Issues
Rule out infection
Assess rotator cuff
Assess bone stock
- can you re-implant glenoid
- do you need bone graft
Removal of prosthesis
- glenoid typically simple
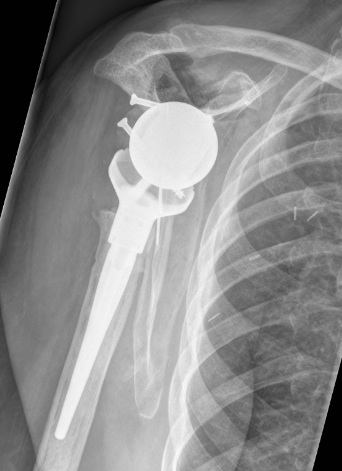
Revise to
- aTSA
- rTSA
- hemiarthroplasty
Outcomes
Ravi et al. Bone Joint Open 2021
- systematic review of 5379 revision aTSA
- multiple indications including loosening (20%), instability (19%), rotator cuff failure (17%) and infection (16%)
- 22% complication rate
- 8% reoperation rate
- revision to rTSA rather than aTSA resulted in fewer complications, better Constant score, but not ASES scores
- revision aTSA to rTSA in 75 patients
- multiple indications for surgery
- major complications in 28% and reoperation in 12%
- improvements in patient reported outcome measures but did not reach that of primary aTSA
- revision of 110 failed hemiarthroplasties and aTSA to rTSA
- 92% 2 year survival
- 74% 5 year survival
Investigations
Rule out infection
- CRP / ESR
- ultrasound or xray guided aspiration
- arthroscopy for fluid and tissue sampling
Ultrasound
- good for cuff integrity
- MRI often not useful due to large amount of metal artefact
CT scan
- glenoid bone stock
Approach
Verhoste et al. Int Orthop 2020
- clavicular osteotomy in revision TSA
- curved longitudinal osteotomy parallel to deltoid insertion, sutured back on at end of case
- improves exposure and preserves deltoid
- 40 patients, with 95% healed by 3 months
- 3 post op clavicle fractures after a fall, one loosening
- 3 surgical revisions required
Implant Removal
Glenoid
- often very loose
- easy to remove

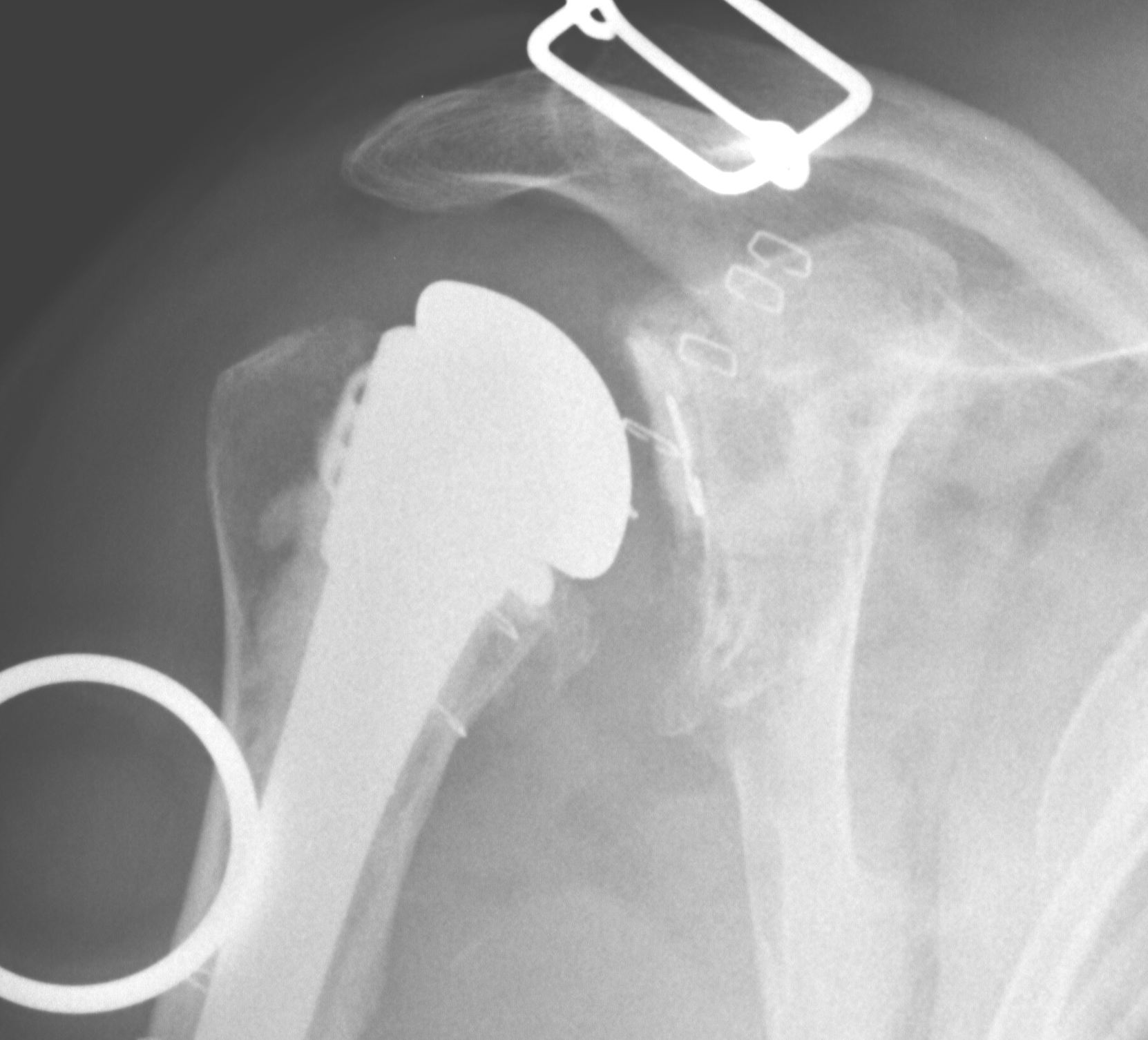
Humeral component
- most uncemented stems only proximally coated
- flexible osteotomes

