Approach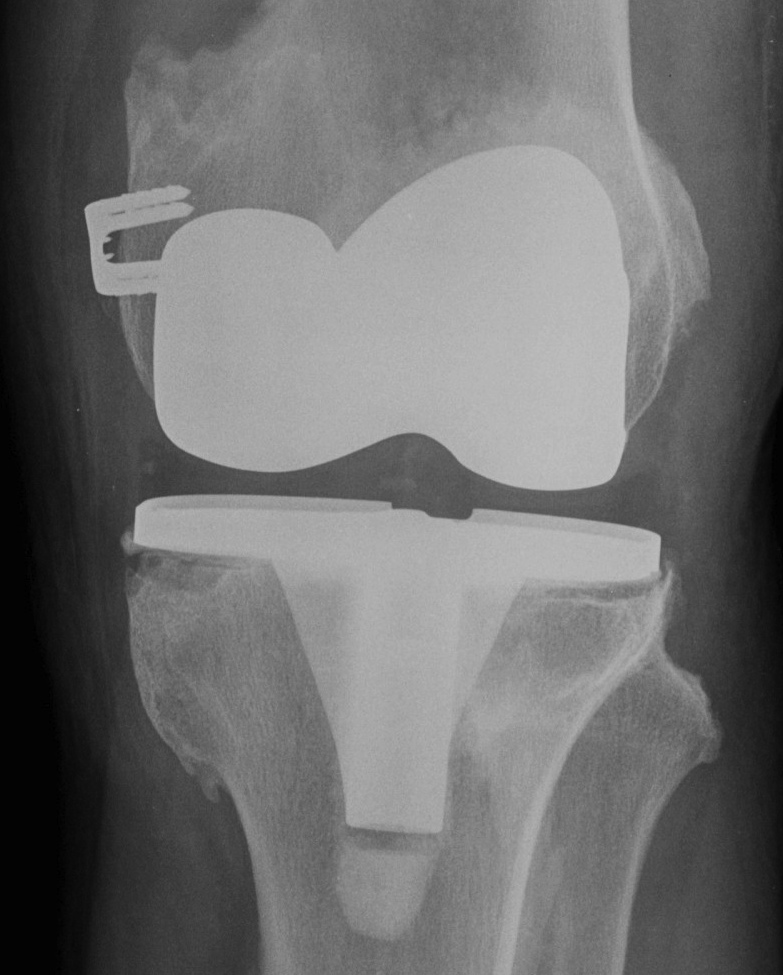
Incision
Always use the most lateral scar
- blood supply comes from medial aspect
- want to avoid a large lateral flap of dubious quality
- cross transverse scars at 90o
- minimum 7 cm skin bridge
Options
- can do trial / sham incision down to capsule
- can perform skin expansion prior to surgery
- consider plastic surgical review for muscle flap
(medial gastrocnemius rotation flap)
Approach
Excise scar tissue
- recreate medial and lateral gutters
- recreate suprapatellar bursa
Patella eversion
- can just slide patella off laterally rather than evert
- put pin in tibial tuberosity to protect patella tendon insertion
Extensile exposures
1. Quadriceps snip
2. Quadriceps turndown
Rarely used
- risk AVN of patella
