
Concept
THA in dysplastic hips complicated due to anatomic abnormalities of acetabulum and femur
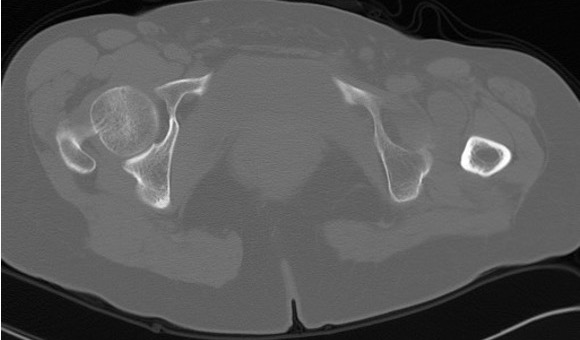
Crowe Classification
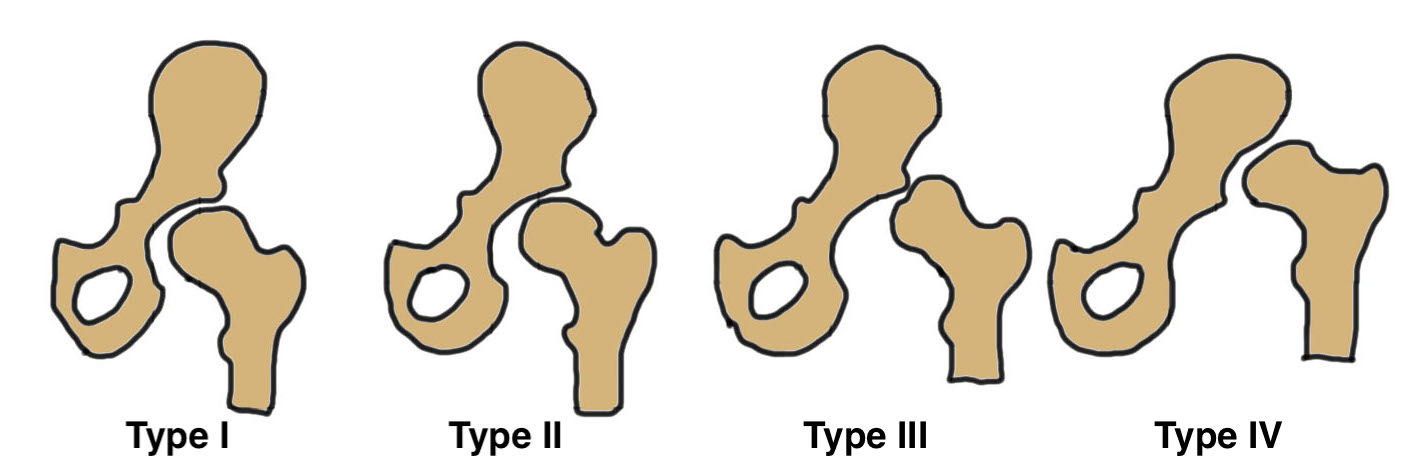
| Crowe Type | Definition |
|---|---|
| I | Subluxation < 50% vertical diameter femoral head |
| II | Subluxation 50 - 75% vertical diameter femoral head |
| III | Subluxation 75 - 100% vertical diameter femoral head |
| IV | Proximal migration of > 100% vertical diameter femoral head |


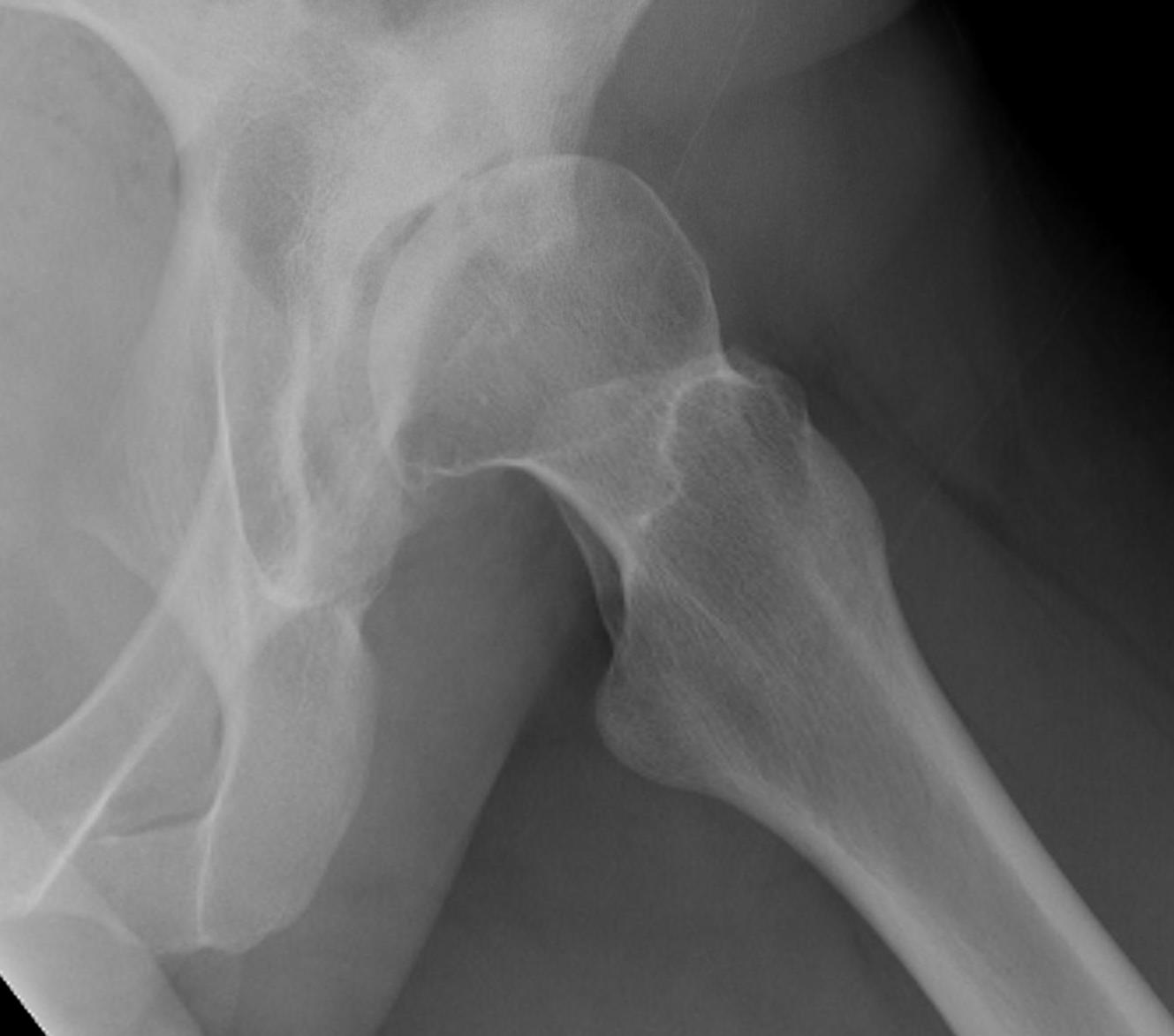
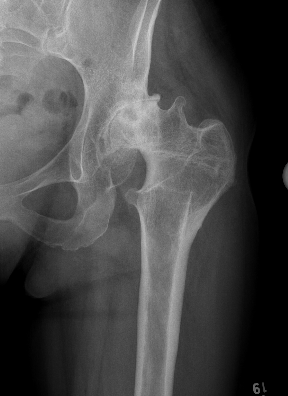
Crowe I


Crowe II


Crowe III

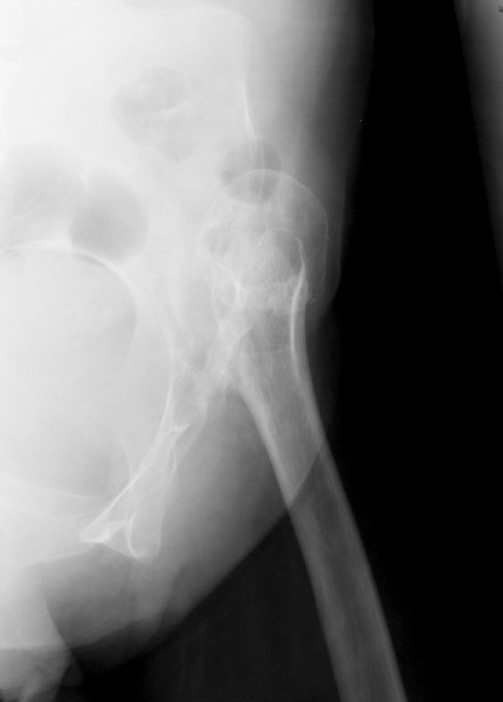

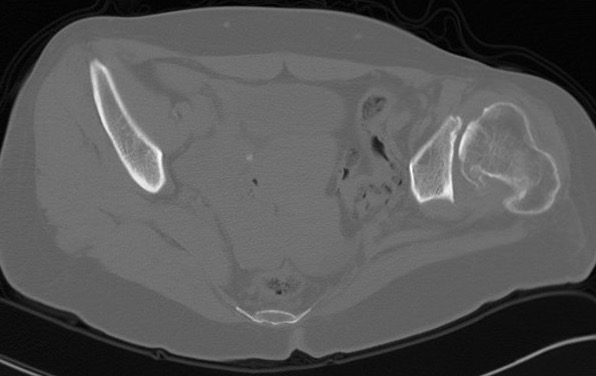
Crowe IV
Hartofilakidis Classification
| A |
|
| B |
|
| C |
|
Anatomical issues
| Soft tissues | Acetabulum | Femur | LLD |
|---|---|---|---|
| Sciatic nerve in abnormal position | Shallow | Increased anteversion | Maximum sciatic nerve can be lengthened is 3-4 cm |
