Definitions
Juvenile Osteochondritis Dissecans (JOCD)
- abnormality of osteochondral bone in young patients
- combination of repetitive trauma and vascular insult
- often medial
Osteochondral fracture / lesion
- damage to osteochondral bone after trauma
- usually lateral
Osteochondral defect
- loss of bone and cartilage from talus
- may be secondary to trauma
- may be from displacement of loose OCD
Epidemiology
- systematic review of OC lesions after ankle fracture
- 45% incidence of OC lesions, 43% on talus
- systematic review of OC lesions after syndesmotic injury
- 21% incidence of OC lesions, 95% talar dome
History
History of ankle injury with development of chronic symptoms
- activity-related pain, stiffness & swelling
- may have symptoms of loose body / locking
Symptoms of lateral ligament instability
Examination
Tenderness around ankle joint
Pain with dorsiflexion / eversion
Decreased ROM, especially dorsiflexion
Effusion
Test for ligament instability
DDx
Chronic ligament instability
Lateral gutter soft tissue impingement
Calcaneal fracture
Lateral process fracture of the talus
Tarsal coalition
Sinus tarsi syndrome
Location
1. Anterolateral / ? traumatic
2. Posteromedial / ? atraumatic
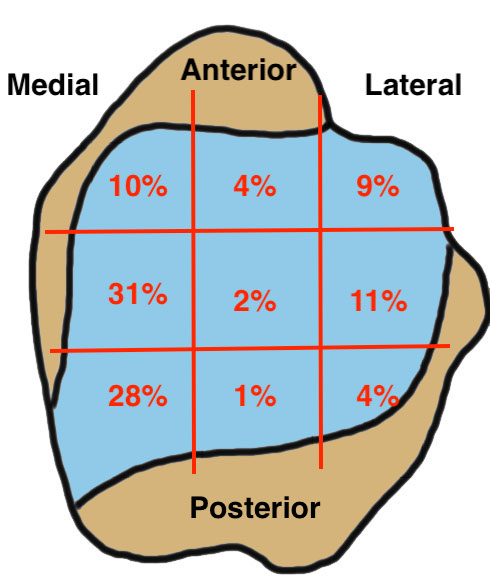
van Diepen et al Cartilage 2021
- systematic review of 2000 OC lesions of the talus
- 9 grid system
- 28% posteromedial
- 31% centromedial
Berndt & Harty Xray Classification
Stage I - subchondral compression fracture
Stage II - partially detached osteochondral fragment
Stage III - completely detached fragment, non displaced
Stage IV - completely detached and displaced fragment
Xray


Stage II medial osteochondral fragments



Stage III medial osteochondral fragments


Stage IV anterolateral osteochondral fragment
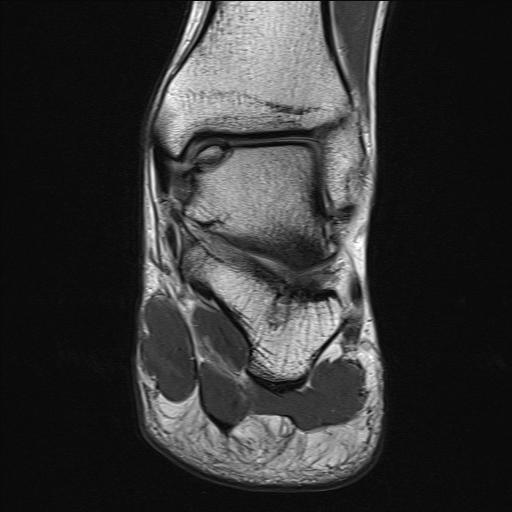
MRI