May consider if limited flexion
- lengthen quadriceps tendon
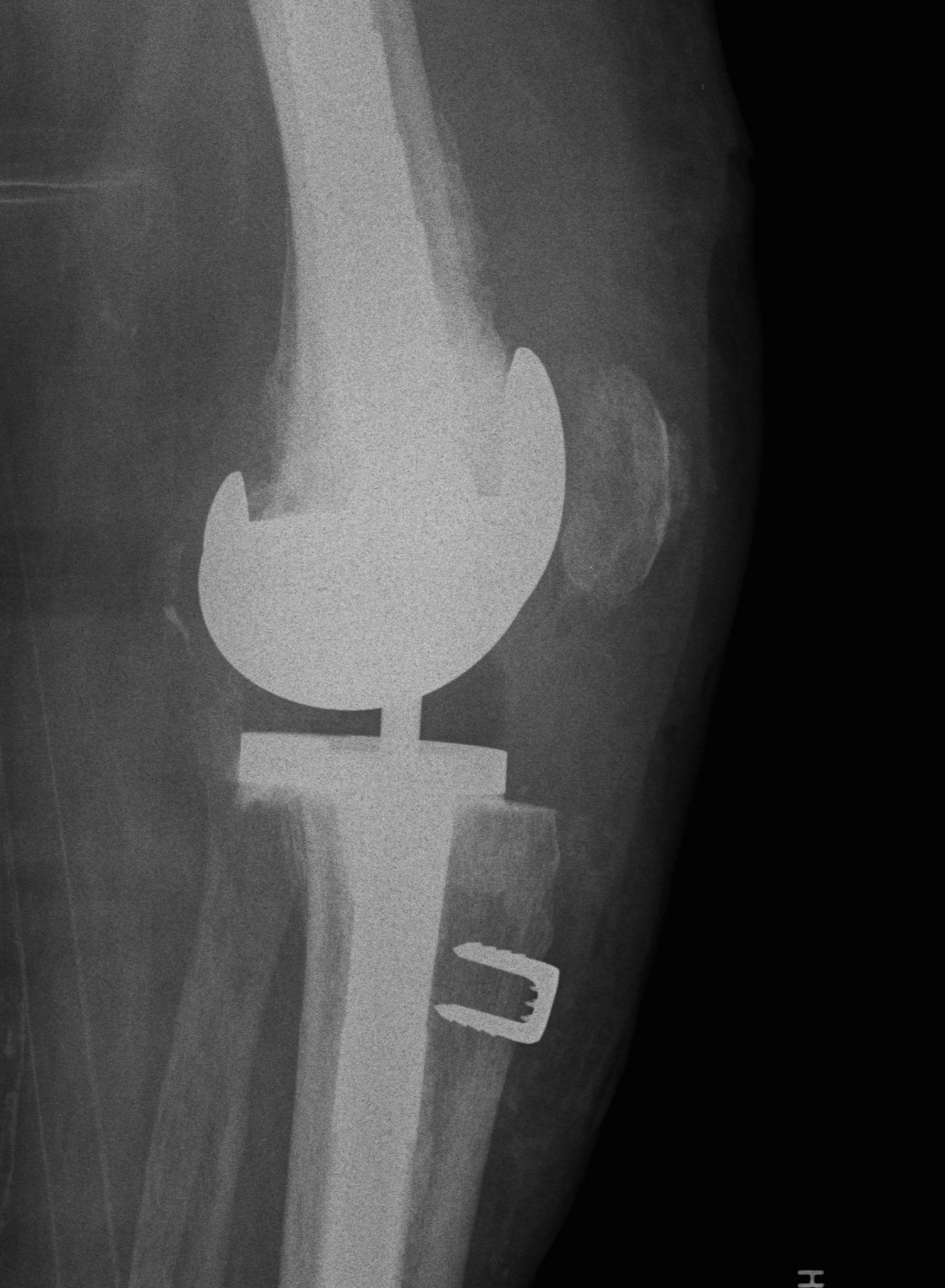
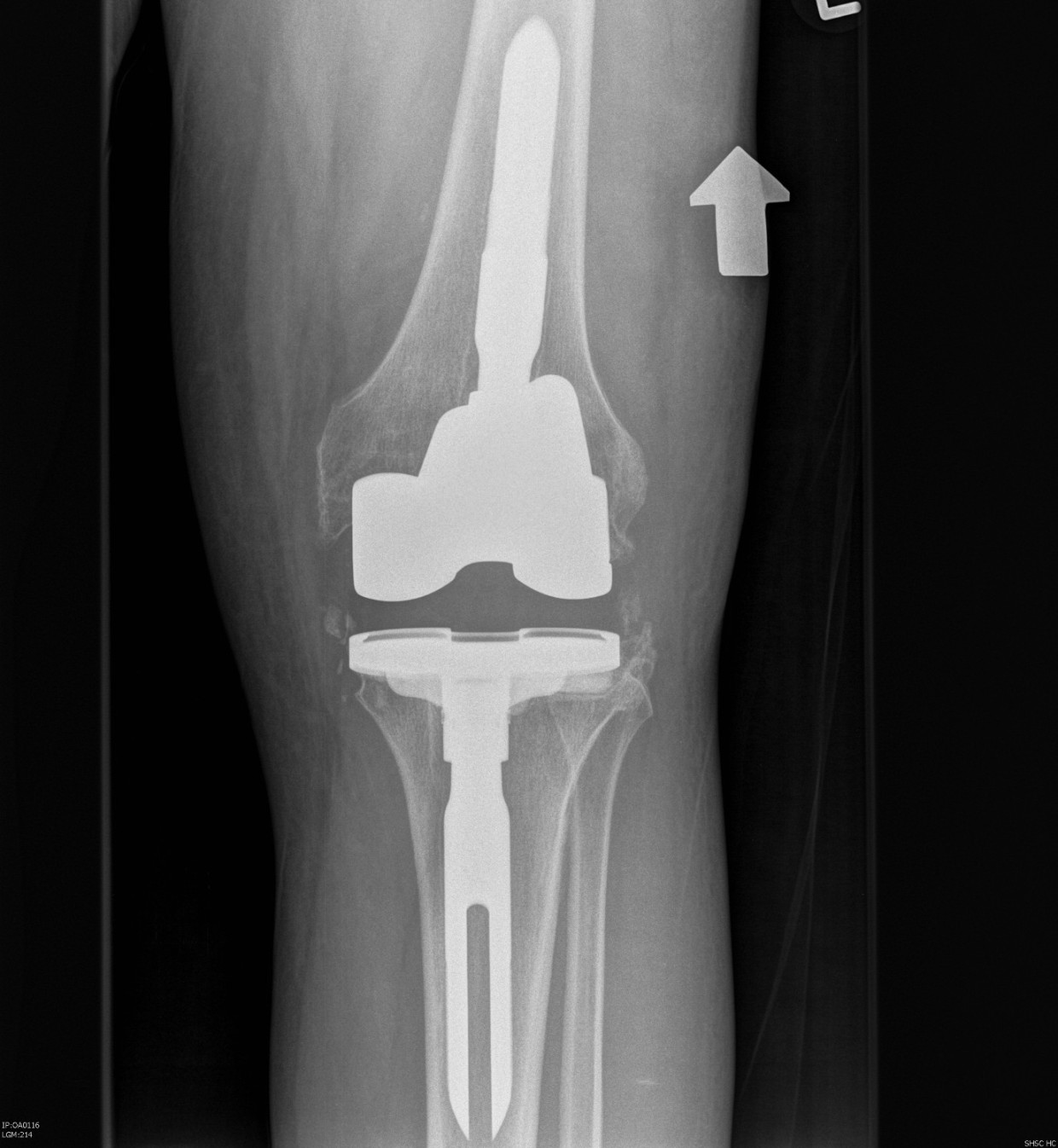
3. Tibial tuberosity osteotomy
- 6-10 cm long, 2 cm wide, 1 cm thick
- lateral periosteum intact / lever open laterally
- bypass osteotomy with stem
- need to wire back around the tibial stem
- place wires before definitive stem
- drill holes medially and laterally
- can use diverging screws as well
Removal of components
Remove poly
- implant specific tools
Careful removal implants to minimise bone loss
- thin, flexible osteotomes, micro-sagittal saw
- gigli saw
- can cut metal with carbide burr
Cemented femur / tibia
- separate at cement-implant interface
- remove cement later
Uncemented femur / tibia
- rarely have to cut base plate from keel (carbide burr)
