Operative versus Nonoperative Management
Issues
Knee function
Return to sport
Meniscal injury
Osteoarthritis
Knee function
Reijman et al BMJ 2021
- RCT of 160 patients
- randomized to early ACLR v rehabilitation and optional delayed reconstruction
- 50% in rehabilitation group underwent delayed reconstruction
- significantly better IKDC scores in early ACLR group at 2 years (85 v 80) but perhaps not clinical significant
https://pubmed.ncbi.nlm.nih.gov/33687926/
Frobell et al BMJ 2013
- RCT of 120 patients
- early ACL reconstruction or functional rehab with option of delayed reconstruction
- 1/3 of patients in ACL rehab group chose to have ACL reconstructed
- at five year follow up, no difference in early ACLR / delayed ACLR / rehabiliation alone
https://pubmed.ncbi.nlm.nih.gov/23349407/
Return to sport
Randsborg et al Am J Sports Med 2022
- 1000 patients 7 years post surgery
- 70% return to sport
https://pubmed.ncbi.nlm.nih.gov/35040694/
Meniscal Injury
Sanders et al Am J Sports Med 2016
- database study of 1000 patients with ACL tear
- matched to cohort of 1000 patients without ACL tear
- early ACLR v delayed ACLR v nonoperative
- at 13 years follow up, patients treated nonoperatively had a higher risk of meniscal injury, OA and TKR
https://pubmed.ncbi.nlm.nih.gov/26957217/
Osteoarthritis
Daniels Am J Sports Med 1994
- higher OA in reconstructed knee v non operative
- even if remove those knees that had meniscal surgery
Operative Management
Indications
1. Continued instability not responsive to physiotherapy and strengthening
2. Reparable bucket handle meniscus tear
Repairing in the setting of ACL deficiency has a lower success
3. Adolescent
4. Reinjury with meniscal or cartilage damage
Patient is demonstrating instability
5. Wish to return to pivoting sports
Clinical scenarios
1. ACL tear + Meniscus tear
Displaced bucket handle meniscus and acute locked knee
Acute meniscus repair + delayed ACLR
- reduced rate of meniscus healing
- an unstable knee may retear the meniscus
Acute ACLR and meniscal repair
- advantage is single surgery / high rate meniscus healing
- problem is risk arthrofibrosis
Results
Majeed et al J Orthop Traumatol 2015
- level IV study of 83 patients with ACL injury and meniscal repair
- meniscal repair failure in 14.5% of patients undergoing early ACLR
- meniscal repair failure in 27% of patients undergoing delayed ACLR
https://pubmed.ncbi.nlm.nih.gov/25701256/
Korpershoek et al Orthop J Sports Med 2020
- systematic review
- level 3 evidence that ACLR in the ACL deficient knee protects the repair
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7388123/pdf/10.1177_2325967120933895.pdf
2. ACL + Medial Collateral
Epidemiology
Grade II MCL
- 75% chance ACL rupture
Non-operative
Rehab MCL
- perform delayed reconstruction of ACL if symptomatic instability
ROM knee brace to limit extension
- 2 weeks 30-60°
- 2-4 weeks 30-90°
- 4-5 weeks 15˚ - 90
- 6th week 0 – 90˚
Indication for surgery
- MCL torn off tibia (usually off femur) and flipped up and over the pes anserinus
- won't heal in this position
- MRI all patients with MCL tenderness over tibal insertion
Patient with MCL and ACL instability
- reconstruct ACL
- reassess MCL at end of case
- if mildly unstable, advance / imbricate MCL on femoral side +/- tighten medial head gastrocnemius
- if severely unstable, reconstruct with hamstring or tendoachilles allograft

