Definition
Idiopathic condition of the immature femoral capital epiphysis involving varying degrees of osteonecrosis
AKA
- Legg-Calve-Perthes disease
- coxa plana
Described in separate publications in 1912 by
- Legg (Boston)
- Calve (France)
- Perthes (Germany)
Epidemiology
M: F 4:1
1 in 740 males
Onset usually at age 4-8
- early as 2 to late as 12
Children small and thin & hyperactive with delayed bone age
Bilateral - between 8 - 24%
- will not be symmetric
- if symmetric think other causes
Risk Factors
Sex : M: F 4:1
Geographic Location - 1/1200 US; 1/12 000 UK ; More common in urban areas
Social Class - Higher incidence in lower socio-economic classes
Race - Caucasian > Asian > African (extremely rare)
Perinatal Factors - Maternal Smoking ; Breech ; Prematurity/ Low Birth Weight ; Older Parental Age
Aetiology
Uncertain
Multiple ischemic events causing AVN
- ? lateral epiphyseal blood vessel occlusion
- sole blood supply 4-8 years
Theories
1. Microtrauma to retinacular vessels
2. Increased synovial pressure
- e.g. transient synovitis
3. Venous HTN 2o to thrombotic occlusion
- hyperthrombotic state
- hypofibrinolysis
Glueck 1996 JBJS
- 75% coagulation abnormality
- decreased Protein C ± S / increased lipoprotein A
- this has never been a found association in any study since
Blood supply immature femoral head
Medial and lateral circumflex femoral
- cruciate and trochanteric anastomoses
- extracapsular ring at base of neck
- retinacular vessels run in capsule
- intracapsular ring at base of head
- lateral epiphyseal artery most important
Ligamentum teres
- artery viable up to age 2
Associations
Short stature & delayed maturation
Attention Deficit Hyperactivity Disorder / ADHD
Trauma
- parents often relate onset of symptoms to traumatic event
- this association not clearly established
Irritable hip ~ 1%
Pathology
Head
Various areas of necrosis / revascularisation
- reossification from periphery
- typically anterior & lateral
Ossified epiphysis small
- stops growing
- cartilage keep growing with blood from synovium
- increased head to teardrop appearance but head does not subluxe
Head deformity secondary to collapse
- biological plasticity during creeping substitution
- head subjected to uneven & excess forces
- flattening or saddle deformity
- anterolateral extrusion of cartilage
Coxa Magna
- flattening of head with lateral extrusion of physis + periosteal new bone
Physis
Avascular
- growth arrest
- disordered cartilage columns in physis
Coxa Breva
- physeal arrest with short neck & long GT
- LLD & Trendelenberg gait
Classification
Chronological
- Waldenstrom
Extent of femoral head involvement
- Catteral
- Salter-Thompson
- Herring
End-result
- Mose
- Stuhlberg
Waldenstrom Stages
History : Swedish Surgeon ; Described disease 1910 prior to being named by Legg-Calve-Perthe in 1912
1. Initial
Duration : 3- 6 months
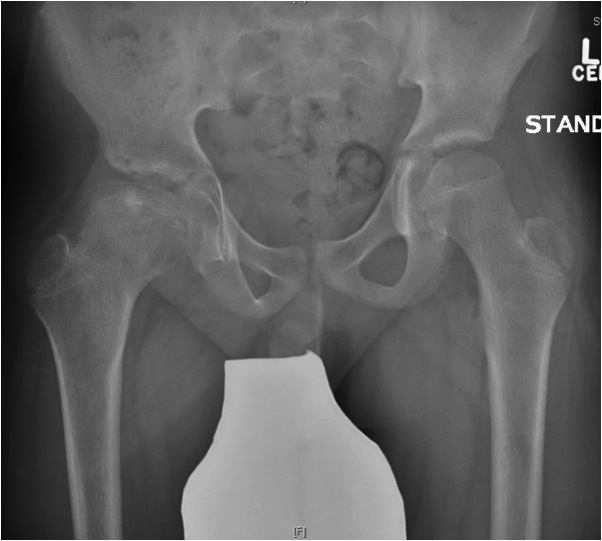
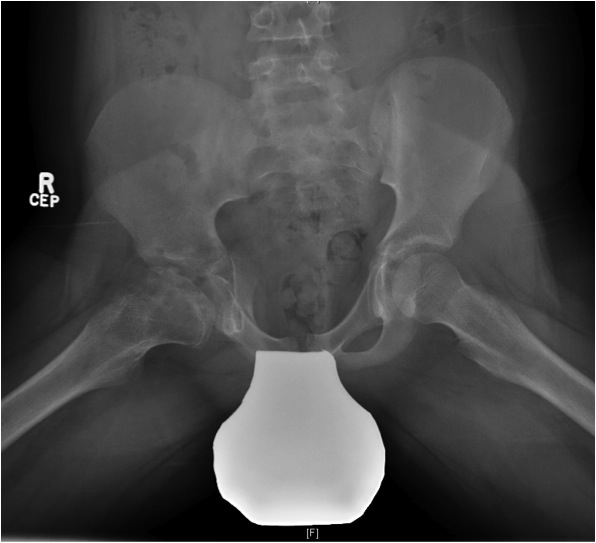
Xray
- may be normal
- small, sclerotic epiphysis