- can perform TT osteotomy
- stacked osteotomes
Prepare Tibia
Reason
- sets joint line
- enables flexion extension balancing
Insert trial intramedullary stem
Find IM canal
- ream until appropriate diameter
- desired length
- place trial
- set proximal cutting jigs off IM stem
Proximal tibial cut
Minimal tibial cut
- cut 1 - 2 mm off high side to preserve bone
- usually lateral side
- make resection for desired augment (5 or 10 mm) other condyle
- use jig
Insert trial tibia
Use offset as required
- ensures tibial component good fit on tibia
- tibial component not dependent on stem position
- ensure not internally rotated
- attach required augments
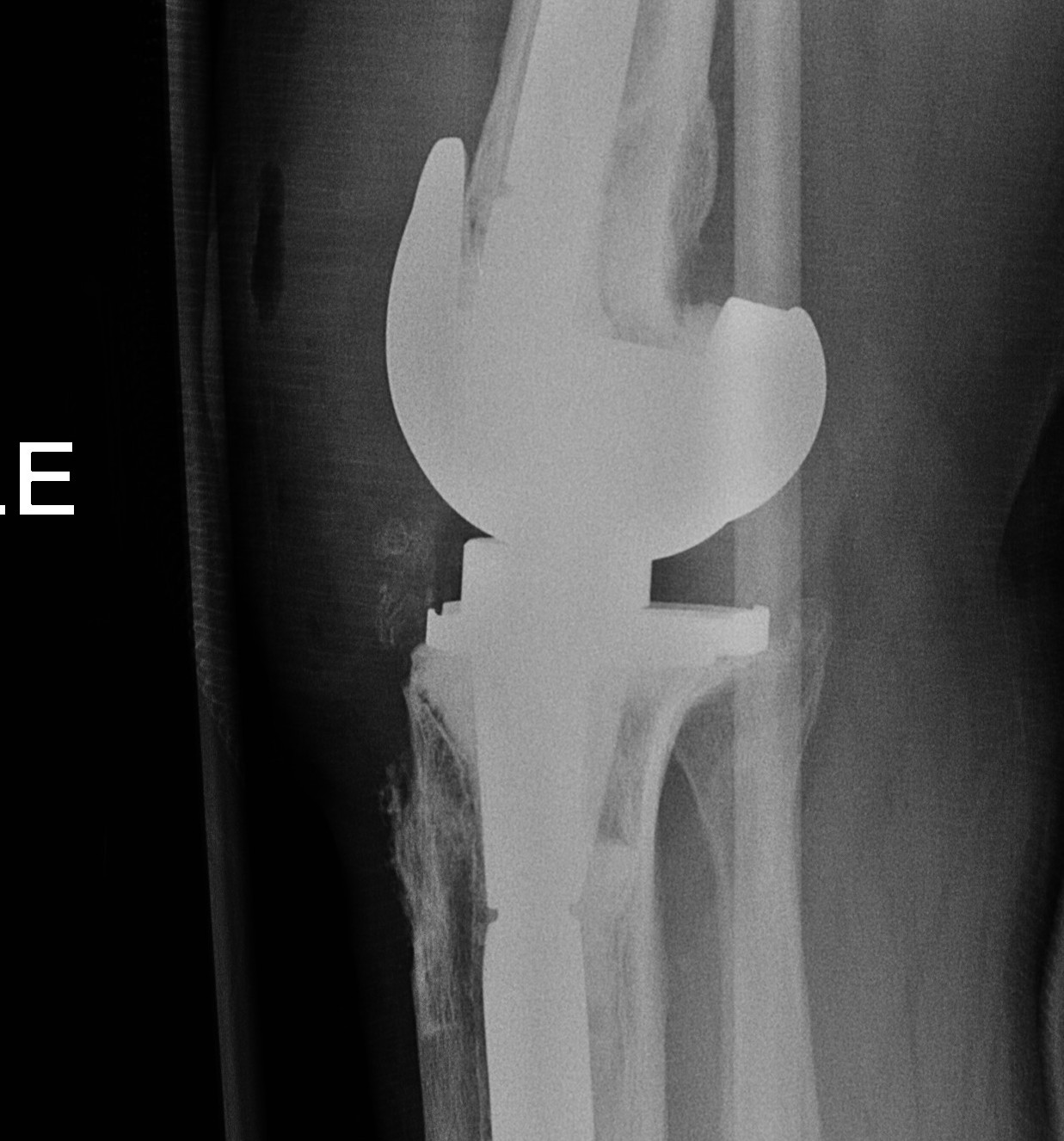
Recreate Joint line
Importance