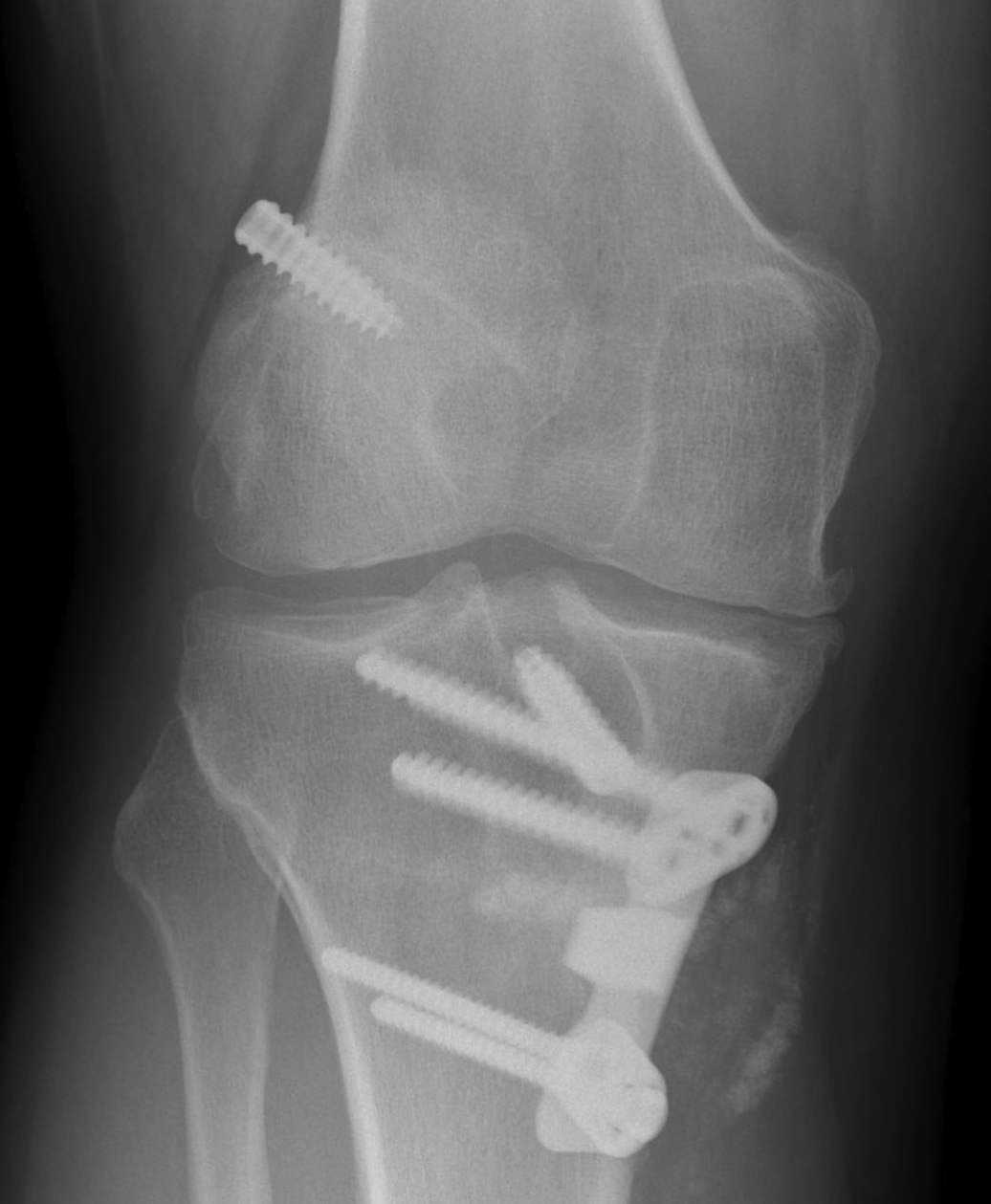
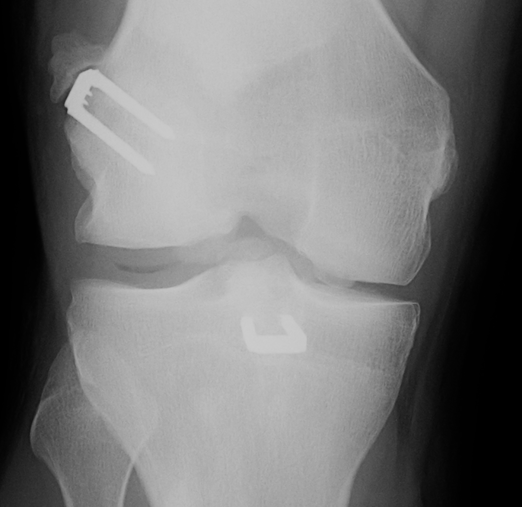
4. ACL + large medial chondral lesion
Consider HTO + ACL

Surgical Options
1. Primary Repair
High failure rate
Reason
1. No clot formation 2° synovial fluid
2. Tension on ligament
3. Intrinsically poor healing potential
2. Extra-Articular Augmentation
Lateral extra-articular procedures
- prevent anterior subluxation LFC in extension
- unpopular due to poor long term results
1. Ellison Procedure
A. Strip of ITB Deep to LCL
- placing it anterior in a bone trough
B. Plication the capsular ligament
2. MacIntosh Procedure
ITB left attached distally
- deep to LCL
- subperiosteal tunnel in LFC
- thru intermuscular septum
- back on itself distally


3. ACL Reconstuction
Graft Incorporation
1. Central necrosis
- 6 weeks post op
- strength of the graft if 70% of original at this time
2. Synovialisation
- up to 6 months post op


3. Revascularisation
4. Ligamentisation
- 6 to 18 months
- longitudinal orientation of collagen
- normal tendon at 2 years
Theory
- acts as scaffold for fibroblasts
- graft undergoes ischaemic necrosis & then becomes enveloped with vascular synovial tissue
- occurs at 4-6 weeks post-op
- neovascularisation & cellular proliferation 3/12
