Pelvic hemorrhage
Mortality
Constantini et al J Trauma Acute Care Surg 2016
- multi-centred prospective study of 1339 patients with pelvic fractures at Level 1 trauma centers
- overall mortality 9%
- pelvic trauma with shock has 30% mortality
- 44 open pelvic fractures
- overall mortality 45%
- concurrent intra-abdominal injury 89% mortality
- pelvic sepsis 60% mortality
EMST / ATLS principles
Blood transfusion protocols
1:1:1 Plasma / Platelets / RBC
Transexamic acid
Loading dose 1g over 10 min then infusion of 1g over 8 h
Abdominal FAST scan to identify intra-abdominal bleeding
Rectal and vaginal examination
Patients in persistent shock despite blood transfusion (systolic 70 - 80 mmHg) go to operating room
Provisional Stabilization in the Emergency Room
Concept
Reduce pelvic volume and stabilize pelvic ring
Options
Sheet / Pelvic Binder/ C-clamp
Results
- 207 patients treated with sheet (16%) v pelvic binder (15%) v C-clamp (69%)
- higher incidence of lethal bleeding with sheet (23%) v pelvic binder (4%) v C clamp (8%)
- compared 40 patients with type C fractures with no stabilization v pelvic binder v C-clamp
- shorter time to application with pelvic binder