| Hamstring / adductors / rectus tight | Anteverted | Valgus neck shaft angle | |
| Horizontal abductors function less efficiently |
Deficient bone stock anteriorly and superiorly |
Short offset | |
| Thick hourglass capsule | Narrow tapered femoral canal with tight isthmus | ||
| Thickened psoas tendon | Posterior displacement of the greater tuberosity |

Operative Management
Technical issues
1. Soft tissue release
- sciatic nerve in abnormal place
- capsule / psoas / adductors / abductors tight
2. Acetabulum
- restore center of rotation / bring down to true floor
- need small components
- +/- augment superolateral acetabulum
3. Femur
- small components required as femur very small
- correct excessive femoral anteversion
- restore offset as best able
- may require trochanteric slide
4. LLD
- > 4 cm need femoral subtrochanteric osteotomy
Management Algorithm
Acetabulum
| Crowe I | Crowe II / III | Crowe IV |
|---|---|---|
|
Acetabulum mildly dysplastic with good bone stock - small cup - medialize - < 30 % uncovering allowed without additional procedures |
Acetabulum - find and restore normal centre of rotation - ream medially Supero-lateral augmentation - autograft / allograft / trabecular metal augments
|
Acetabulum unaffected with good bone stock - find and restore normal center of rotation - ream medially
|
|
Small femur - small femoral stem - reduce excessive anteversion
|
Small femur - small femoral stem +/- modular - reduce excessive anteversion
|
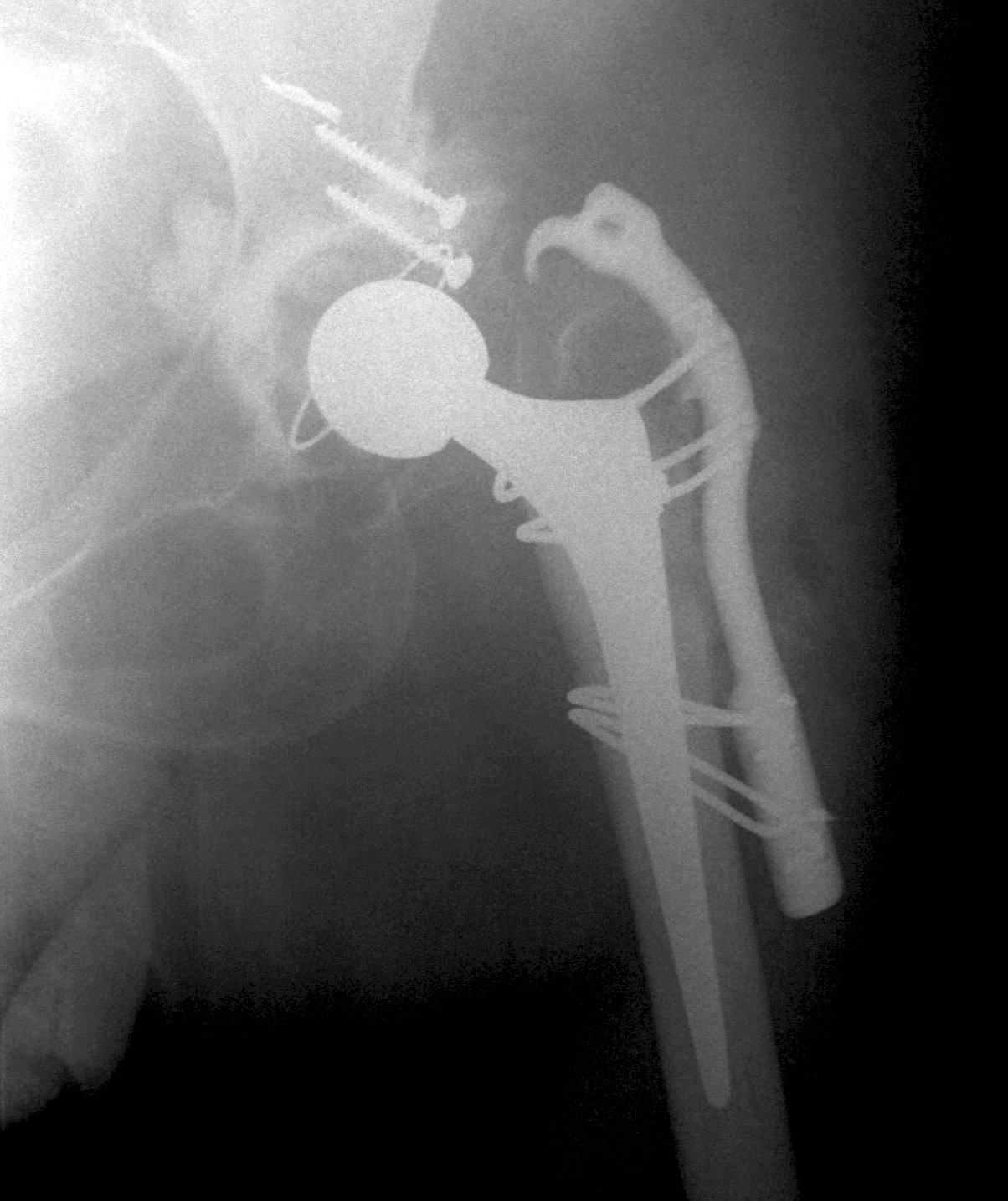
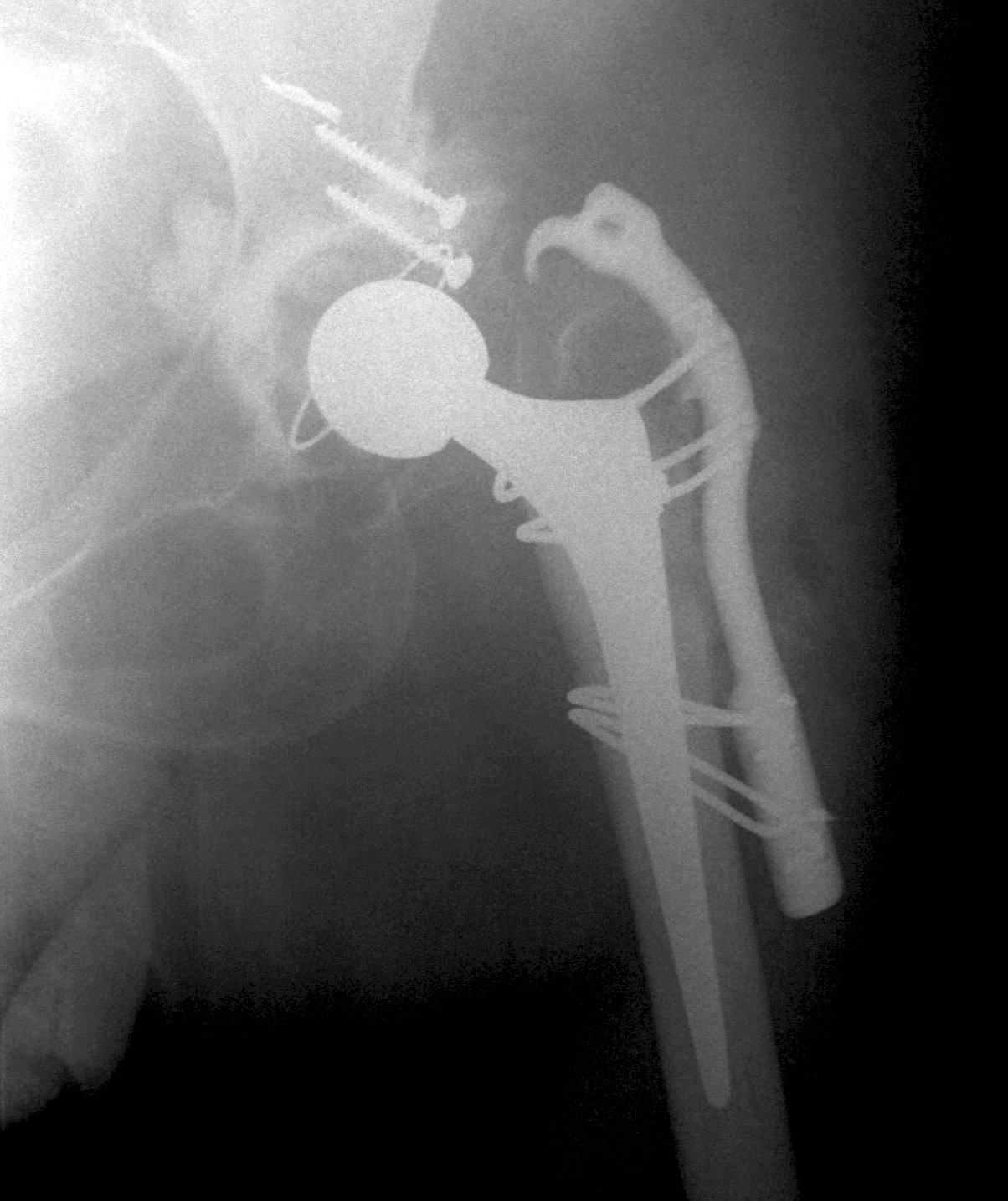
Small femur - small femoral stem +/- modular - reduce excessive anteversion > 3- 4 cm LLD - shorten femur |
|
Soft tissues - releases - consider trochanteric slide |
Soft tissues - releases - consider trochanteric slide |