- joint space widening
- increased density of ossific nucleus & cessation of growth
2. Resorption / fragmentation
Duration : 6/12
Pathologic Process
- necrotic bone irregularly resorbed / creeping substitution
- replaced with vascular fibrous tissue
- may be associated with collapse
XRay - Fragmentation of Physis
3. Reossification
Duration : 1.5 - 3 years
Pathologic Process
- starts at margins & progresses centrally
- eventually new areas coalesce & epiphysis regains normal strength & density
XRay
- Better defined shape
- Return of bone density
4. Remodelling
Duration : Occurs until skeletal maturity
Xray - May have flattening of the head and neck
Herring Lateral Pillar
AP xray when disease in fragmentation / divide femoral head into 3 pillars
- lateral (25%)
- medial (25%)
- central (50%)
Group A
- no lateral pillar collapse or radiolucency
- all become Stuhlberg 1 & 2
Group B
- > 50% of lateral pillar height maintained
- outcome depends on age
- < age 9 almost all become Stuhlberg I and II
- > age 9 30% become Stuhlberg II / 70% become Stuhlberg III or IV
Group C
- pillar < 50% normal height
- majority do poorly
Catterall
Technique
- uses AP & lateral xray
- 4 groups
- significant inter & intra-observer error
Group I
- < 25% involved
- anterocentral head
Group II
- 25-50% head
- anterolateral region / lateral column intact
Group III
- 50-75% head involvement
- moderate collapse
Group IV
- 100% of head sequestered
- severe collapse
Salter-Thompson
Group A
- Catterall 1 and 2
- < 1/2 of head involved
- viable lateral pillar
- good prognosis
Group B
- Catterall 3 and 4
- > 1/2 head involved, loss of lateral pillar
- poorer prognosis
Mose
Quantifies degree of sphericity
- graded according to variance from perfect circle in either AP or lat
- many authors do not agree that Mose sphericity is accurate predictor of long term outcome
- good or fair Mose rating = good result
- poor Mose rating not necessarily = poor result
Good - no deviation on the 2 views
Fair - up to 2 mm variance
Poor - 3 mm or more variance
Stuhlberg
Based on congruency & sphericity
Class 1
- normal
- 0 % OA
Class II: Spherical & Congruent
- femoral head spherical (mose circles overlaid on AP / lateral of femoral head show <2mm variation)
- At least 2 other abnormal features including Coxa Magna , Coxa Breva or Abnormally Steep Acetabulum
- 15% OA
Class III: Aspherical Congruity
- head ovoid (mushroom or umbrella shaped) and aspherical i.e Mose circles show > 2mm variation
- 60% OA in middle age
Class IV: Aspherical Congruous Incongruity
- head flat, steep acetabulum
- 75% OA usually in middle age
Class V: Aspherical Incongruous Incongruity
- head flat, normal acetabulum
- 80% OA at young age before 50
Natural History
Osteoarthritis 10x more prevalent than general population
Only 40% have normal radiographs
20-40 years after onset of symptoms
- 80% active & pain-free
- only 10% have THR
At 50 years after onset of symptoms
- 50% have disabling pain
- 40% have THR
Weinstein