Stable lesion (Stage I) - cartilage intact, no synovial fluid under lesion
Unstable lesions (Stage II or III) - cartilage breach, synovial fluid under lesion
Displaced lesion with resultant osteochondral defect
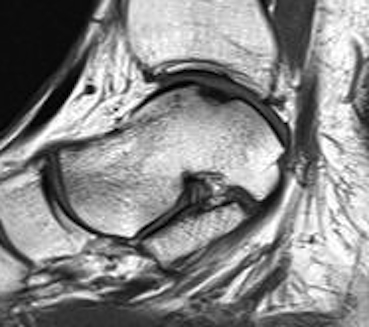

Stable lesion with intact cartilage and no synovial fluid under lesion
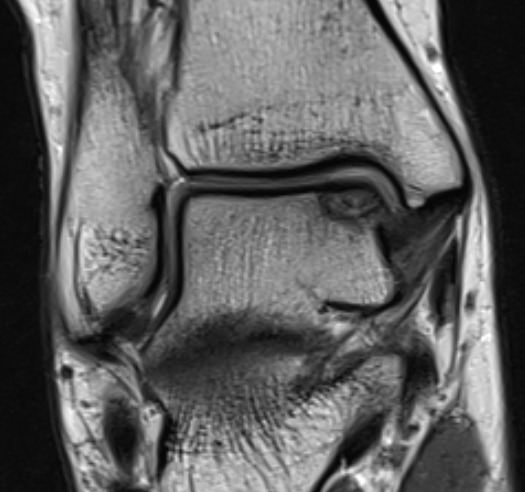
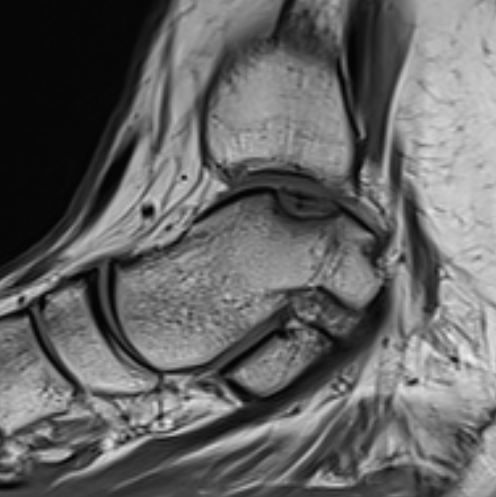


Stage III completely detached but not displaced
CT

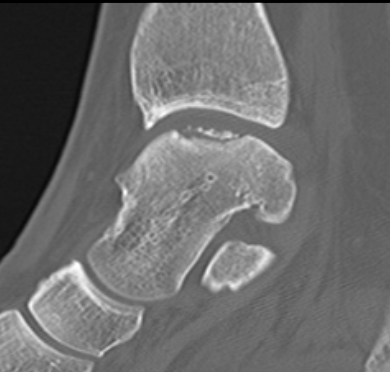
Stage III
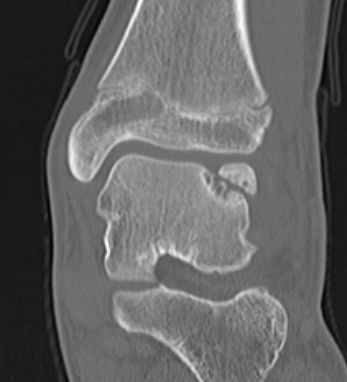
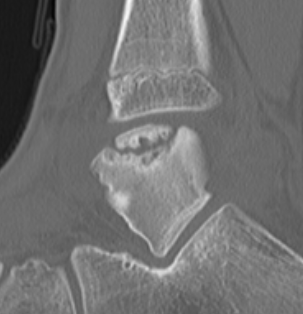
Stage III

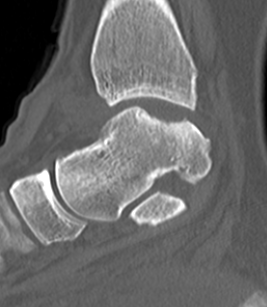
Stage IV displaced fragment with osteochondral defect
Management
Management Algorithm
Stable lesion (Stage 1)
- if cartilage intact, initial non operative care
- drill in situ +/- screw fixation if no healing with non operative care
Unstable in situ lesion (Stage 2/3)
- large lesion: screw fixation