- if rebuild tibial with augments and poly to correct joint line
- can rebuild distal and posterior femur to match


Markers
- scar from meniscal remnant
- 10 mm above fibula head
- 30 mm below medial epicondyle
- use templated distance from medial epicondyle on other knee
Restore joint line with appropriate sized poly
Prepare Femur
Insert trial intramedullary stem
Find IM canal
- entry point important
- if too posterior will flex femur
- if too anterior will extend femur
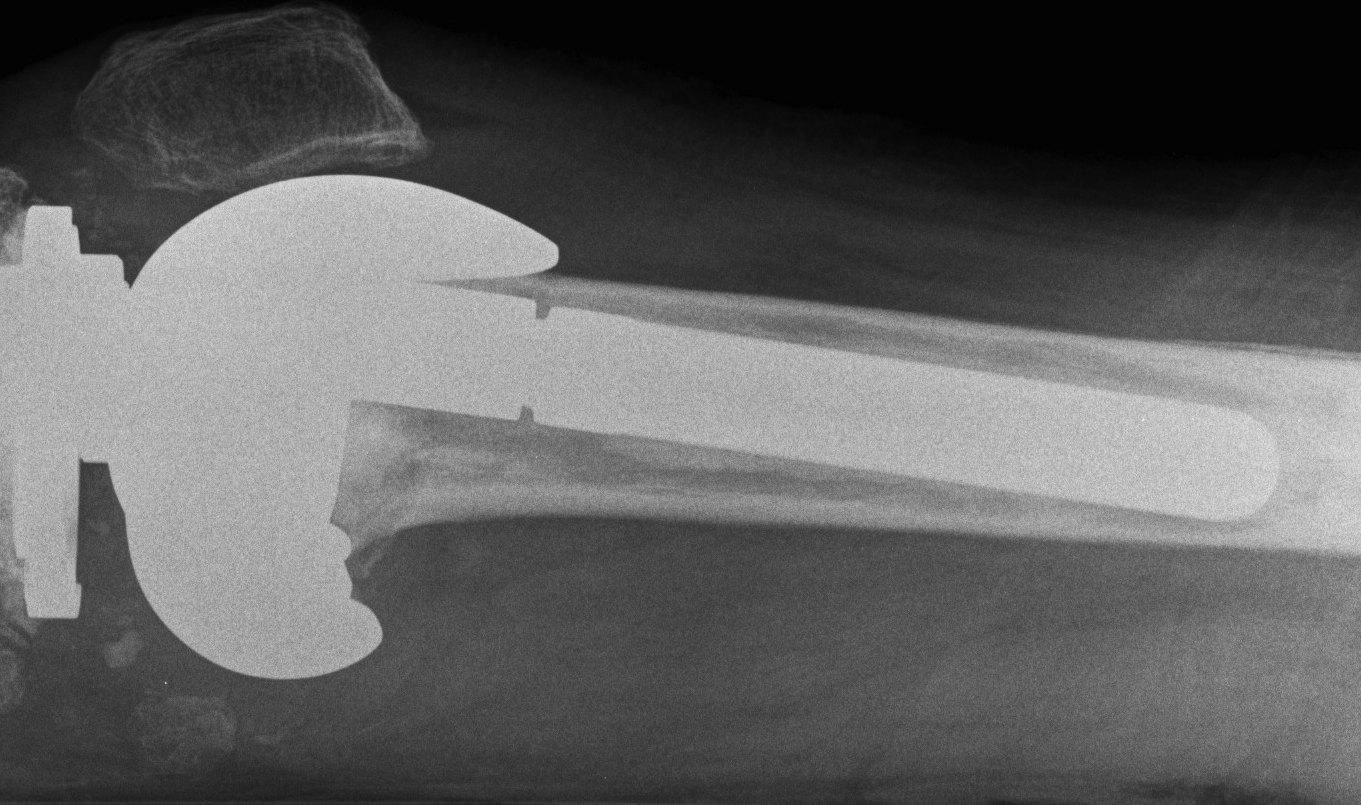
Ream until press fit
- insert desired length of stem
Distal femoral Cut
Distal cutting block on stem
- want to freshen surfaces minimally
- 1-2 mm off distal surface only
- consider distal femoral augments
- wait to trial extension gap to decide distal femoral augments
AP sizing
