Aim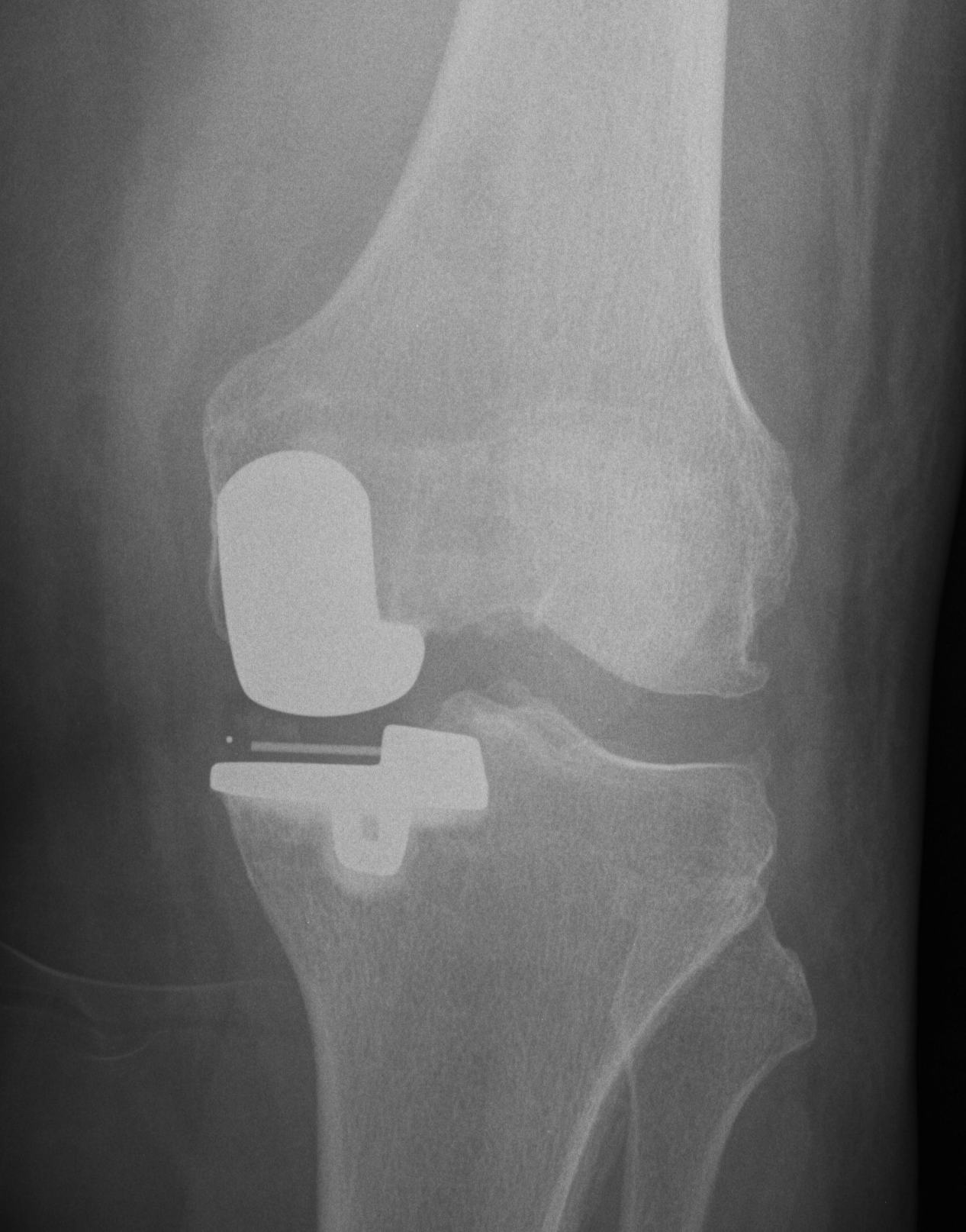
UKA is intended to be load sharing
- correct to neutral or slight varus
HTO is a load-shifting / load-sparing procedure
- over correct into valgus
UKA v TKR
Advantages UKA
1. Rapid rehabilation
2. Increased ROM
3. More normal knee kinematics
- more normal gait
- preserves ACL, PCL, PFJ & lateral compartment
4. Low complication rate
- decreased infection, bleeding
Results
Laurencin Clin Ortho 1991
- TKR one side, UKA other
- patients preferred UKA
Newman JBJS Br 1998
- randomised trial TKR v UKA
- UKA less perioperative morbidity, faster ROM, better knee scores
Disadvantages UKA