- small lesion: remove + microfracture / cartilage restoration
Displaced fragment with osteochondral lesion (Stage IV)
- ORIF if possible (i.e fragment is large and replaceable)
- remove + microfracture / cartilage restoration
Non Operative Management
Indications
Juvenile Osteochondritis Dissecans (JOCD) in adolescent with open growth plates
Stable lesion - intact cartilage
Technique
Touch weight bear 6 weeks
No sport 6 months
Results
Perumal et al J Pediatr Orthop 2007
- 31 patients with JOCD and open growth plates
- mean age of 12
- 6 months non operative management: 16% healed
- 12 months non operative management: 42% surgery for pain, 46% asymptomatic with visible lesions
Kim et al Clin J Sports Med 2022
- 55 JOCD treated with nonoperative management
- 77% healed
- increased risk nonunion with older age and completely detached lesions
Operative Management
Options
Drill
Screw fixation
Remove + marrow stimulation / cartilage restoration
Drilling
Indication
Stable lesion with intact cartilage
Options
Antegrade
- through cartilage surface of talar dome
- may have to go through medial malleolus for posteromedial lesions
Retroarticular
- transtalar
- uses image / arthroscopy / navigation
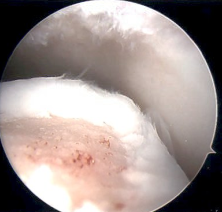
Screw fixation


Indications
Large fragment in situ
Technique
Lift, drill, fill, fix (LDFF)
- partially displace
- debride base +/- microfracture
- consider bone graft
- secure with headless compression screws
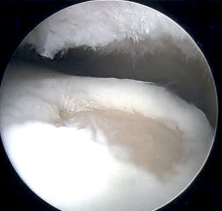
Arthroscopy Approaches
Arthroscopy techniques medial transmalleolar screw fixation PDF
Anterolateral / anteromedial
- anterior 50 - 60% lesions
Posterolateral / posteromedial
- prone
- posterior lesions
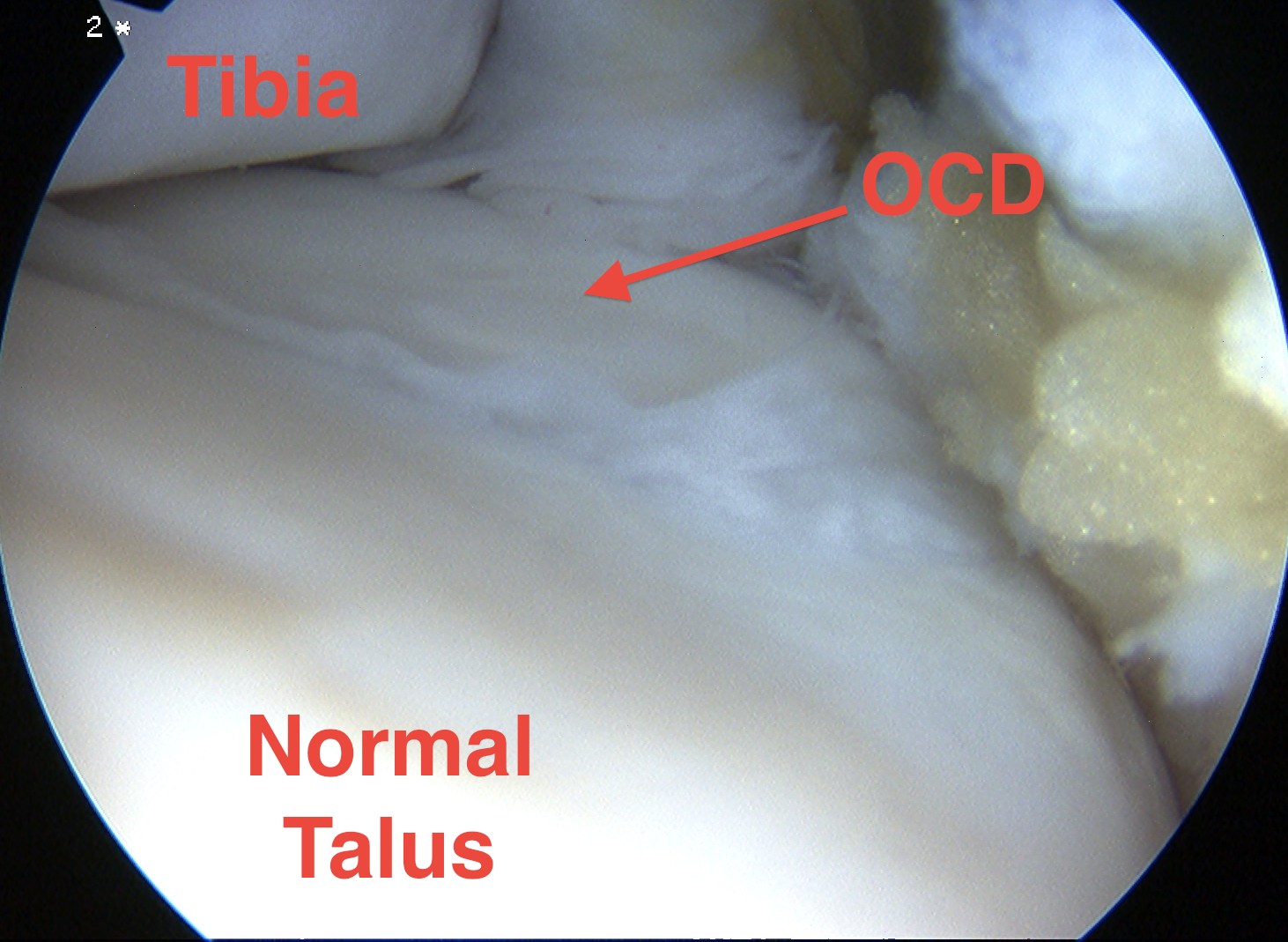
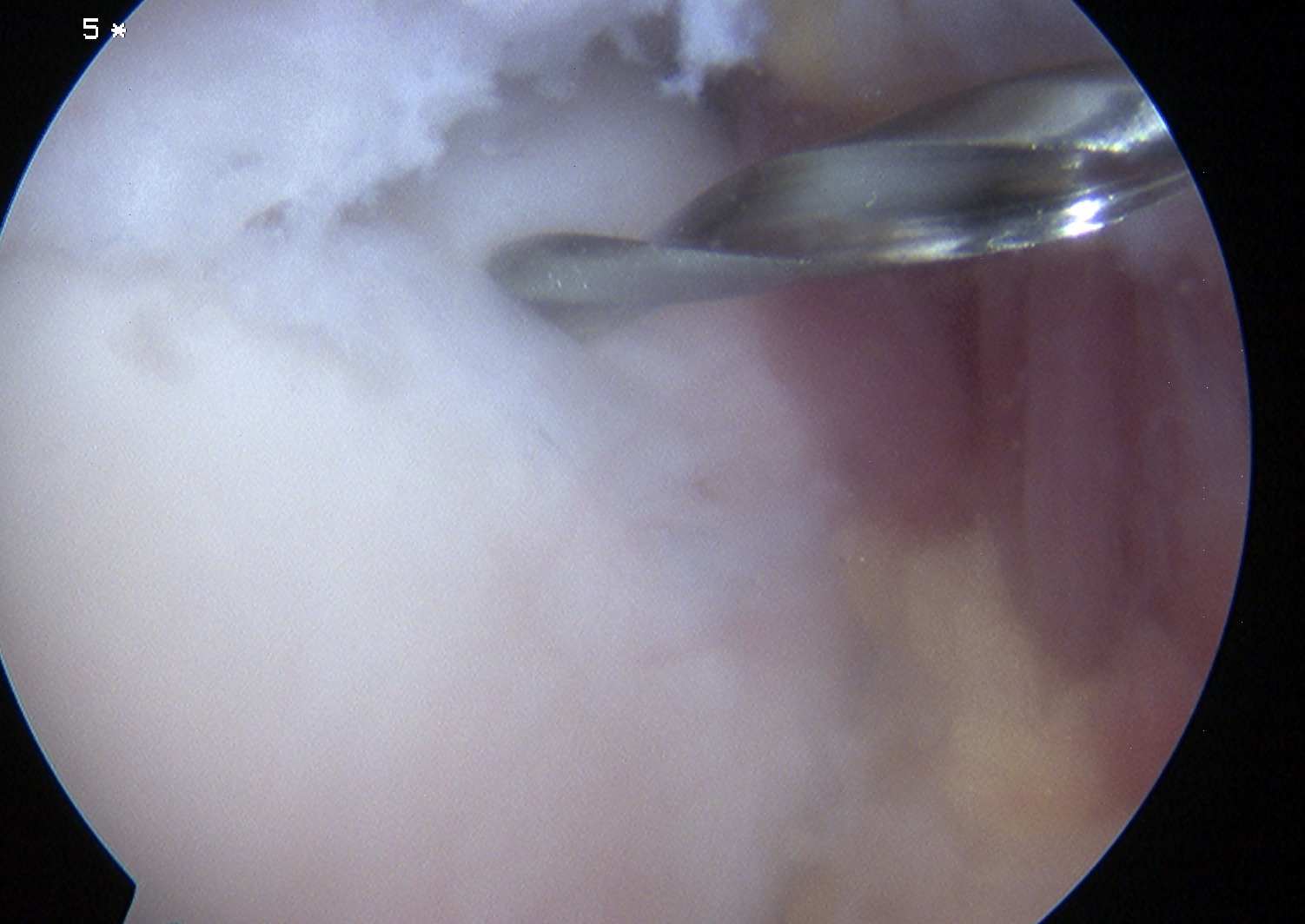
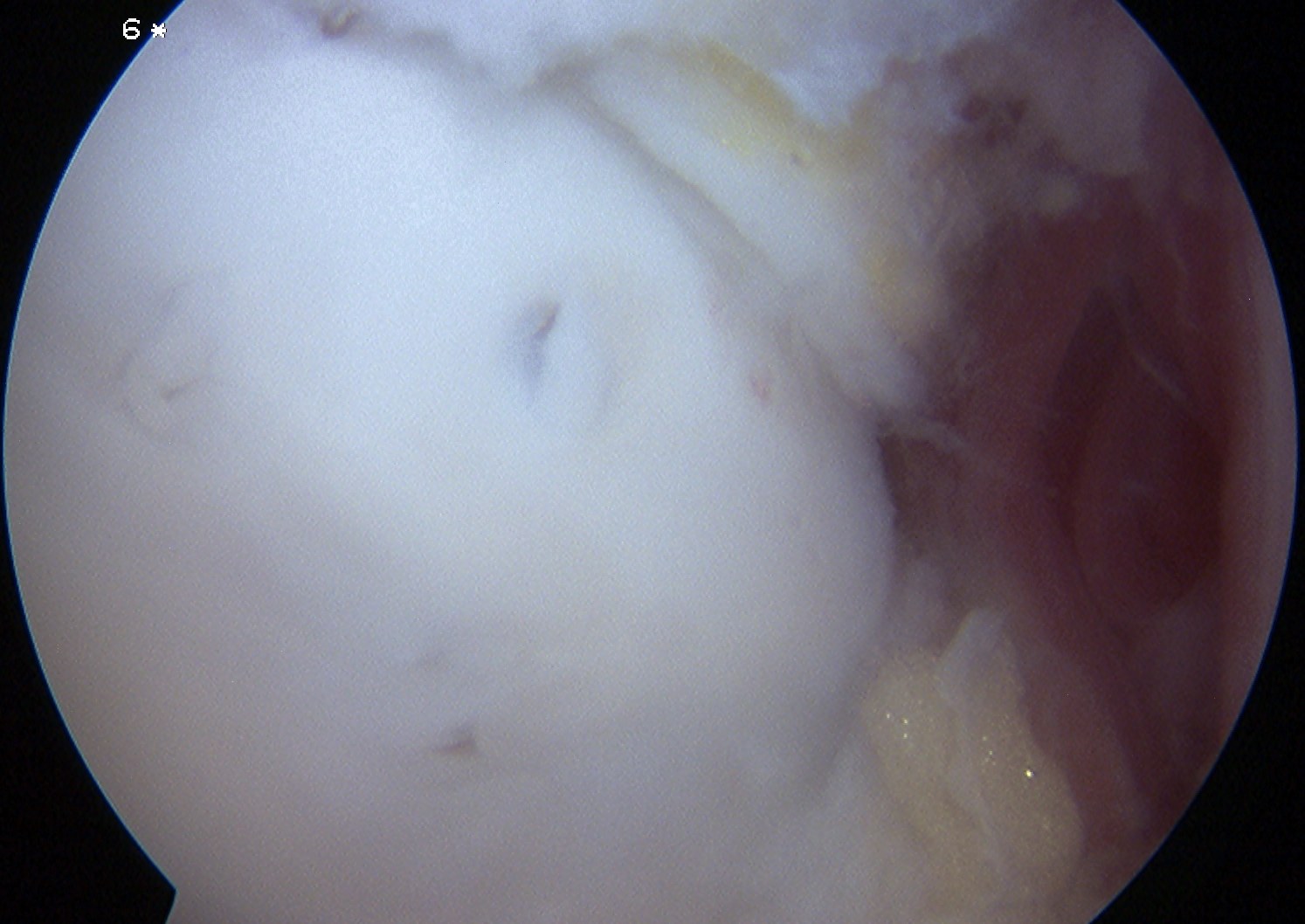