Posterior femoral condyles frequently deficient
- require augment posteriorly
- use anatomically sized femoral component
- template from other knee or use previous size from primary
- add augments posteriorly as
May need offset so femoral component sits on IM stem

Rotation
Trans-epicondylar axis most reliable
- posterior femoral condyles may be more deficient laterally than medially
- set correct rotation
- freshen AP and chamfer cuts
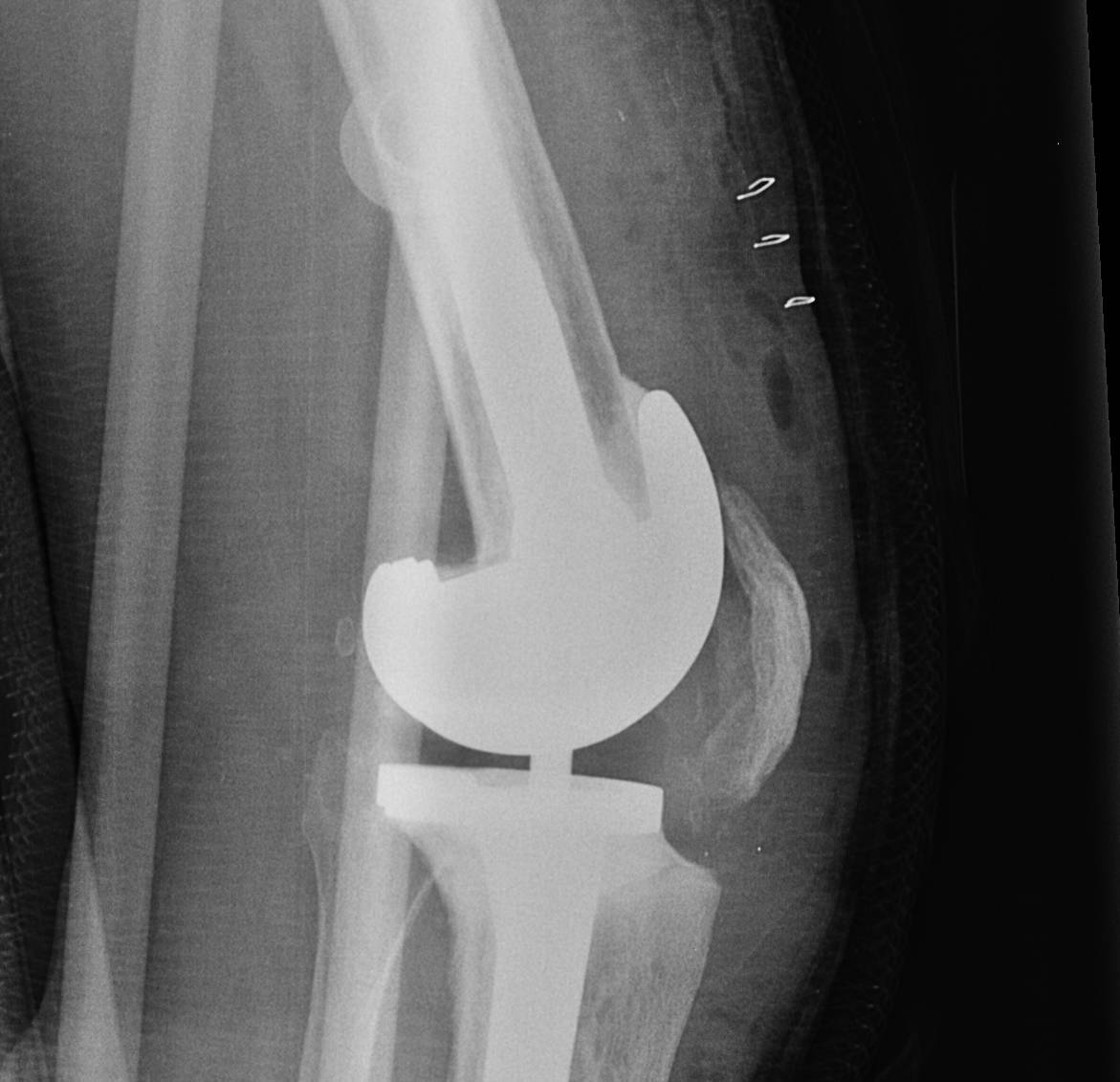
Balancing
1. Loose flexion and extension
- ensure poly thickness restores correct joint line
- increase distal and posterior femoral augments
2. Loose flexion gap
- most common
- add posterior femoral augments
- use appropriate sized femoral implant

3. Loose extension gap
- increase distal femoral augments
