

Indications
Severe lower back pain - most common indication
Ipsilateral knee pain
Contralateral hip pain
Malposition - especially abduction
Degenerative scoliosis post hip arthrodesis
Issues
Abductors
- if intact will have atrophied
- risk of abnormal gait / trendelenberg gait post surgery
Leg length discrepancy
Complex surgery
- restore anatomical hip center
- significant complications
Examination
LLD
- difficult to assess given flexed position of hip
Assessment abductor function
- palpation whilst asking patient to contract
- MRI
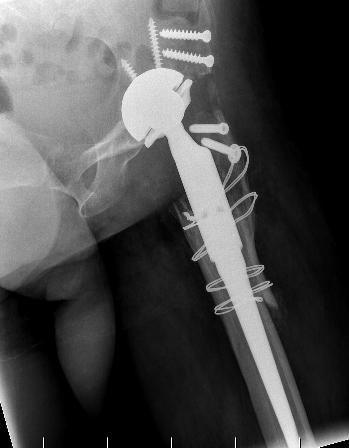
Technique
Surgical technique PDF Hip Conversion Robotic Assistance
Surgical technique PDF Hip Conversion image less navigation
Youtube surgical technique Hip Conversion image less navigation
Difficulty prepping & draping
Exposure
- identify and protect sciatic nerve
- perform GT osteotomy / trochanteric slide
- may require adductor & psoas tenotomy
Neck osteotomy
- can be difficult to identify landmarks
- can damage acetabulum with saw
Identification of acetabulum and restoration of anatomical hip center
- normal landmarks not identifiable
- need to establish correct position and depth
- have to ream away femoral head
- consider image less navigation / CT guidance / robotic guidance
Restoration of leg length
- maximum 4cm lengthening




Results
Survival
- 208 hips converted at average 51 years
- 83% good to excellent function
- 96% 10 year survival
- 90% 15 year survival
- 15 nerve palsies
Outcomes
- fusion takedown in 23 hips with 15 year follow up
- average improvement in Harris hip score 30 points
- average hip ROM 30 degrees
- back pain decreased in 62%
- knee pain decreased in 42%
Complications
Jauregui et al Int Orthop 2017
- systematic review of 27 studies and 1,100 conversions fusion to THA
- infection 5%
- instability 3%
- loosening 6%
- nerve injury 5%
- abductor complications 13%
Ayekoloye et al Bone Joint J 2021
- 39 hip fusion conversion to THA
- 70% required walking aid postoperatively
- 5% sciatic nerve injury
- 10% had significant HO required excision
