Definition
Diffuse Idiopathic Skeletal Hyperostosis
- non-inflammatory disease
- ossifying enthesopathy / bone forming diasthesis
- most commonly involves spine / anterior longitudinal ligament
AKA Forestier's disease
DDx
Ankylosing Spondylosis
DISH
- non inflammatory
- no facet or SIJ involvement
- no squaring of anterior vertebral body
- non marginal syndesmophytes
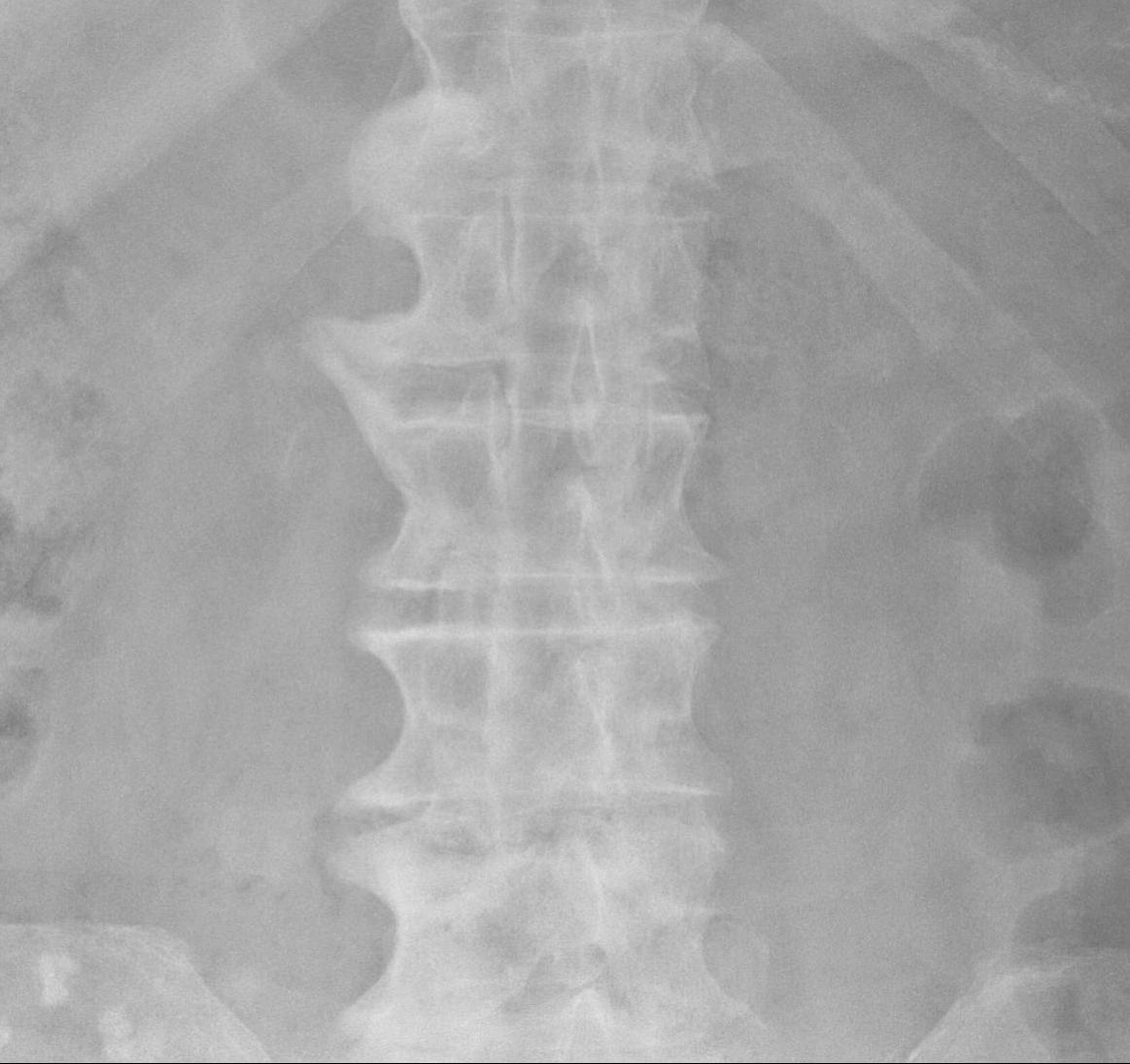
Diagnostic Criteria for DISH
1. Flowing ossification along the anterolateral aspect of at least 4 contiguous vertebrae
2. Preservation of disc height / relative absence of significant degenerative changes
3. Absence of facet joint ankylosis or sacroiliac erosion


