Conditions
1. PIPJ Synovitis
- synovectomy via dorsomedial approach
2. Flexor tenosynovitis
- may cause trigger finger
- trial HCLA
- remove synovits but don't release A1 pulley
- will worsen ulna drift
3. DIPJ
- rarely affects
- may get mallet
- arthrodesis
4. Ankylosis
- arthrodesis / arthroplasty
5. Unstable / flail
- arthrodesis usually best option
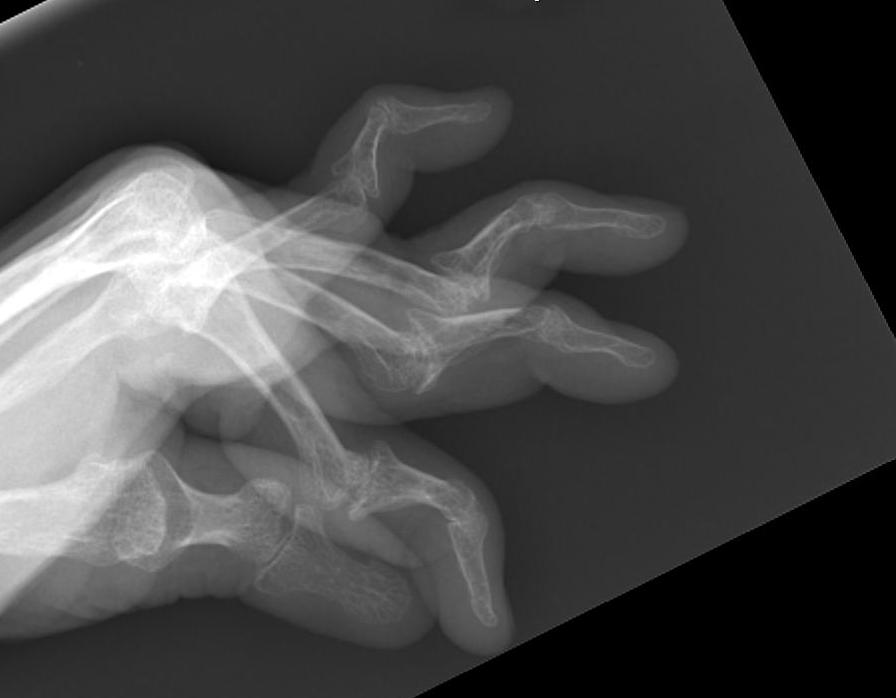
6. Swan neck deformity
7. Boutonnière deformity
Concepts
Boutonnière deformity
- usually good function
- often don't need surgical treatment

Swan Neck
- much more debilitating
- usually need treatment
Swan Neck Deformity (Intrinsic Plus Deformity)
Deformity
Hyperextended PIPJ / MCPJ + DIPJ flexion
- Bunnell calls this "Intrinsic plus deformity"



Cause
Primary process is usually synovitis
- starts at either MCPJ / PIPJ / DIPJ
DIPJ
Dorsum
- terminal tendon ruptured or attenuated
Volar
- may also be due to stuck FDP
PIPJ
Volar
- rupture of FDS due to synovitis
- volar capsule stretches due to synovitis
Dorsum
- contracted central extensor slip
MCPJ
Extrinsic
- relative shortening of long extensors
Intrinsic
- relative intrinsic tightness
- also seen in CP / CVA
Articular
- destruction or deformity

Nalebuff Classification
Function depends upon PIPJ flexion
Bunnell Test
Assess Interossei Tightness
Positive test
- PIPJ flexion less in MCPJ extension than with MCPJ flexion
- interossei are tighter in extension
- invalidated by MCPJ dislocation
Test
- hand dorsum up
- correct ulna deviation
- extend MCPJ & comment on active PIPJ range
- flex MCPJ & comment on active PIPJ range
Type I
- PIPJ passively correctable / regardless of MCPJ position
- Bunnell Test negative
Type II
- PIPJ flexion limited with extension of MCPJ
- Bunnell Test positive
- intrinsic tightness
Type III
- fixed PIPJ flexion regardless of MCPJ position
- joint problem
- lateral bands dislocated dorsal to axis of rotation
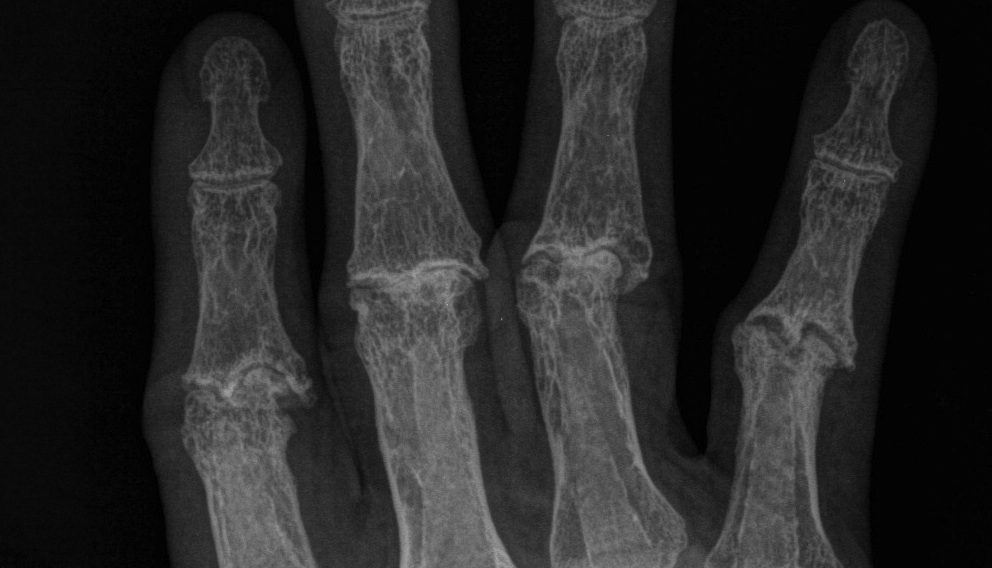
Type IV
- joint destruction / X-ray arthritis