- no evidence of advantage of C-clamp over pelvic binder
- use of C-clamp resulted in 5 fold increase infection for subsequent SI joint screws
Pelvic binder
Simple, easy to use
Apply over greater trochanter




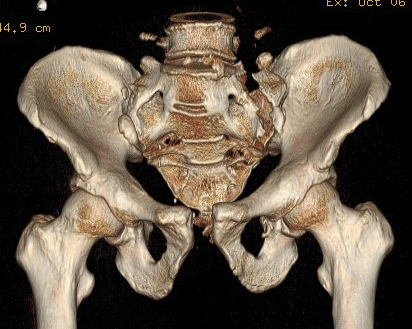
APC fracture pre- and post binder (note improper position cranial to trochanters)
C clamp
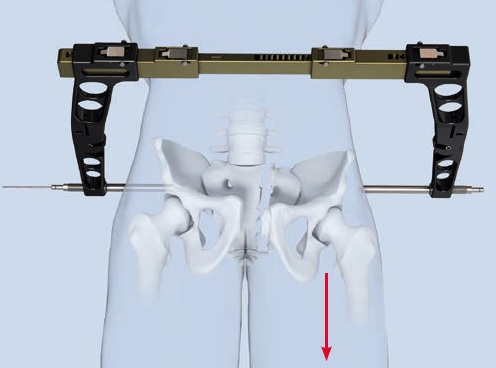
Contra-indications
Contra-indicated in iliac wing fracture / can over compression in cases with sacral comminution
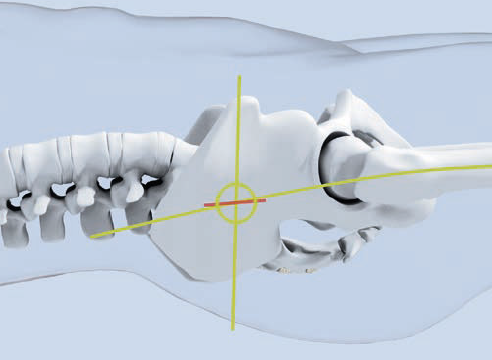
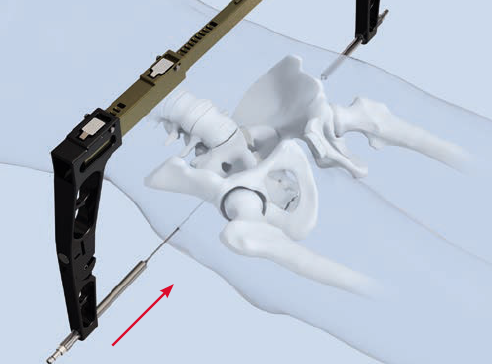
Technique
Synthes surgical technique PDF
Entry point of steinmann pins
- intersection of 2 lines
- line parallel with femur / line back from ASIS
Management of hemodynamically unstable pelvic fractures
Sources of hemorrhage
Arterial bleeders 15%
Abboud et al BMC Emerg Med 2021
- CTa of 127 consecutive pelvic fractures
- 12% had intra-pelvic arterial bleeders
- most common: obturator artery / superior gluteal / inferior gluteal arteries
- others: internal iliac / internal pudendal / fifth lumbar / lateral sacral / ilio-lumbar
- APC > Vertical shear > LC
Venous bleeding 85%