Epidemiology
Common
- 1/3 over age 65
Middle-aged or elderly
Associations
Diabetes
Hypertension
Gout
Obesity
Normal incidence of HLA B27
Clinical Presentation
Principal symptom is LBP
Occasional dysphagia
- anterior osteophytes in cervical spine impinging on oesophagus
Occasional spinal stenosis
- due to ossification of PLL
Achilles tendonitis
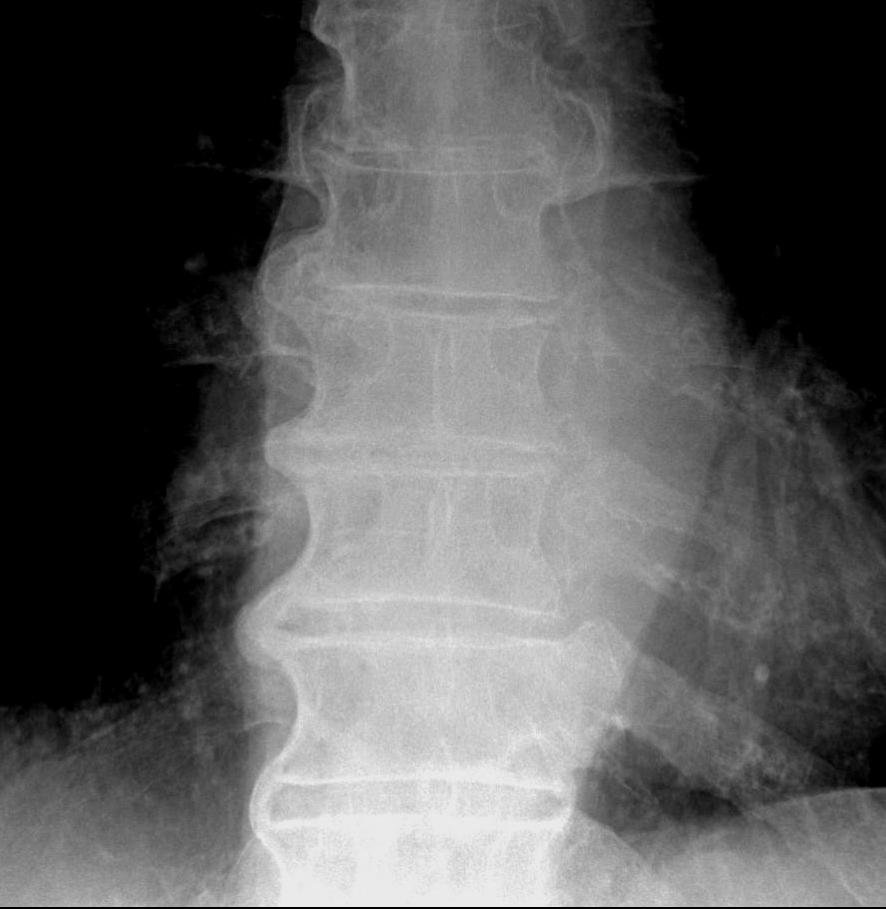
X-ray
Thoracic vertebra
Most common right sided and unilateral
- anterior & lateral spine
Non marginal syndesmophytes
- flowing / candle wax
- marginal osteophytes of ankylosing spondylitis very vertical
Integrity of disc spaces & facet joints maintained
- not an arthritis
Cervical spine
- less frequent


Lumbar spine
- least common



Other
Pelvis
- osseous whiskering at sites of ligament attachment
- iliac crests / ischial tuberosity / trochanters


Heel
- calcaneal spurs / achilles tendonitis
Hip
- periarticular bone formation with intact joint space
- increased risk of HO in THR
Shoulder
- hyperostosis deltoid insertion, LT, GT
Elbow
- olecranon spurs
Management
Non operative
Analgesia
NSAID
Physiotherapy to maintain motion
Operative
Surgery rarely required to remove osteophytes
- sometimes in cervical spine to relieve symptoms
Trauma
- high risk of fracture
- need to be carefully assessed
- high risk of neurology and instability