Soft tissues - releases - consider trochanteric slide |
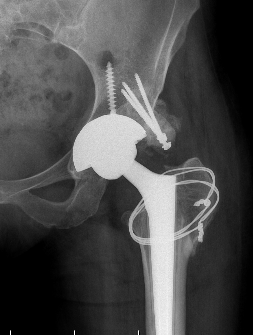
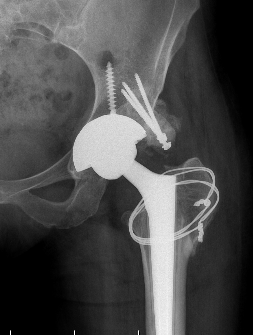
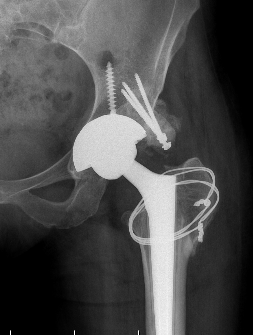
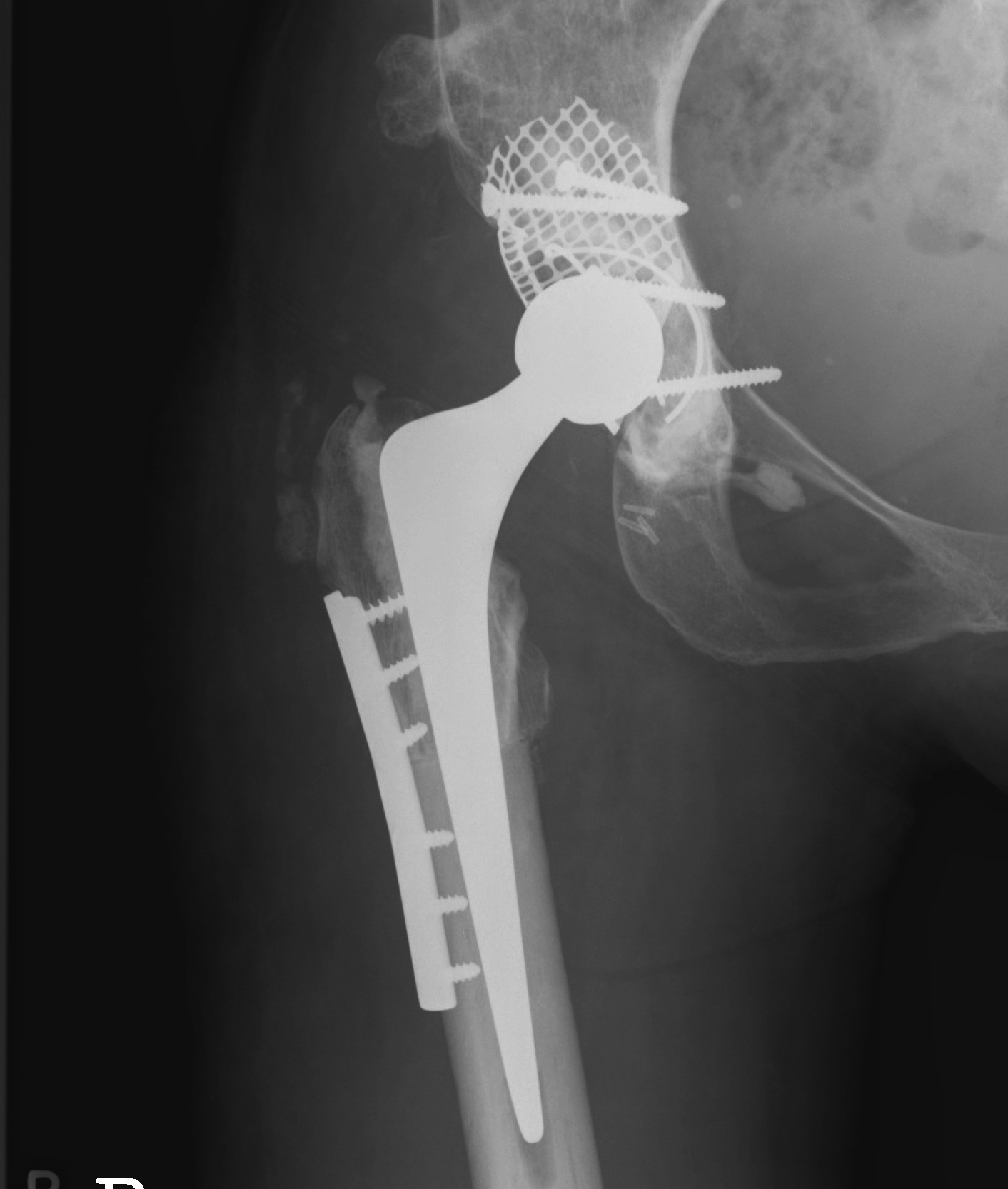
Crowe II / III: Medialize cup, superolateral femoral head augment, trochanteric slide

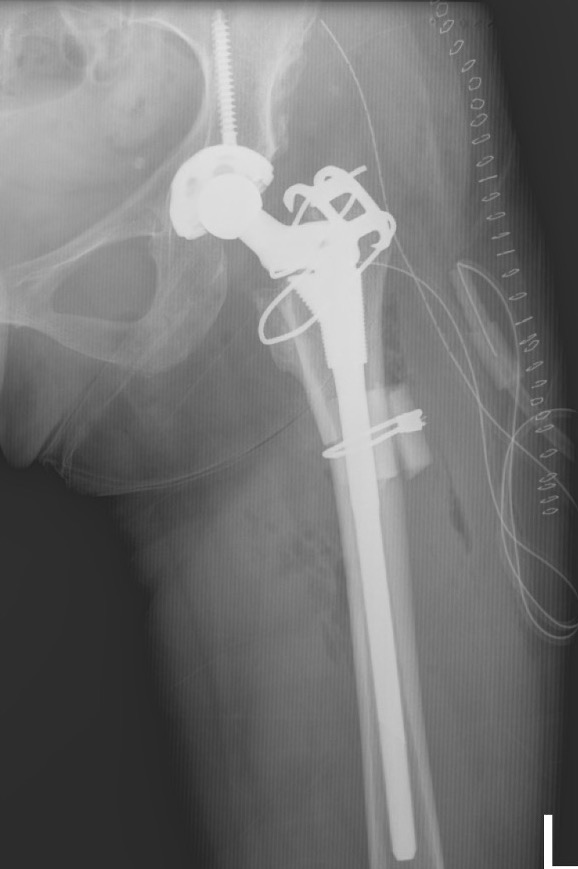
Crowe IV: Use normal acetabulum, shorten femur with subtrochanteric osteotomy + trochanteric slide
Outcomes
THA for DDH versus OA
Australian Joint Registry 2023
- 400,000 THA for OA: 20 year revision rate 8.1%
- 6,400 THA for DDH: 20 year revision rate 8.7%
Salman et al Eur J Orthop Surg Trauma 2024
- systematic review of 9 studies and 500,000 THA
- mean age THA for OA 62 and for DDH 51
- increased revision and dislocation in DDH patients
Accuracy
Wang et al Ann Transl Med 2021
- RCT of 100 DDH patients undergoing THA
- used of patient specific instrumentation increased acetabular accuracy
