
Complications
- anterior impingement of subscapularis on coracoid causing pain
- anterior subluxation of humeral head