Anterolateral osteochondral lesion accessible via plantarflexing the ankle
Open approaches
Vumedi open approaches to talus OCL
Lateral lesion
- more anterior lesions accessible with anterolateral approach
- ± Anterior plafond osteotomy ± Chaput anterolateral osteotomy if large
Medial lesion
- often more posterior
- may require medial malleolar osteotomy
Medial Malleolar osteotomy
Predrill for screws
Arthrotomy / image guidance
Posterior homan to protect tibialis posterior
Initial osteotomy with saw / complete with osteotome
Surgical technique PDF medial malleolar osteotomy
Vumedi surgical technique medial malleolar osteotomy video



Results
- ORIF of 44 talus lesions
- treatment failure in 1 patient
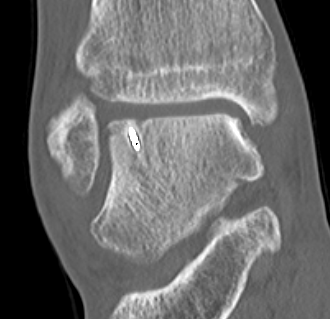
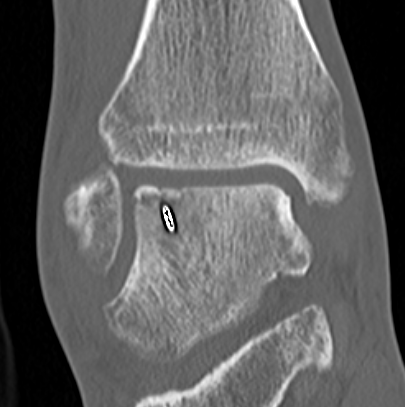
CT assessment of bony healing post ORIF with screws
Excision + microfracture / cartilage restoration
www.boneschool.com/osteochondraldefecttalus