Definition
Reduction of space available for neural elements
- in spinal canal or intervertebral foramina
- due to degenerative changes, congenital abnormalities or both
- involves compression of the thecal sac or nerve roots
Epidemiology
Onset 50 - 60's
- M = F
- associated with onset OA spine
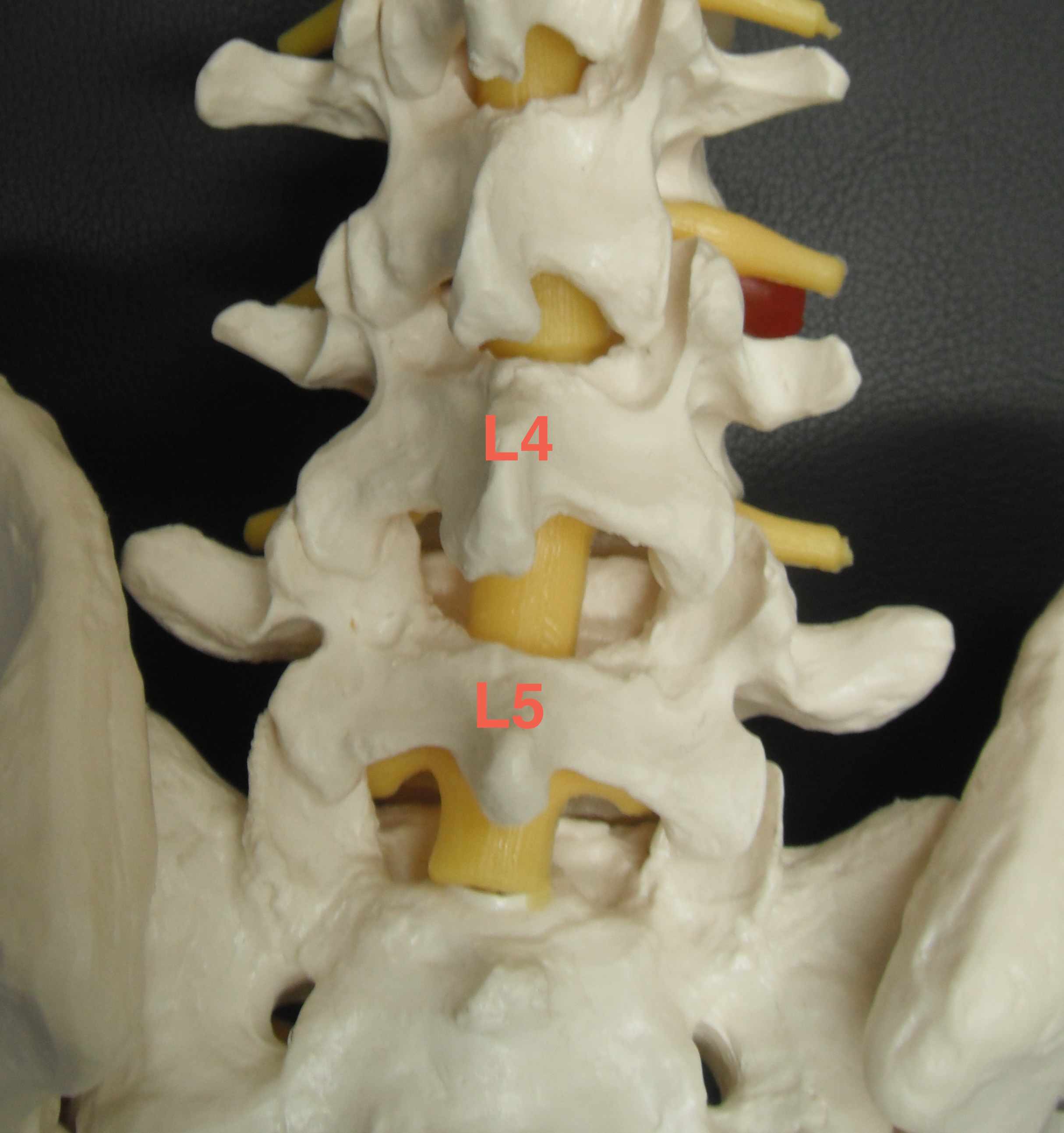
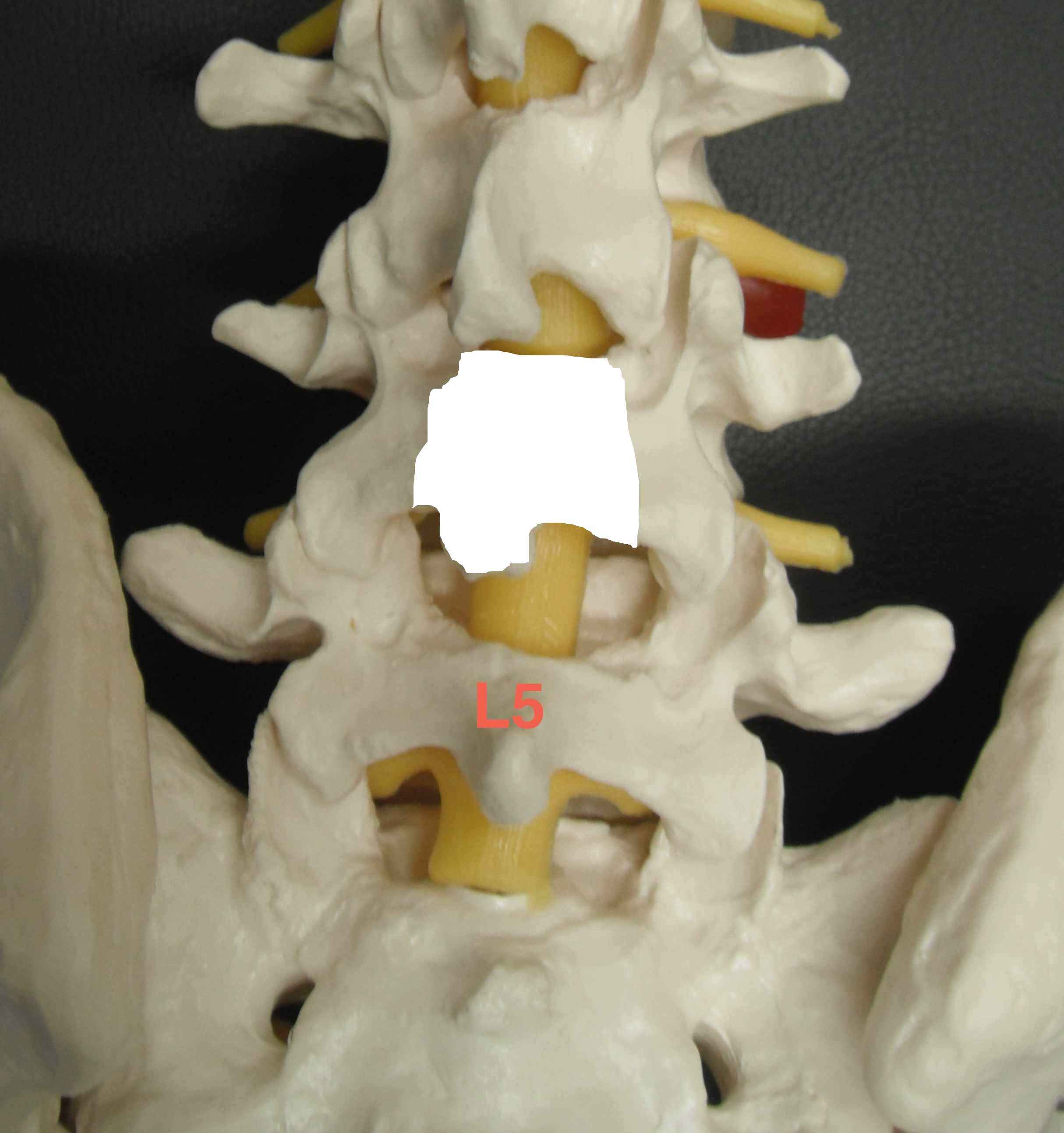
L3/4 & L4/5 most common
Aetiological Classification
1. Congenital
Achondroplastic
- short thick pedicles and narrowed interpedicular distance
SED
Idiopathic ~ Polynesians
- trefoil-shaped canal
Congenital narrow spinal canal
- most syptomatic patients have canals at lower end of spectrum
Prematurity
- narrow L3
Ostepetrosis
2. Acquired
Degenerative
- most common aetiology
- disc desiccation / loss of height / bulging of annulus
- facet subluxation / capsular hypertrophy / osteophytes
- overall shortening of lumbar spine / decreased volume
- ligamentum flavum hypertrophy
Spondylolisthesis
Kyphosis
Iatrogenic
- post-laminectomy
- post-fusion
Miscellaneous
- Paget's disease
- Fluorosis
- DISH
- Ankylsing spondylitis
- Tumour
- Infection - TB
Traumatic / Post fracture
Anatomical Classification
1. Central Canal Stenosis
2. Lateral Recess Stenosis
3. Foraminal
Anatomy
1. Central canal
Posterior wall - ligamentum flavum & laminae
Lateral wall - medial facet joints & intervertebral foramina
Anterior wall - annulus fibrosis & posterior vertebral body
2. Lateral recess
Extends from where nerve root leaves dural sac to where nerve root enters foramen
Posterior wall - ligamentum flavum & superior part of lamina
Anterior wall - posterior vertebral body & annulus fibrosis
Lateral wall - medial & inferior pedicle
3. Intervertebral foramen
Extends from inner to outer foramen
Superior wall - inferior part of pedicle above
Inferior wall - superior part of pedicle below
Anterior wall - above is body, below is disc
Posterior wall - pars interarticularis, ligamentum flavum & apex of superior facet of vertebrae below