4. Tight flexion gap
A. Reduce femoral distal augments / femoral component size
B. Lower joint line by reducing poly thickness
- becomes loose in extension
- increase distal femoral augments
5. Tight extension gap
A. Correct joint line
- decrease distal femoral augments
B. Joint line too high
- reduce poly to joint level
- create loose flexion gap, posterior femoral augments
6. Tight flexion and extension
- reduce poly thickness
Constraint
Usually determine constraint after bone defects dealt with and flexion / extension gaps balanced
1. Collaterals Intact
Posterior stabilised sufficient

2. MCL deficient
Option A
Young patient MCL deficient
- High Post / Condylar constrained implant
- will eventually fail if don't reconstruct MCL
- young patient use CCK as internal splint and reconstruct MCL
MCL reconstruction
- achilles tendon allograft
- semitendinosus left attached distally
Option B
Rotating hinge
- elderly patient MCL deficient



3. Lateral instability
Causes
1. Femoral component malrotation
2. ITB deficient
- VVC
- brace for 3/12
3. LCL deficient
- VVC + reconstruction
- semitendinosus / lars / allograft
- find centre of rotation on femur
- pass through drill hole in fibula
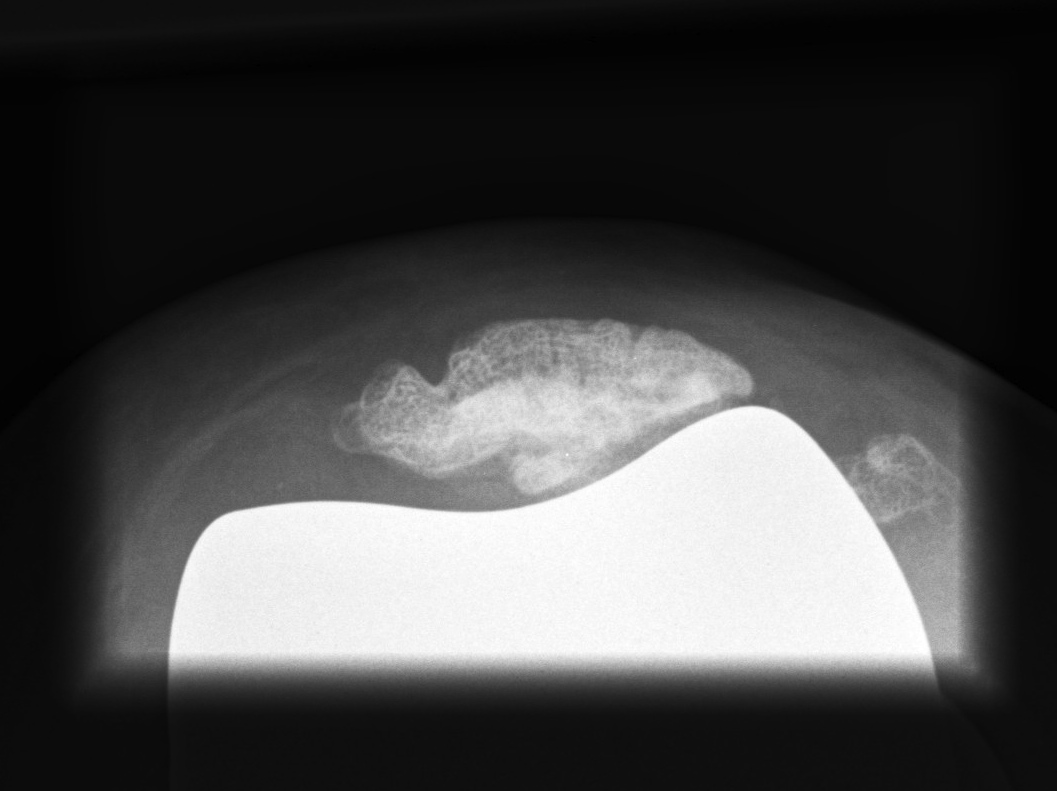
Patella
Options
1. > 10 mm bone remaining
- can resurface
2. Ignore

Patella tendon avulsion
1. Repair
- Krackow suture secured around tibial post and washer
- staples
2. Biological augmentation
- semitendinosus graft and gracilis
- achilles allograft
- LARS
3. Immobilise in extension for 6 weeks