Soft tissues
Sciatic nerve
Identify and protect sciatic nerve at all times
- keep hip and knee flexed
- subtrochanteric osteotomy if lengthen > 3-4 cm or nerve tight
Releases
Can be difficult to reduce hip with anatomical centre of rotation
- release gluteus maximus /iliopsoas / rectus femoris / sartorius / piriformis / hamstrings
- +/- abductor slide
- +/- subtrochanteric osteotomy
Greater trochanter osteotomy / Trochanteric slide
Indication
- acetabular exposure
- retensioning abductors
- reposition abductor insertion to correct anteversion

Results
Schafer et al Arthroplasty Today 2023
- 76 greater trochanters fixed with cable plates
- nonunion rate 24%
Acetabular component
Options
1. Restore normal hip center
- may need superolateral augmentation for stability wit Crowe II/III
2. High hip center
- allows coverage by native bone and decreases need for femoral shortening
- very small acetabular component with increased risk of loosening

Anatomic hip center versus high hip center
Watts et al J Arthroplasty 2018
- 88 Crowe II/III
- reduced acetabular loosening with anatomic hip center
- systematic review of 9 studies
- high hip center: reduced operative time and blood loss
- anatomical hip center: better at restoring leg length
- systematic review
- revision rate high hip center: 2 - 9% at 7-15 years
- revision rate anatomical hip center: 0 - 6% at 6-16 years
- increased dislocation risk with high hip center
- increased neurological complication with anatomical hip centre
Restore normal hip center
A. Recreate center of rotation
Place in true acetabulum
- transverse ligament is anatomical landmark
Medialise cup
B. Need for augmentation if > 30% uncoverage of acetabular component
Options
- bulk femoral head autograft / allograft
- mesh + impaction bone graft
- reinforcement rings