1. Technically difficult
2. Progressive OA of un-resurfaced compartments
3. Inferior survivorship to TKR
- higher revision rates in young
- revision rates in Australian Joint Registry approach TKR only in > 75 year old patient
4. More difficult future TKR with poorer results
- revision rate of TKR post Uni is close to 10% 5 year in AJR
UKA v HTO
Advantages UKA
Fewer complications
- higher earlier success rate
- more rapid rehabilitation
Stukenborg et al Knee 2001
- randomised prospective
- 7 - 10 year survival
- 77% UKA
- 60% HTO
- higher complication rate in HTO
Indications
Kozinn and Scott JBJS Am 1989
- minimal deformity
- only medial compartment OA
- asymptomatic mild PFJ OA
Unicompartmental OA +
- intact ACL
- FFD < 5°
- flexion > 90° (probably more, 110-130o)
- maximum varus 15o which is correctable to neutral
- older age group (> 60 years)
- lower weight < 82 kg
- lower activity level
Only 6% of patients fulfil these criteria
Contraindications
Instability
- ACL deficiency
- tibial / joint subluxation
- lateral thrust
If ACL gone allows varus in all positions
- subsequent global joint erosions
Significant OA changes in other compartment
- some surgeons ignore PF if non symptomatic
- only early changes in lateral compartment
- examine at time of surgery