Glenoid bone stock restoration
1. Cortical ring allograft
- napkin ring type
- take from calcar of a femoral neck
- cut so is thicker posteriorly to reconstitute the glenoid
- place onto freshened glenoid surface
2. Bulk posterior allograft
Technique
- use femoral head
- reconstitute posterior aspect of glenoid
- fix with 2 x cannulated 4mm screws via stab incisions posteriorly
- need to be able to fix glenoid component with screws still
Revision Humeral Component
Technique
- often need long stem
- often use cement in revision circumstance
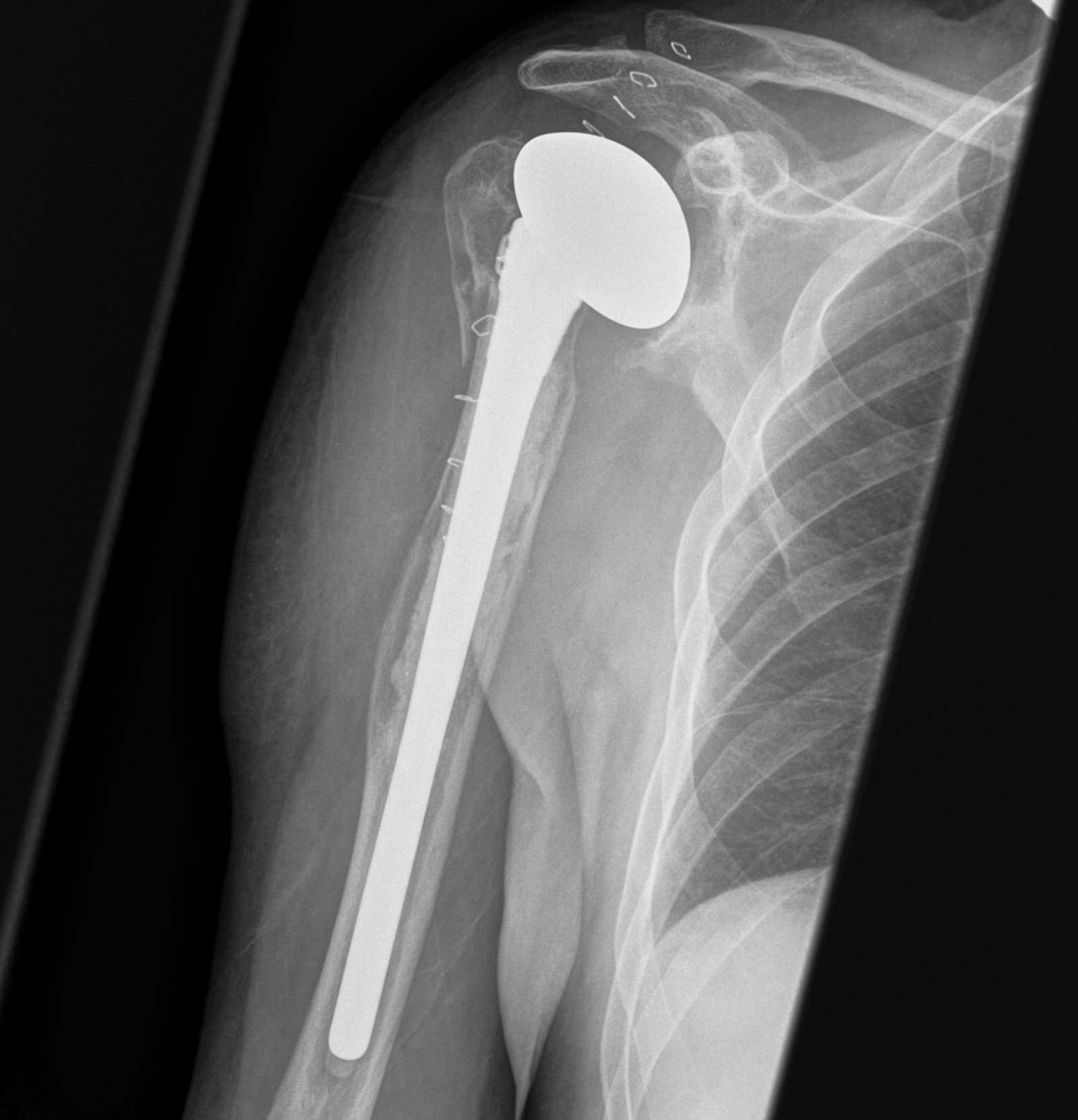
May need proximal humerus allograft

Sanchez - Sotelo et al. JBJS Am 2017
- 26 patients undergoing revision to reverse with bulk proximal allograft
- average time to union 7 months
- one patient required bone grafting to obtain union