- cup and cage
- tantalum cup with augments
Acetabulum Reconstruction
Structure Femoral Head Autograft
Technique
Fashion femoral head into 7 graft
- screw into place with 2 x 6.5 mm cancellous screws
- ream into inferior aspect of graft
Results
Karczewski et al Arch Orthop Trauma Surg 2023
- systematic review of femoral autograft in THA for DDH
- 26 studies and 1500 THA
- at 10 years the revision rate 8%
- mostly for loosening, dislocation rate 1%
- on xray, 11% loose and 8% resorption
Mesh + Impaction Bone Grafting
Iwase et al J Arthroplasty 2016
- impaction bone grafting for 40 THA in DDH
- 100% survival at 8 years
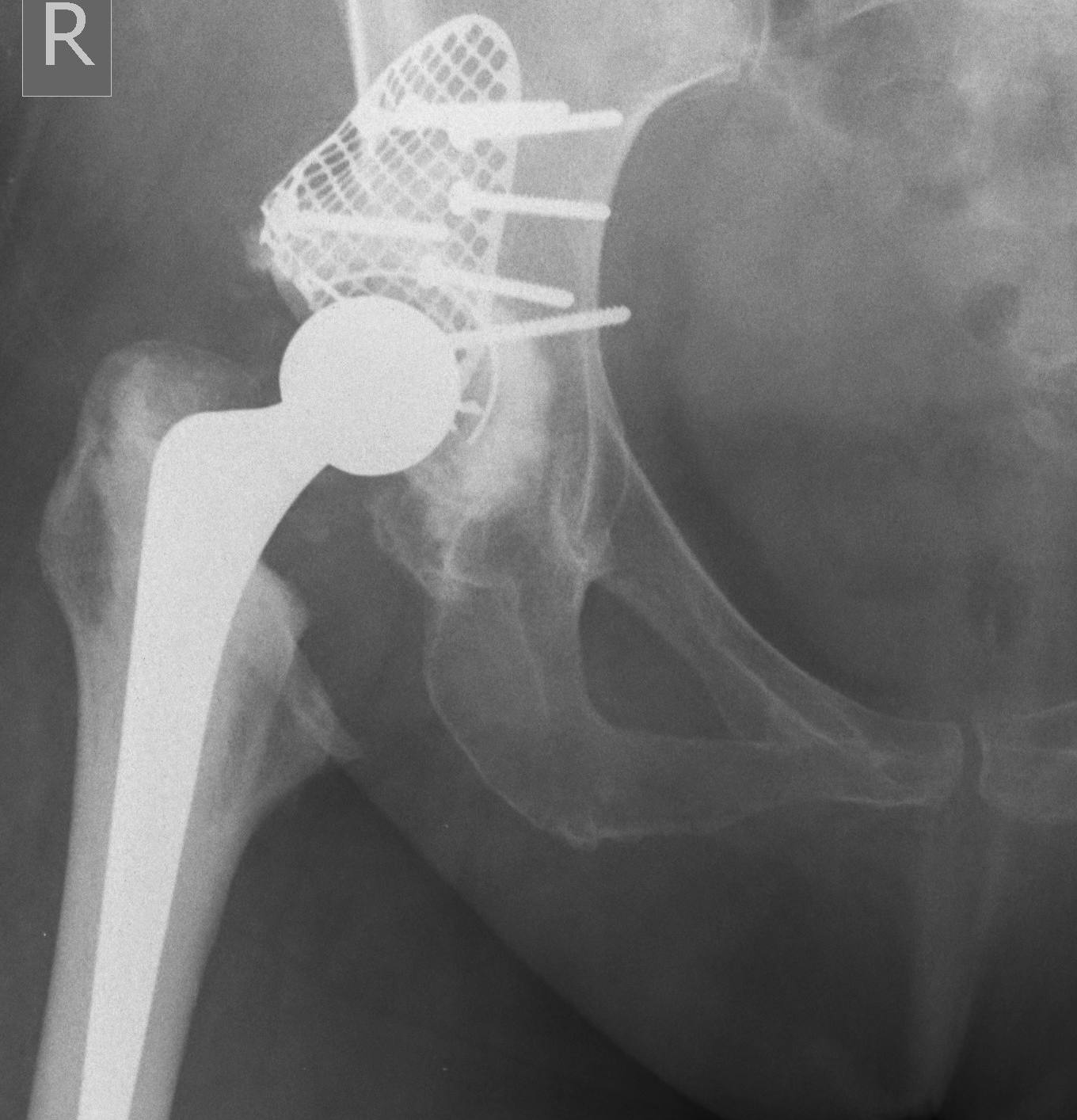
Trabecular metal cup with augments / 3D printed cups


Zimmer trabecular metal acetabular revision system
Femur
Issues
Small and narrow femoral canal
Excess anteversion
Need to shorten femur with Crowe IV
Reduce femoral anteversion
Options