Inflammatory arthritis
Assessment
One finger test
- patient points to affected compartment only
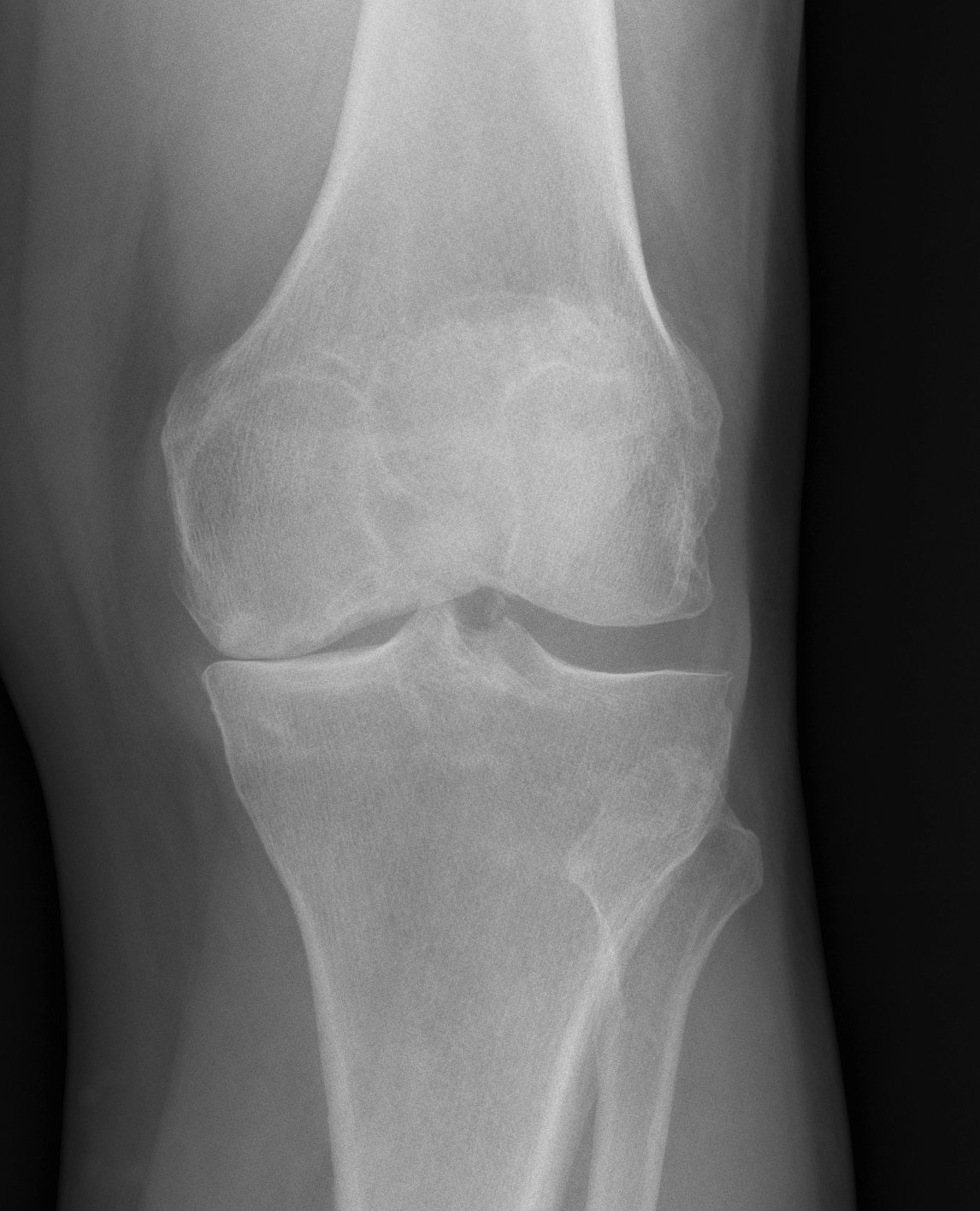
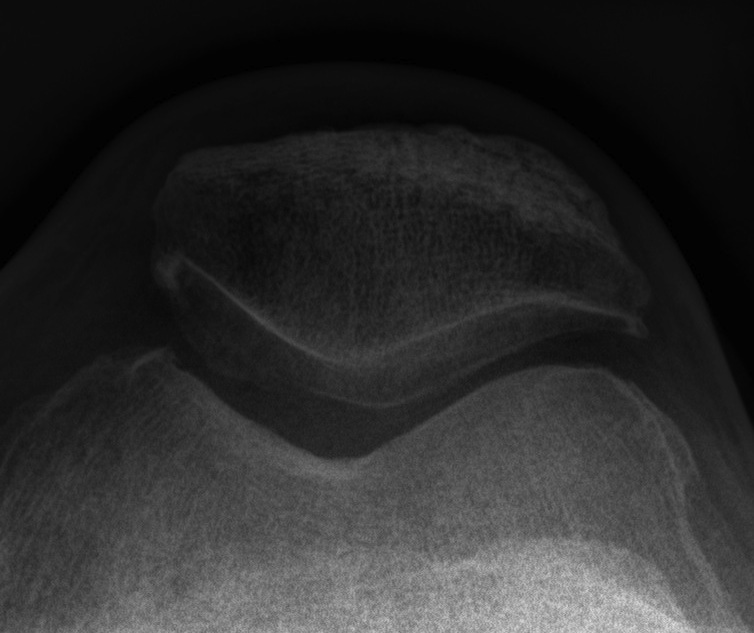
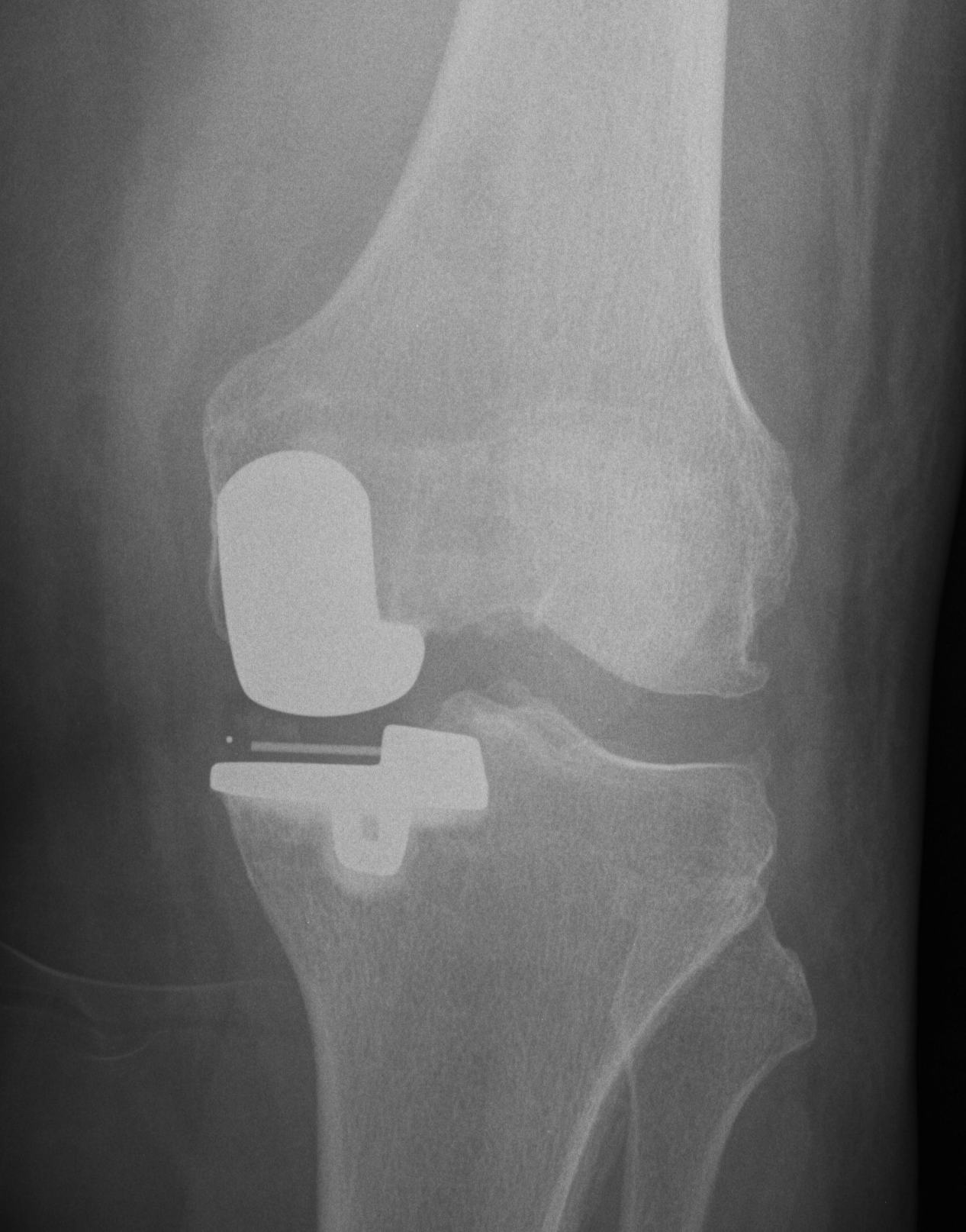
X-rays
AP / Lateral / Skyline
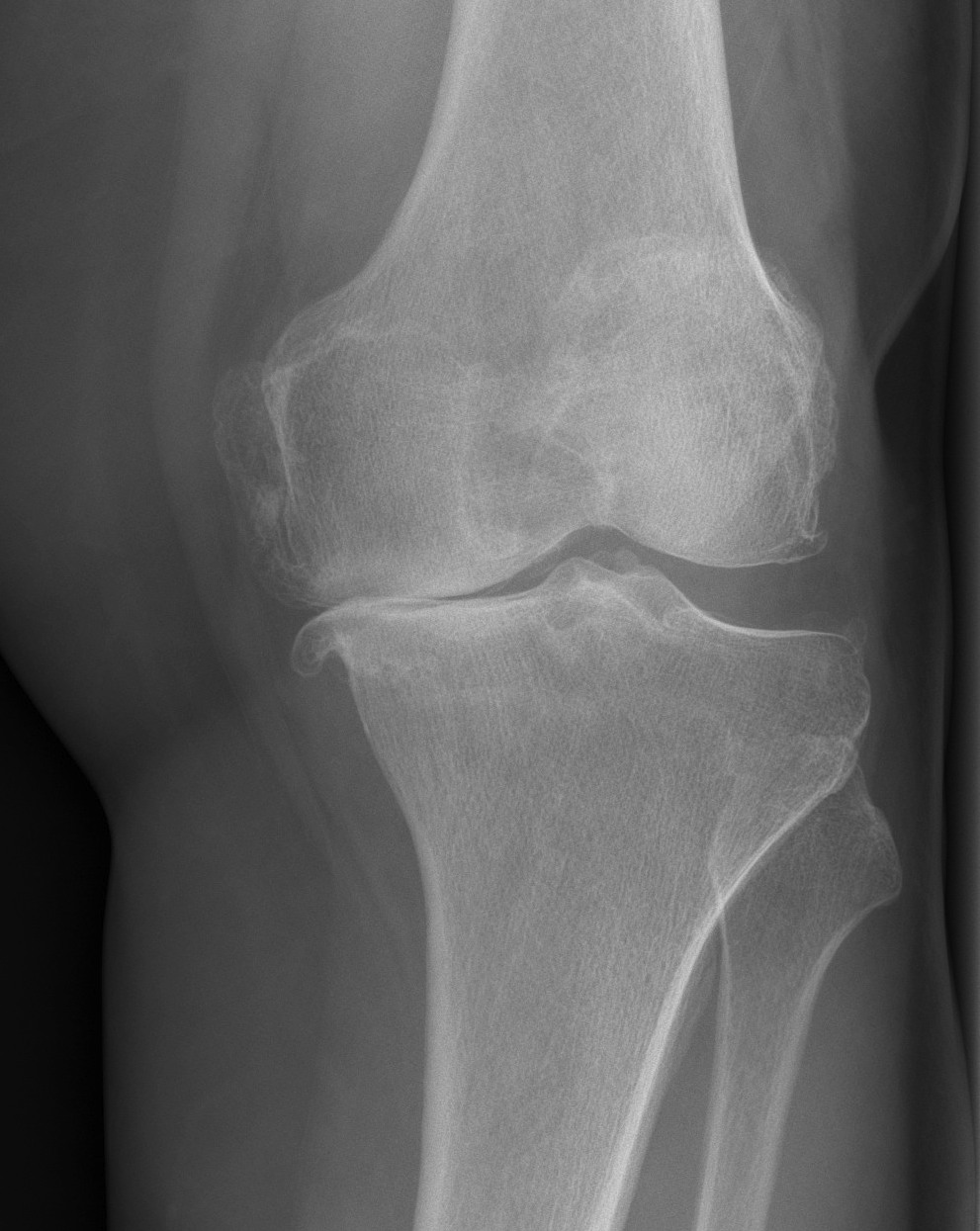
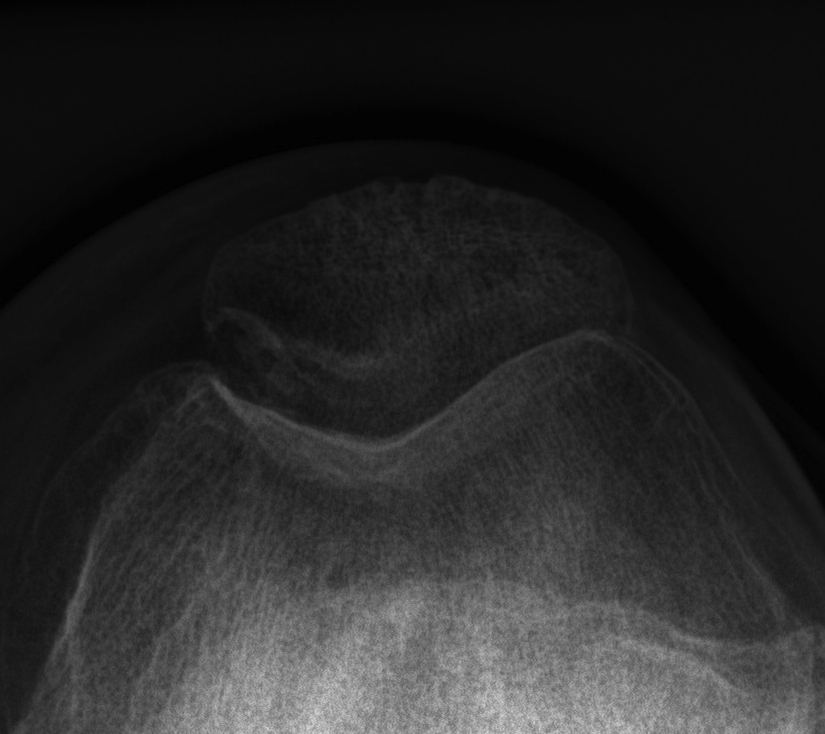
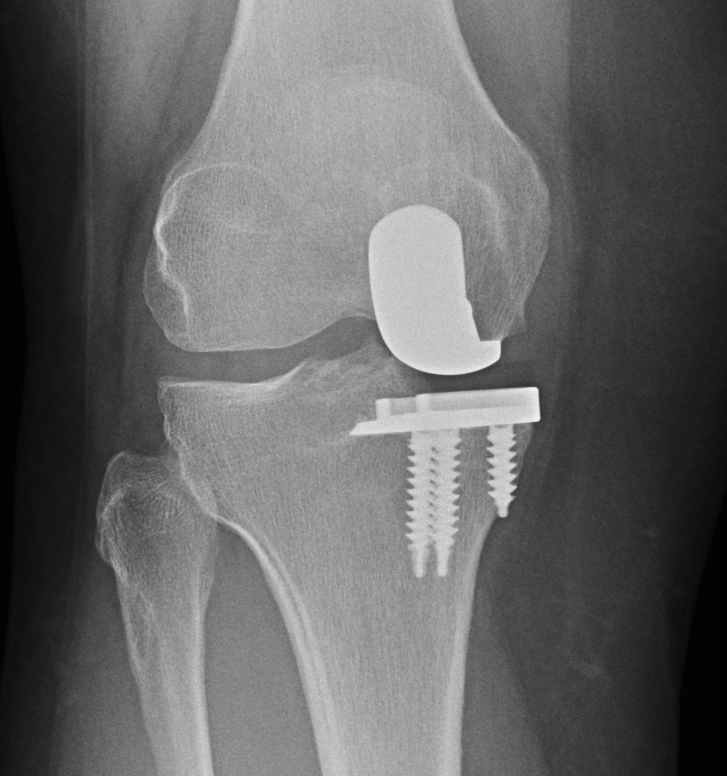
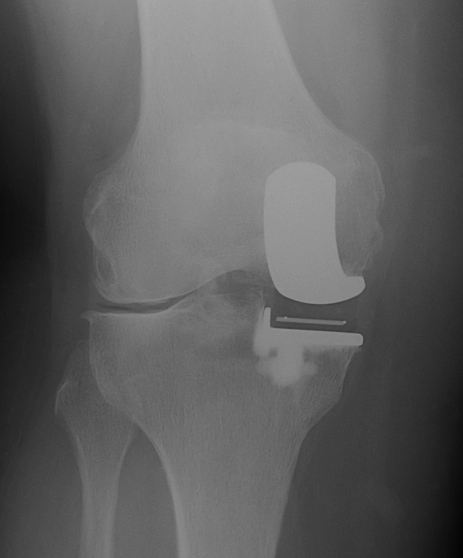
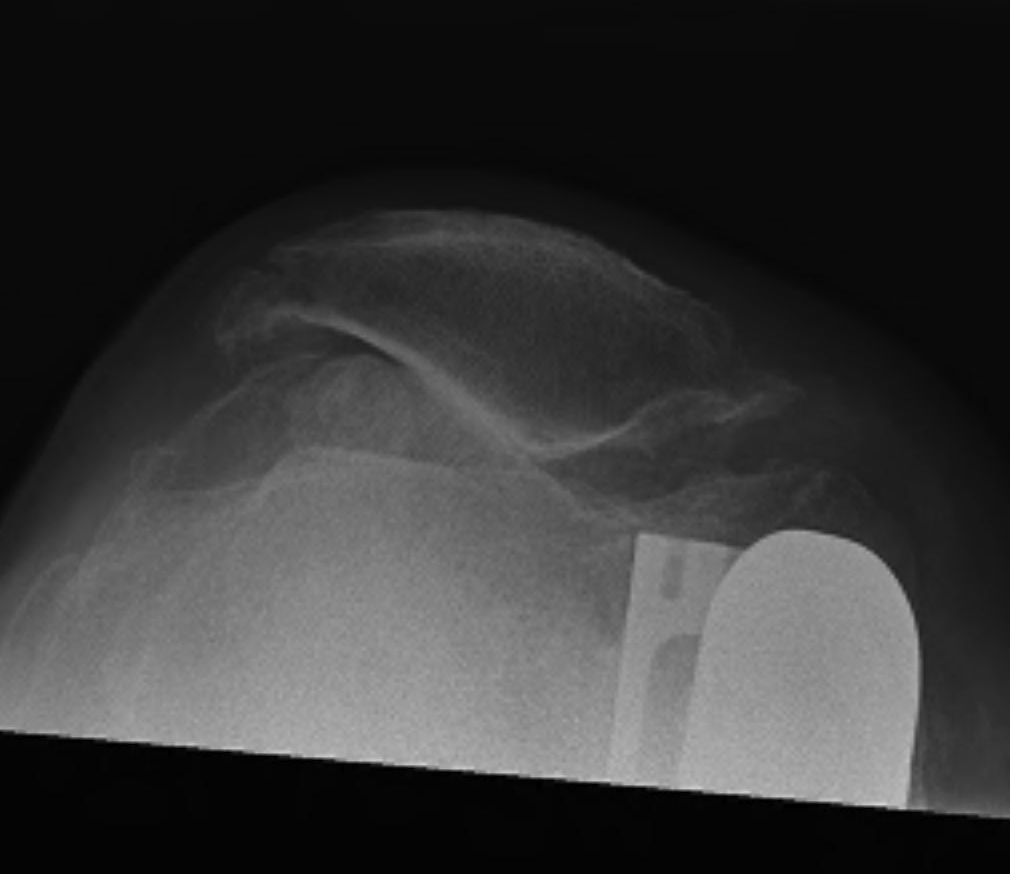
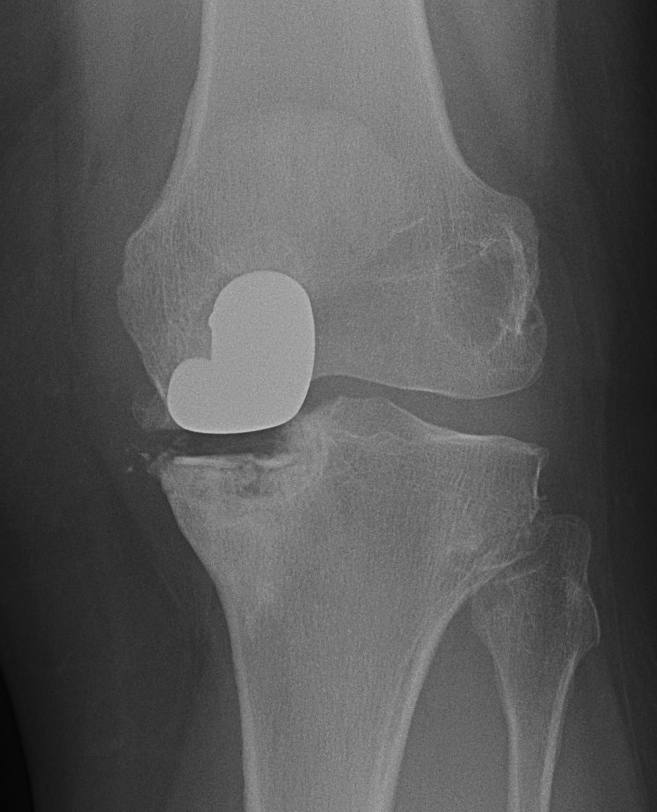
Patient 1

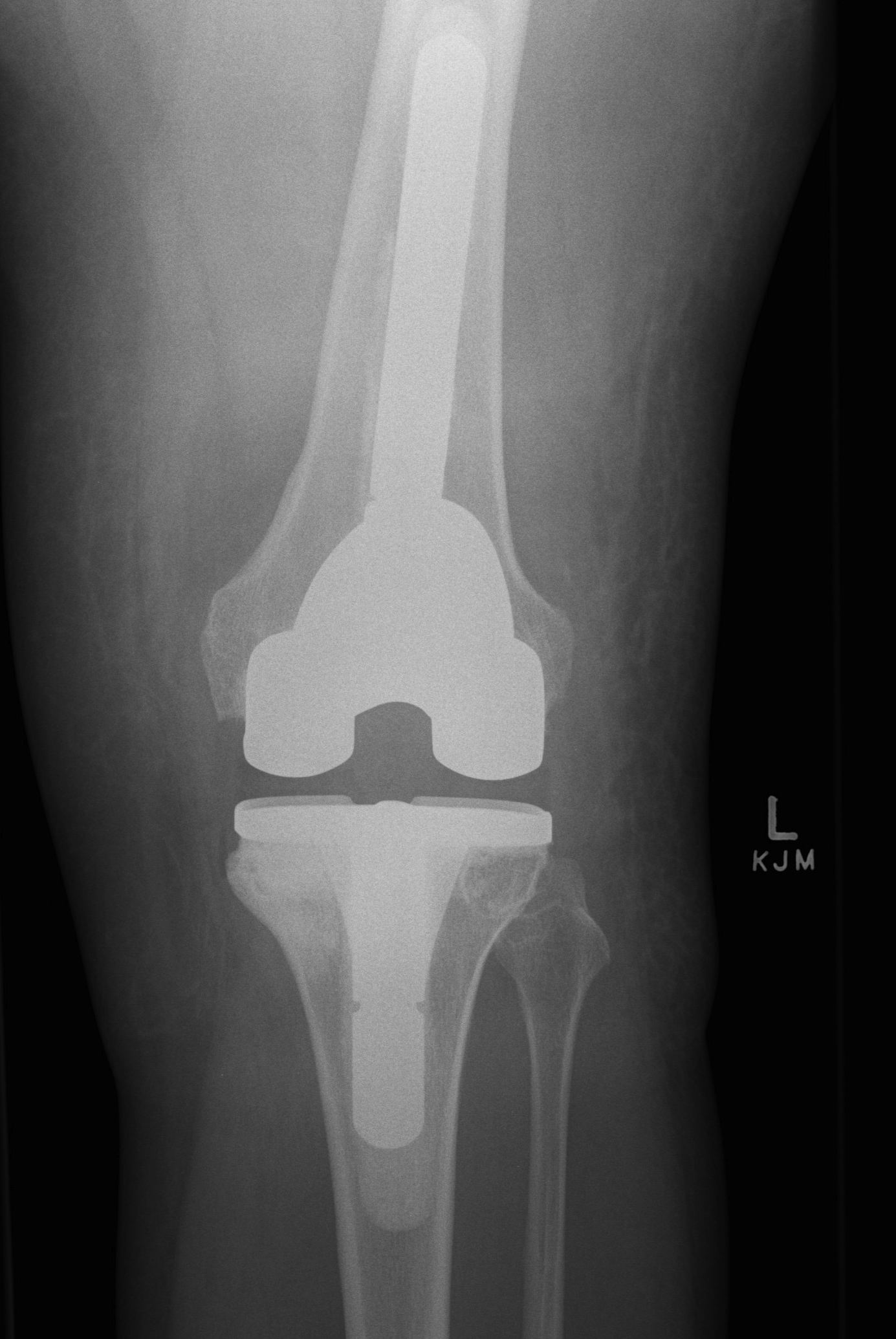
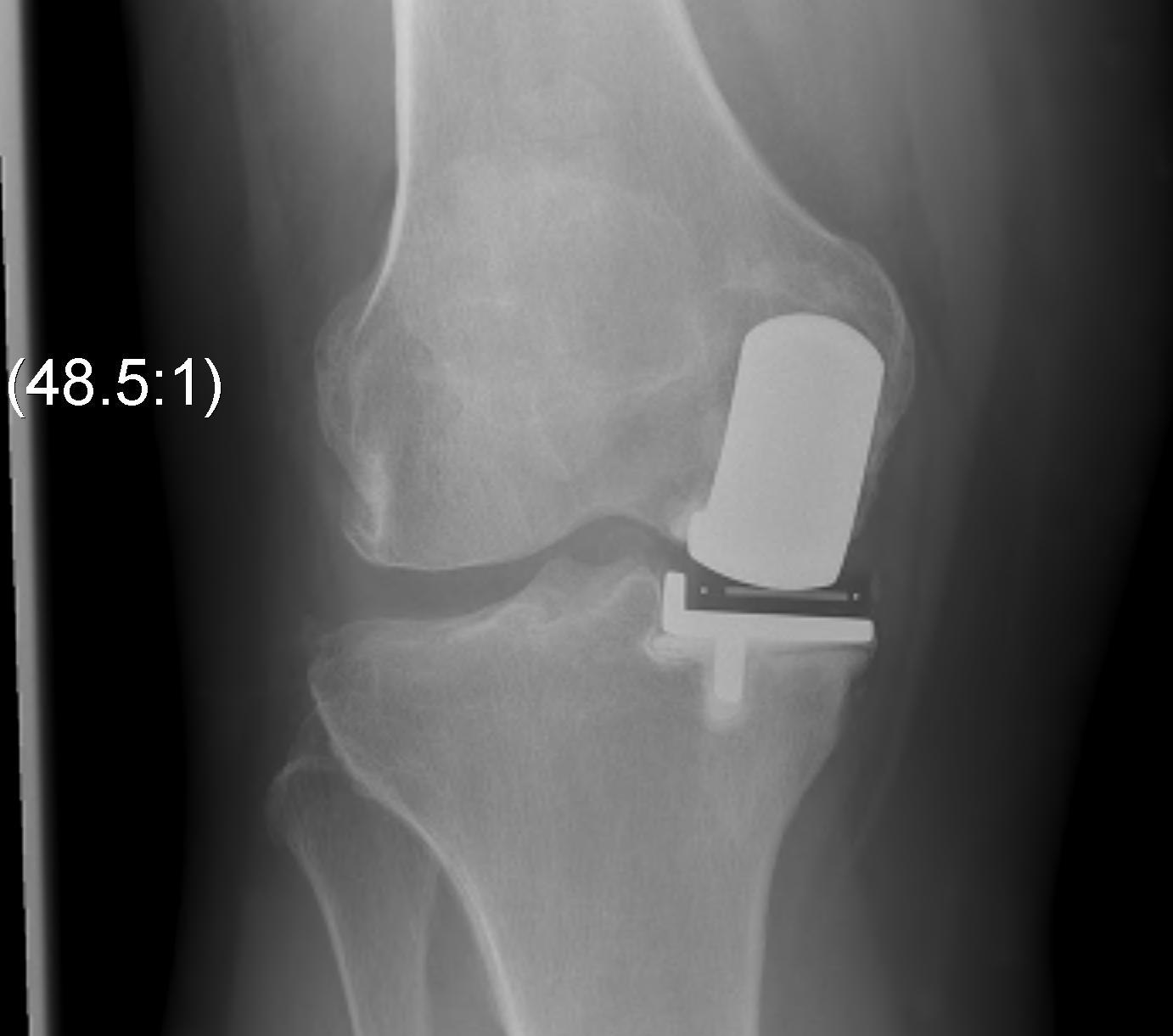
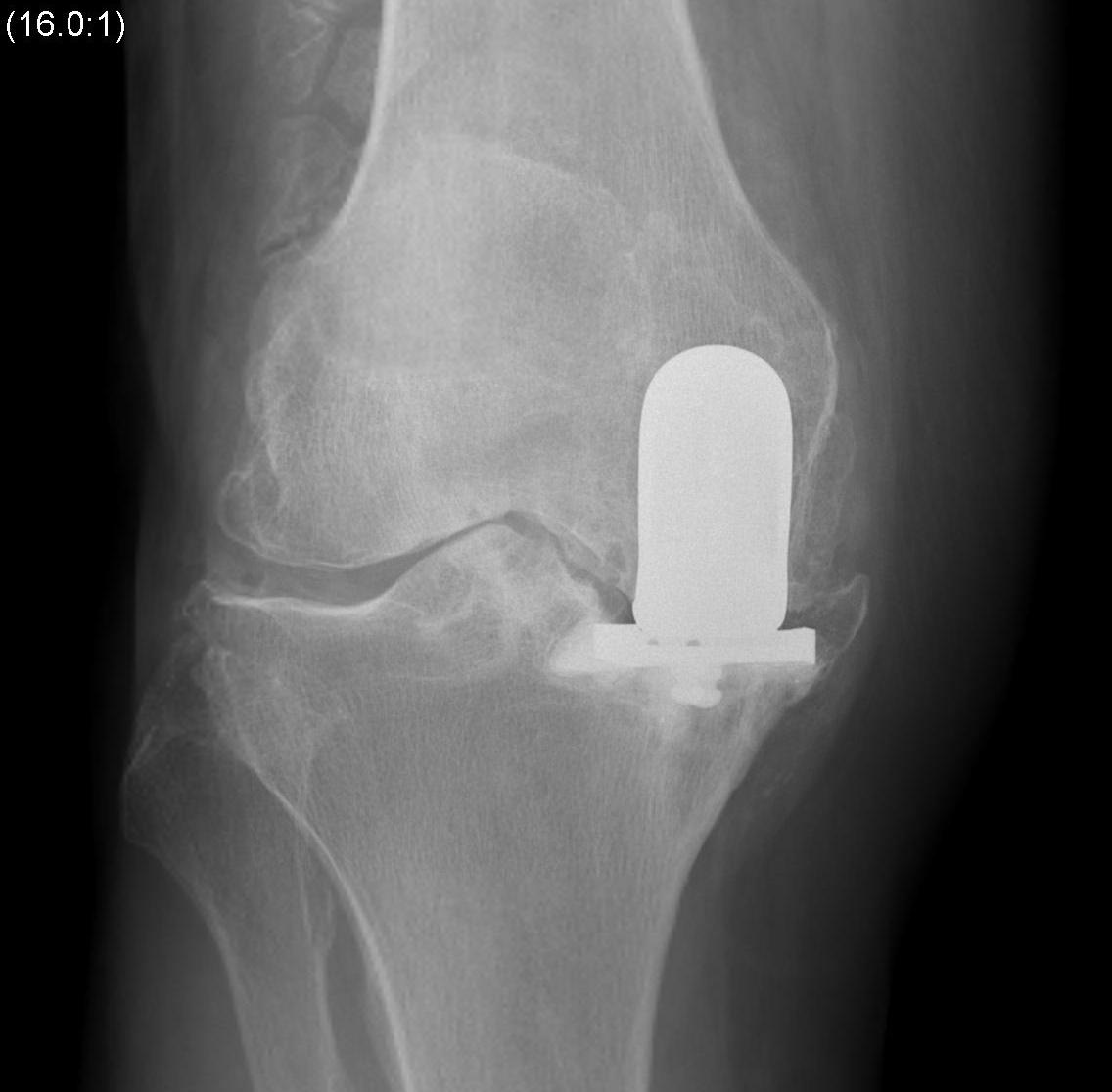
