Indications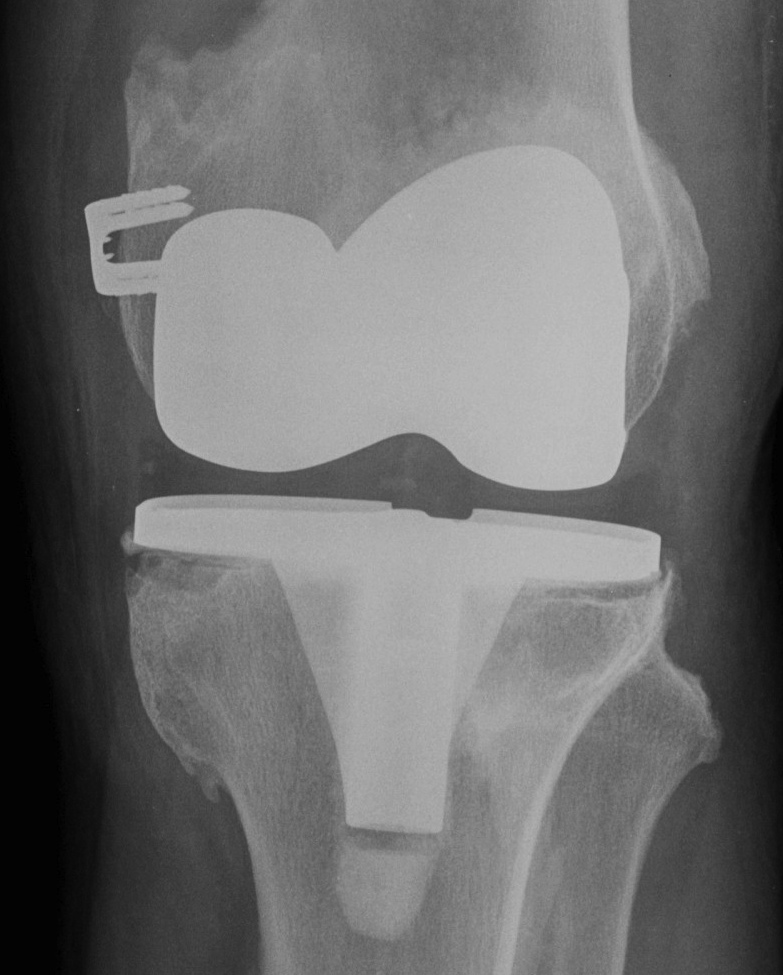
Aseptic loosening
Infection
Instability
Wear & breakage components
Fracture
Stiffness
Pain
Aims
Restoration of anatomical alignment
Restoration of joint line
Restoration of bone stock
Restoration of femoral and tibial rotation
Flexion and extension balancing
Surgical Issues
1. Exclude Infection
2. Incisions / Approach
3. Component removal
4. Bone Defects
5. Restoration of joint line
6. Balancing
7. Component Fixation / Stems
8. Constraint
9. Patella
Examination
Lower limb
- old incisions
- pulses
- sensation (Charcot neuropathy)
ROM
- need 110o flexion to remove and insert components
- otherwise will need tibial tubercle osteotomy
Stability
- LCL / MCL intact
- need VVC / hinge
Extensor Mechanism
Examine hip and back
- may be cause of referred pain
Exclude Infection
1. Clinical Findings
2. ESR & CRP
3. Bone Scan
4. Aspiration
5. Intra-op FFS
Assess Bone Stock
Causes
- secondary to osteolysis
- iatrogenic when removing components
Site
Tibial bone loss
- often medial, due to implant in varus
Femoral bone loss
- often posterior femoral condyles
Aims
Preserve all viable bone
Reconstruct deficient bone
Provide stable base for implants
AORI Classification / Andersen Orthopaedic Research Institution
T Tibial F Femoral
1 Contained Metaphyseal defect
2 Damaged Metaphysis
A One condyle
B Both
3 Deficient Metaphysis +/- collaterals / quadriceps
Template
1. Establishment of joint line essential
Allows flexion and extension balancing
X-ray contralateral knee
- measure medial epicondyle to joint line
Template same on revision knee
2. Length and diameter of stems
3. Augments
- distal and posterior femur
- proximal tibia
Order instrumentation
Previous component company specific removal gear
Cement removal instruments
Diaphyseal engaging stems, offset available
Modular metal augments
Constraint including CCK / hinges
Full component of poly thicknesses
Allograft