1. Small cemented / uncemented components
- allows stem to be orientated independently of patients anteversion
2. Modular uncemented stems to adjust version
- can dial in required anteversion
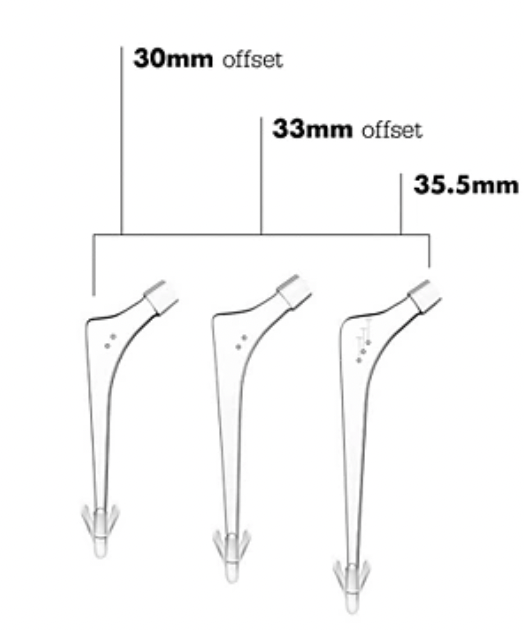
Stryker Exeter small DDH stem


Depuy S-ROM uncemented modular prosthesis
Femoral shortening / Subtrochanteric osteotomy
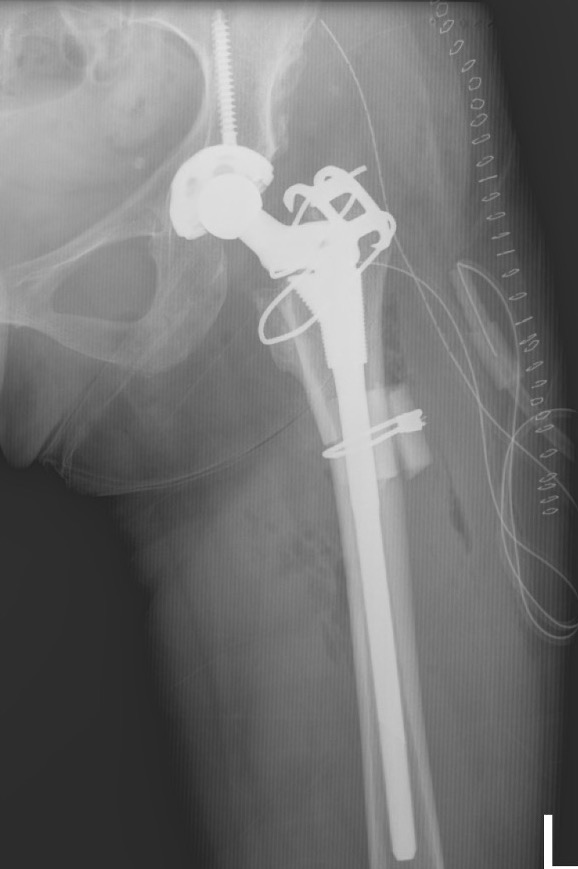
Technique
Vumedi subtrochanteric osteotomy for Crowe IV
Vumedi subtrochanteric osteotomy for Crowe IV
Options
- transverse / oblique / chevron / step cuts
Results
Li et al BMC Musculoskeletal 2014
- systematic review of trochanteric osteotomy for DDH THA
- 37 studies and 800 hips
- no difference in outcomes (nonunion, revision) for transverse versus stepcut
Wang et al J Arthroplasty 2017
- 76 Crowe IV THA
- transverse osteotomy with uncemented stem
- 1/76 nonunion
- 1 acetabulum and 1 femoral stem revised at mean 10 years