Patient 2

Surgical Principles
1. Correct to neutral or slight varus
2. Femoral component
- should be centred on condyle
- parallel to tibial component
- must not overstuff
- must not impinge on patella
3. Tibial component
- minimal resection
- must be perpendicular to long axis tibia
- must not be in varus
- should cap but not overhang medial cortex to prevent irritation of pes anserinus
4. Balance flexion extension gaps
- don't overstuff with poly
- 2mm laxity in flexion and extension
Prosthesis
Oxford
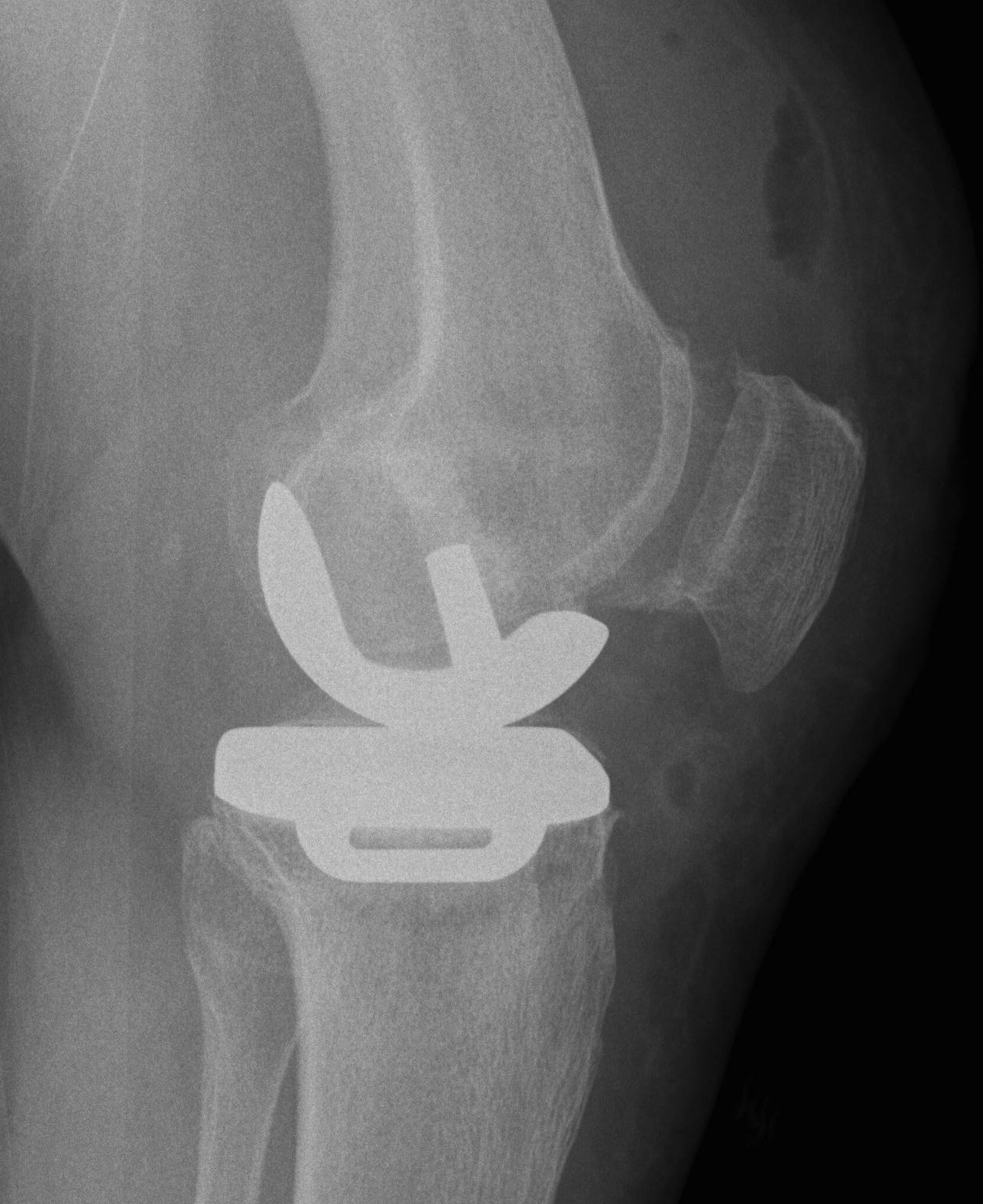
Design
- spherical, constant radius femur, fully congruent
