Nonoperative
< 2.5 cm diastasis
Stable
Sacrospinous ligament intact
EUA of APC-1 injury demonstrating < 2.5 cm instability
Instability
Sagi et al J Orthop Trauma 2011
- EUA of 14 APC-1 fractures
- 50% deemed unstable and to actually be APC-2 fractures
Operative
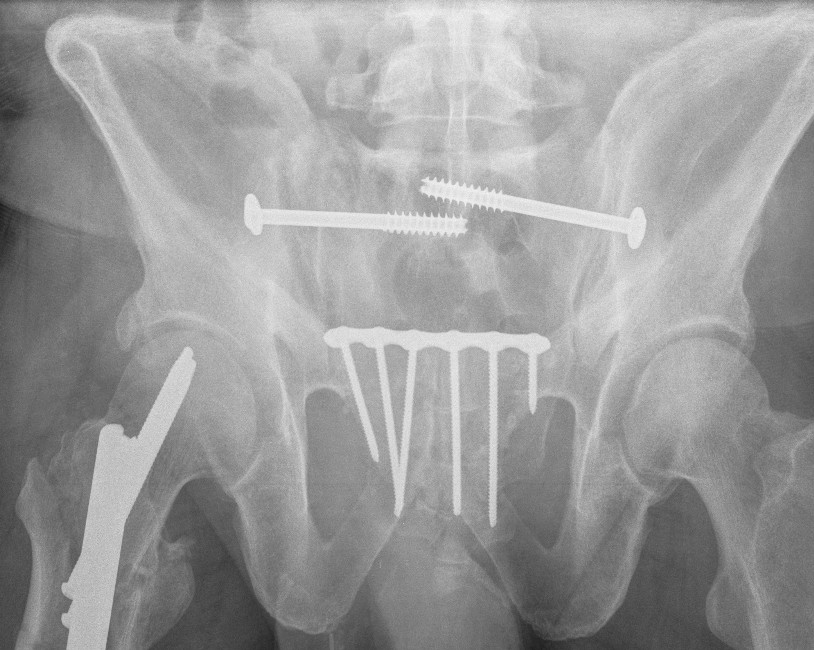
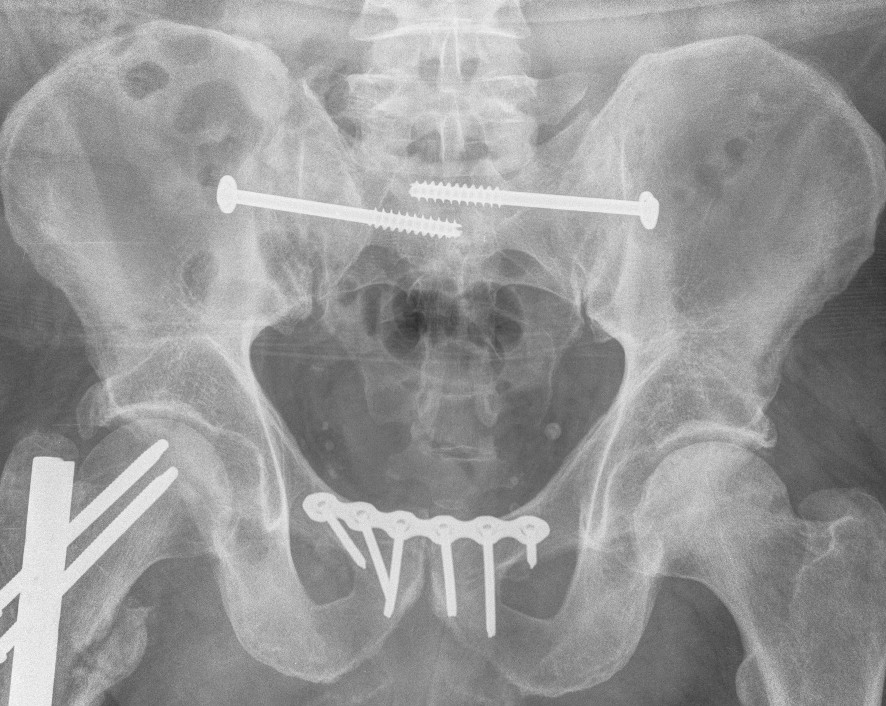
1. Anterior pelvic ring injury > 2.5 cm pubic diastasis
- anterior plate through Pfannenstiel incision
- anterior external fixation
2. Posterior SI joint disruption
- reduction and posterior stabilisation