Pathology
Stenosis typically at disc level either due to disc or facets
1. Central Canal
- bulging of annulus posterior
- facet osteophytes posterolateral
- hypertrophied ligamentum flavum posterolateral
2. Lateral Recess
- facet subluxation & osteophytes + hypertrophied ligamentum flavum
3. Intervertebral Foramen
- loss of disc height with approximation of pedicles
- inferior annular bulge
- medial facet hypertrophy
Effects
Mechanical
- increased canal narrowing with extension
- also get posterior disc protrusion and redundancy of ligamentum flavum
- root lacks perineurium & hence more susceptible to compression
Ischaemia
- interference with metabolic demands of nerve root
- exercise increased nutritional requirements & waste production
- canal constriction limits response = relative ischaemia
Symptoms
Back Pain
Sciatica
- L5 most common, then S1
Neuropathic claudication
- insidious onset
- usually bilateral
- diffuse / no dermatomal pattern
- buttocks / thighs / calves
- heaviness / weakness / burning / cramping / tingling / numbness
Worse with walking, standing & lumbar extension
Relieved by sitting, flexion, walking upstairs, squatting
Signs
Often none, but can overlap with HNP
DDx
Vascular claudication
- calf pain with exercise
- rapid relief with cessation walking
- no back pain / no numbness
- abnormal pulses
Hip Disease
Diabetic neuropathy
Retroperitoneal pathology
X-ray
Rule out
- infection / tumour / fracture
Confirm degenerative changes
- facet hypertrophy / disc narrowing
- decreased AP diameter of canal
- identify associated pathology i.e. spondylolisthesis / scoliosis
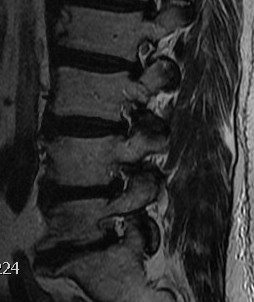
MRI
T2 Sagittal "MRI Myelogram"



Stenotic Measurement
A. Volume
- more accurate
- critical area is 100 mm2
B. AP diameter less accurate
- normal if > 12mm
- absolute stenosis if < 10mm
Intervertebral foramina
- no fat about nerve root
- reduced height

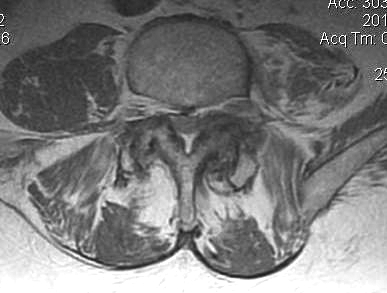
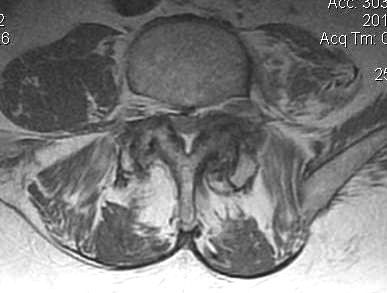