Management
Aim is to create FFD
- many techniques described
Type 1
A. Create FFD by FDS tenodesis
- use slip of FDS
- detach proximally
- pass through A2 pulley and attach to bone or on itself
- producing 20° FFD
+ DIPJ fusion
B. Zancoli lateral band transfer
Lateral bands mobilised volar to axis of PIPJ
- raise flap of flexor retinaculum
- suture over lateral band to fix in place
- dorsal blocking splint / K wire
+ DIPJ fusion
Type II
Above +
Intrinsic release
- division of intrinsic oblique fibres
Anatomy
- oblique fibres which extend IPJ / interossei
- transverse fibres flex the IPJ / lumbricals
Type III
PIPJ release first / Lateral band tenolysis / K wire
- release central slip / dorsal capsule / collateral ligs to allow flexion to >90o
- manipulate joint to flexed position
- fix with K-wire
- often stiff due to flexor synovitis
- often need flexor sheath synovectomy to get moving
Type IV
Arthroplasty RF / LF for grasp
- arthroplasty has highest failure rate for Swan Neck
- high recurrence and poor range
- 80% survival at 9 years
Fusion IF / MF for strength
- angle of fusion a cascade
- 20 30 40 50 (IF MF RF LF)

Boutonniere's Deformity (Intrinsic Minus Deformity)
Deformity
PIPJ flexed / DIPJ hyperextended / MCPJ hyperextended
Often well tolerated & treatment not needed
Cause
1. Central slip dysfunction
- always starts with PIPJ flexion
2. Lateral bands displace volar
- secondary to triangular ligament stretching
3. DIPJ hyperextends secondary to PIPJ flexion
- contracted oblique retinacular ligament
- becomes fixed
- examination finds limited DIPJ flexion with PIPJ in extended position
Nalebuff Classfication
Stage 1
- mild extensor lag 10-15°
- passively correctable
Lateral band reconstruction
- reduce lateral bands dorsally
- suture together
Stage 2
- moderate 30-40° lag
- passively correctable
Lateral band reconstruction + Central slip shortening / reconstruction
Dorso-Medial Incision & Synovectomy
A. Reduce lateral bands dorsally & Suture together
B. Tenotomy Terminal slip
C. Central slip options
i) Shorten 5 mm
ii) Reconstruct with lateral bands (take inside half of each and suture together)
iii) Reconstruct with PL
iv) Matev central slip reconstruction
Matev Central Slip Reconstruction
- radial lateral band divided at level of P2
- proximal stump rerouted through central slip
- attached to base P2 at central slip insertion
- ulnar lateral band divided distally
- passed dorsally over P2 and attached to distal radial lateral band stump
Stage 3
- severe
- fixed with x-ray arthritic changes
Arthrodesis / arthroplasty
PIPJ replacement
Types
A. Pyrocarbon implants
- partially constrained press fit components
- relatively high failure rate
- can fracture when inserting and need cerclage wire
B. Swanson spacer
Contra-Indications
Infection
Non reconstructable / irreparable
- extensor and flexor tendons
- collateral ligaments
Complications
Does not have same stability of MCPJ
- can dislocate
Technique
Dorsal incision
- straight or curved dorsomedially
- enter between central slip and lateral band
- can detach central slip proximally and reflect distally
Release contractures
- balance soft tissues
- retain collaterals
Broach distally and proximally
- avoid extension at all times
Implant must achieve full extension
- no buckling, and no impingement
Repair central slip
Post op
- immobilise for 1 week
- dynamic extension splint 0 - 30o (Capner)
- active flexion
Arthrodesis PIPJ
Approach as above
- resect collaterals
- position as appropriate
- cross K wires / screw