- probably best you can say is function deteriorates with time
- 50% THR at 50 years
Prognostic Factors
1. Age of onset
- most important
- < 6 good Stulberg I-II
- 6-9 variable Stulberg I-IV
- > 9 Stulberg III & IV
- related to amount skeletal growth & thus remodeling available
2. Sex
- F worse than M
- ? early maturation, less time to remodel
3. Extent head involvement
- quantified by Caterall / Salter-Thompson / Herring classification
4. Containment of head
- extrusion and asymmetric growth leads to worse prognosis
5. ROM
- hip irritability causes adductor tightness
- loss of abduction ROM prevents remodeling head by acetabulum
7. Lateral Pillar Collapse
Catterall "Head at Risk" Signs
Only lateral subluxation shown to be prognostic
5 Xray
1. Lateral subluxation head
2. Lateral epiphyseal calcification
3. Gage Sign - V shaped defect in lateral physis
4. Horizontal physis angle
5. Metaphyseal cysts
4 Clinical
1. Progressive loss ROM
2. Adduction contracture
3. Flexion with abduction
4. Obesity
Gage's sign
- lateral bulge of metaphysis
- extruded cartilage may calcify lateral to acetabulum
- gives appearance of head extrusion
- coxa breva
Symptoms
Most present early
- 75% during necrotic / fragmentation stages
- insidious painless limp commonest
- ache groin / anterior thigh or knee
- exacerbated by activity
Examination
Short stature
- usually short with delayed bone age
Antalgic / Trendelenberg gait
Decreased ROM
Early
- synovitis with tight adductor and/or psoas
- loss abduction in extension and flexion
- loss IR / flex into ER
Late
- bony impingement
- "hinge subluxation"
- lateral extrusion, flattening & enlargement of head prevent normal motion
LLD usually small
- apparent LLD from adduction contracture
Occasionally thigh / gluteal wasting in advanced cases
Xray
Grade stage of Perthes
Lateral Pillar classification
US
Nonspecific findings of synovitis usually found
- thickening synovial membrane vs. synovitis
- synovial effusion
CT

MRI
Advantage
- can assess amount of cartilaginous head outside of acetabulum
- very good way of assessing containment of cartilage head
DDx
AVN
MED / SED
Hypothyroidism
MED
- bilateral and symmetrical
- acetabular involvement
- no metaphyseal cysts
- other physeal involvement therefore consider skeletal survey in those with bilateral "perthes"

Complications of Perthes
1. LLD 25%
Causes
- subchondral fracture & collapse
- arrest proximal femoral epiphysis
- adductor contracture
- varising osteotomy
2. Trendelenburg gait
Proximal greater trochanter
- collapse of epiphysis / coxa breva
- varus osteotomy
Management
- growth arrest of greater trochanter at 10 years or distal transfer
- femoral neck lengthening osteotomy
3. Hinge abduction
Extrusion of epiphysis laterally
Management
- treat with cheilectomy once physis closed
- has poor reputation
- may worsen arthrosis by exposing fresh bone
- if done prior to physeal closure may cause SUFE or growth arrest
4. Labral tears
Rare
- abnormal stress by head on lateral acetabulum
5. Secondary OA