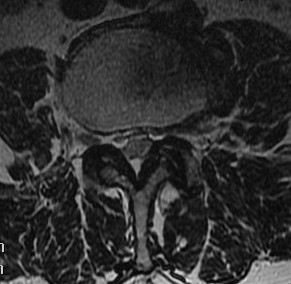
B. Axial slices
Findings
- no fat about dura
- trefoil shape canal
- lateral recess or foramina compression
- nerve root compression

NHx
Not clear not all patients progress
Johnsson 1993 Clin Orthop
- 32 patients followed 4 years
- 70% unchanged
- remainder: half worse, half better
Management
Non-Operative Management
Options
Rest / Avoid aggravating activities
Analgesics
- simple analgesia
- short course NSAIDS
Back support
- prevent extension
Physio
- back strength in flexion
- stabilise abdominal muscles
- aerobic fitness on exercise bike
Epidural steroids
Koc et al Spine 2009
- RCT of exercise v epidural steroids v control in spinal stenosis
- exercise and epidural steroids both effective up to 6 months
Calcitonin
Podichetty et al Spine 2004
- RCT of calcitonin v placebo
- no difference in two treatment groups
Operative Management
Indications
Absolute
Cauda equina syndrome
Relative
Failure to respond to non operative treatment
Disabling neurogenic claudication
Progressive neurological deficit
Back pain is not an indication
Options
Decompression +/- fusion
Interspinous devices
- limit extension
Indications for fusion
1. Degenerative Spondylolisthesis
2. Radiological instability
- > 3mm or > 11o
3. Intra-operative destabilisation
- removal of > 1 facet joint or pars
- i.e. radical decompression required laterally
4. Degenerative scoliosis
5. Significant low back pain / disc degeneration
Decompression
Define site of compression
- central / lateral recess / foramina
Define levels
- single / multilevel
Fusion
- must be prepared to fuse if cause instability
- consent
Results
Operative v Non Operative
Weinstein et al Spine 2010
- SPORT trial
- RCT of operative v non operative treatment lumbar stenosis
- 289 patients with 4 year follow up
- substantially improved pain and function in operative group
Interspinous Devices
Hsu et al J Neurosurg Spine 2006
- RCT of non operative v X Stop interspinous device