Presacral or lumbar venous plexus
Fracture site
Options
External fixation + extra-peritoneal pelvic packing
Pelvic angiography + embolisation
Pelvic packing versus Angiography
In the hemodynamically unstable patient with a bleeding pelvic fracture
- early pelvic packing and external fixation
- +/- subsequent embolization as needed
- RCT of 56 patients with hemodynamically unstable pelvic ring fractures
- pelvic angiography (ANGIO) versus retroperitoneal pelvic packing (PACK)
- median time to ANGIO was 102 minutes versus 77 minutes to PACK
- 9/27 (33%) ANGIO patients required packing for persistent bleeding
- 6/29 (21%) in the PACK group required angio for persistent bleeding
- 2 patients in ANGIO group died from exsanguination
- 0 patients in PACK group died from exsanguination
Chiara et al World J Emerg Surg 2017
- 78 patients with hemodynamically unstable pelvic fractures where pelvic was major source of bleeding
- extra-peritoneal packing reduced mortality from 50% to 20%
- hemodynamically unstable pelvic fractures
- treated with angiography versus packing +/- subsequent angiography as needed
- mortality 70% in ANGIO group versus 36% in PACK and subsequent angio group
Li et al J Orthop Traumatol 2022
- meta-analysis of packing v angiography
- 8 studies and 480 patients
- packing thought to reduced mortality and transfusion
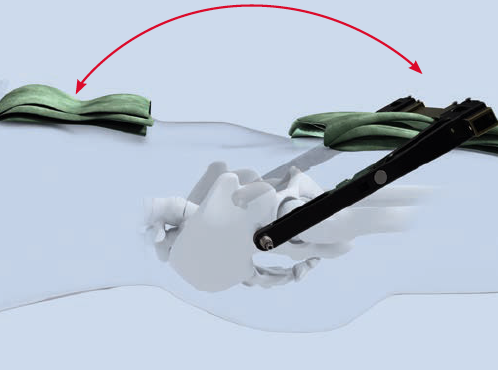
Retro-peritoneal packing + external fixation
Pelvic packing
Vumedi video of peritoneal packing
Packs need to be removed at 48 hours due to infection risk
Ensure bladder decompressed with foley catheter
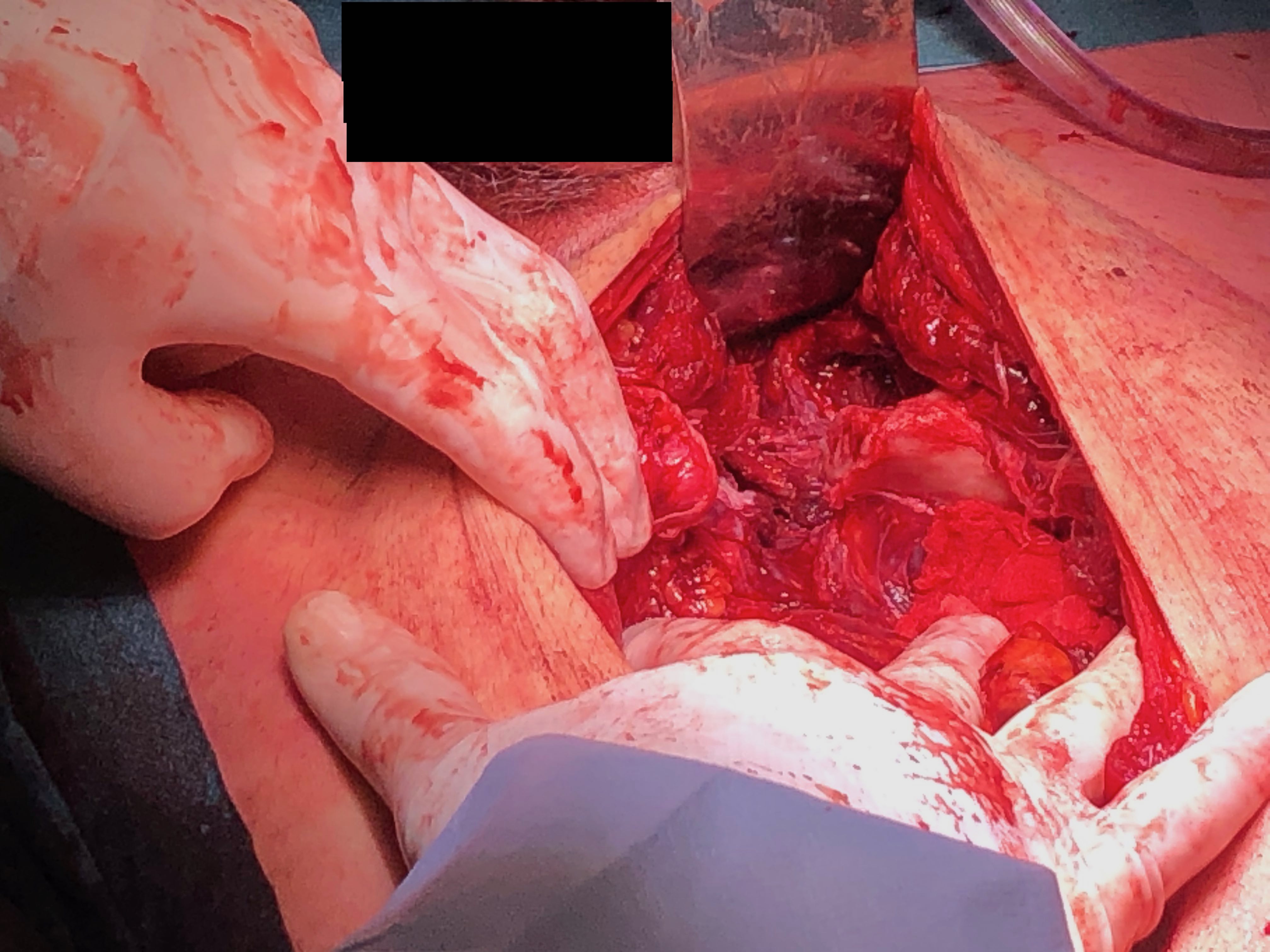
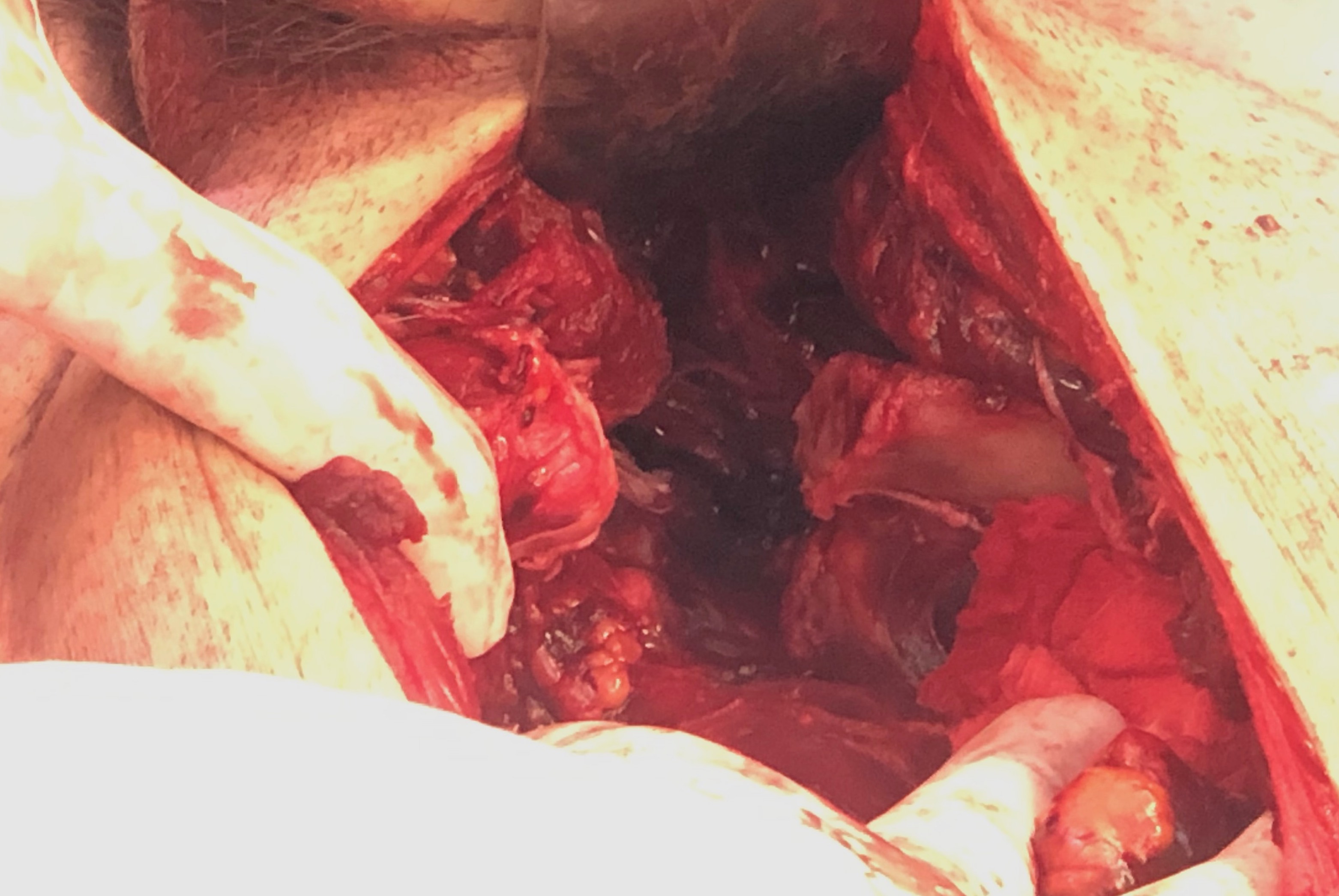
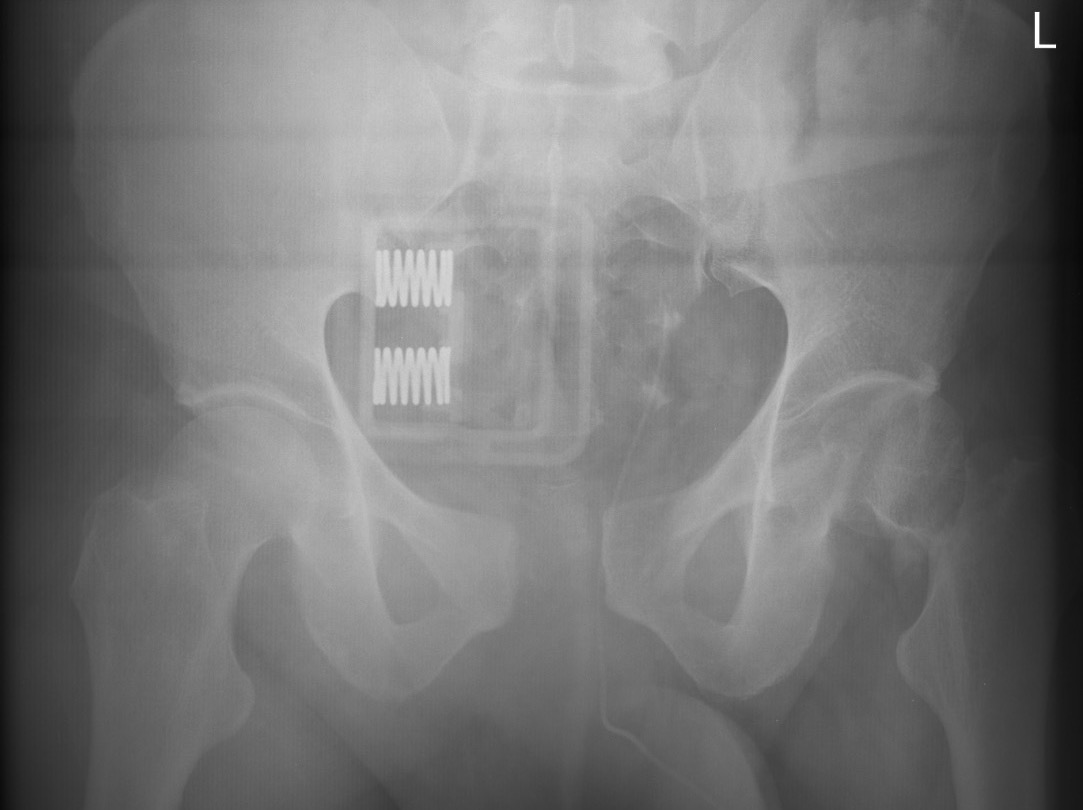
Retroperitoneal packing in unstable patient with pubic diastasis and pelvic bleeding


External fixation technique
Indications
Hemodynamically unstable patients
Anterior pelvic ring injuries
Can be definitive treatment for those with open or visceral injuries precluding anterior internal fixation
Options
Iliac crest frame
Supra-acetabular frame
- pins in AIIS
- requires fluoroscopy
Technique iliac crest
Vumedi video sawbones iliac crest external fixation
Vumedi video intra-operative iliac crest external fixation
Technique supra acetabular
AO foundation pelvic supra acetabular external fixation technique
Vumedi video supra acetabular external fixation