- mobile bearing (risk bearing dislocation)
- flat tibia
Variations on Oxford design
- fixed bearing
- all poly tibia
- uncemented tibia + screws

Complications
1. Bearing dislocation
2. Poly wear

3. Pes anserine bursitis
4. Patella impingement
- femoral component not flush in sagittal plane
- don't oversize femoral component
5. Aseptic loosening
Cause
- no difference fixed v mobile bearing
- undercorrection of deformity
- malalignement of components


6. Tibial Subsidence
- too much bone taken from tibia (into soft bone)
- overimpaction of tibial component
7. Progressive OA
- overcorrection of deformity overloads lateral component
- degeneration of PFJ
8. Infection
- 0.8% UKA
- 2% TKA
Results
UKA
Price and Svard AAOS 2000
- Oxford Knee
- 95% 10 year survival
Swedish knee registry
90% survival at 5 years
- failure rate varies 0 - 30% in different centres
Australian Joint Registry
12.1% revision rate at 7 years
- 3 times the revision rate of TKR
Risk of revision decreases with age
- < 55 20% 7 year revision
- > 75 6% 7 year revision
- but worse than TKA for all ages and gender
Prosthesis
- Oxford 11.5% 7 year revision
- LCS 20.4% 7 year revision
Revision of UKA to TKA
- 12.9% 5 year revision of that TKA
- 3.5 x primary TKA
Summary
- joint registry has poor results
- specialised centres have good results
- need to carefully select patients
- be an experienced unicompartmental surgeon
- perform good surgery
Lateral Unicompartmental Knee
Gunther et al 1996 with 53 Oxford knees
- 75% seven-year cumulative survival rates
- main problem was with dislocation of bearing
Findings
- suggest poorer results with lateral replacements
- suggests fixed bearing may be more suitable in lateral compartment
Conversion to TKR

Problem is bone loss
- up to 75% need grafting / augments
- need to take minimal bone at primary surgery
- watch closely for signs osteolysis
Results
- worse if need augments / stems