- significant improvement in QOL, with results similar to surgical decompression
Decompression v Fusion
Niggemeyer et al Eur Spine J 1997
- meta-analysis
- if symptoms < 8 years, decompression without fusion yields best results
- if symptoms 15 years or more, decompression with instrumented fusion best results
- decompression and fusion without instrumentation had worst results
Complications
Epidural haematoma
Instability
Infection
Nerve root injury
Dural Tears
Technique L4/5 Decompression
Position
- abdomen free to limit venous pressure and bleeding
- 4 poster / knee below hips / arms on bolster
- feet / knees / elbows / face / eyes cushioned
- SCUDS, TEDS
- betadine packs in buttocks
- +/- Jackson table (enables more lordotic position if instrumentation planned)
Landmarks / Check level
- iliac crest L4/5 interspinous space
- prep area aseptically, spinal needle
- check with lateral x-ray
- square drape
Incision
- inject LA with A
- midline
- meticulous haemostasis
- divide thoracolumbar fascia
Superficial Dissection
- subperiosteal elevate of supraspinous muscles (Cobb's and diathermy)
- sequentially pack with rolled swabs / sausages to control bleeding
- out to lateral extent of pars
- expose facet joints, but preserve capsule if not fusing
- beware parafacetal arteries
- don't extend between transverse processes as nerve root at risk
Deep dissection (L4/5)
Recheck level
- L4/5 interspinous gap
Resect L4 spinous process
- remove ligamentum flavum above and below
- Kerrison Rongeur / knife
- remove all of L4 lamina
- expose L4/5 disc space
- L5 nerve root exits inferior
- L5 nerve root will pass below L5 pedicle
Remove L4/5 disc fragments if needed
- nerve root retractor
- gently retract dura to each side
- take out with pituitary rongeur
L4/5 medial facetectomy
- above L5 pedicle
- L5 nerve root exits inferior to it
- decompress, pass Watson Chaney
Preserve pars & half of facet
- may have to remove entire facet joint & pars
- preserve one facet joint at each level
- can be 1/2 on each side