- usually with SI screws
- if comminuted may need sacro-iliac plates (anterior or posterior)

Pfannenstiel approach / Plating Pubic Symphysis
Vumedi video pubic symphysis plate
AO surgery reference pubic symphysis plate
Technique
Set up
- supine on radiolucent table
- foley catheter to decompress bladder
Incision 2 cm above pubis
- through fat and fascia
- split linea alba between rectus
- identify and protect bladder

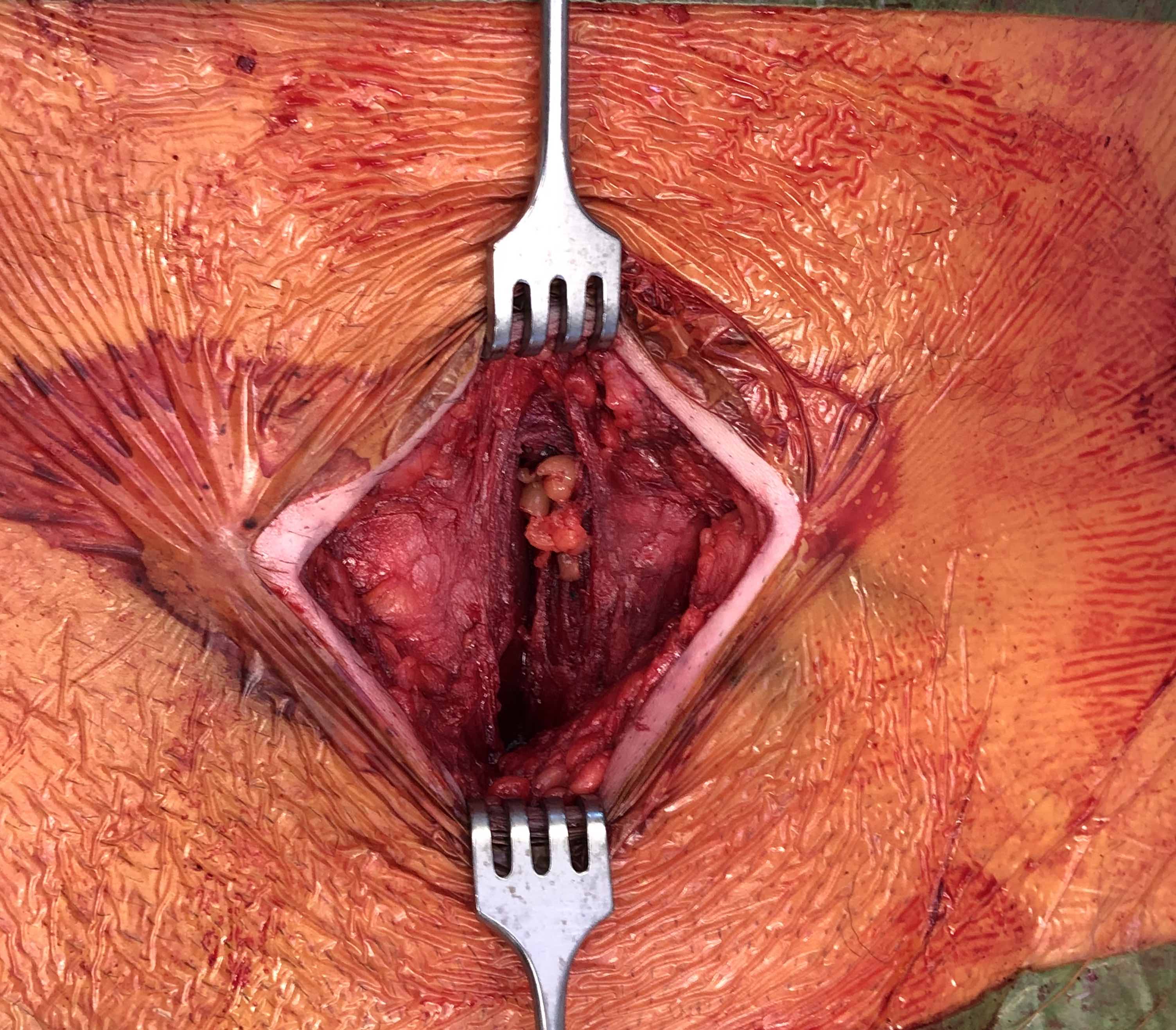
Incision 2 cm above pubis Identify linea alba and develop plane between rectus
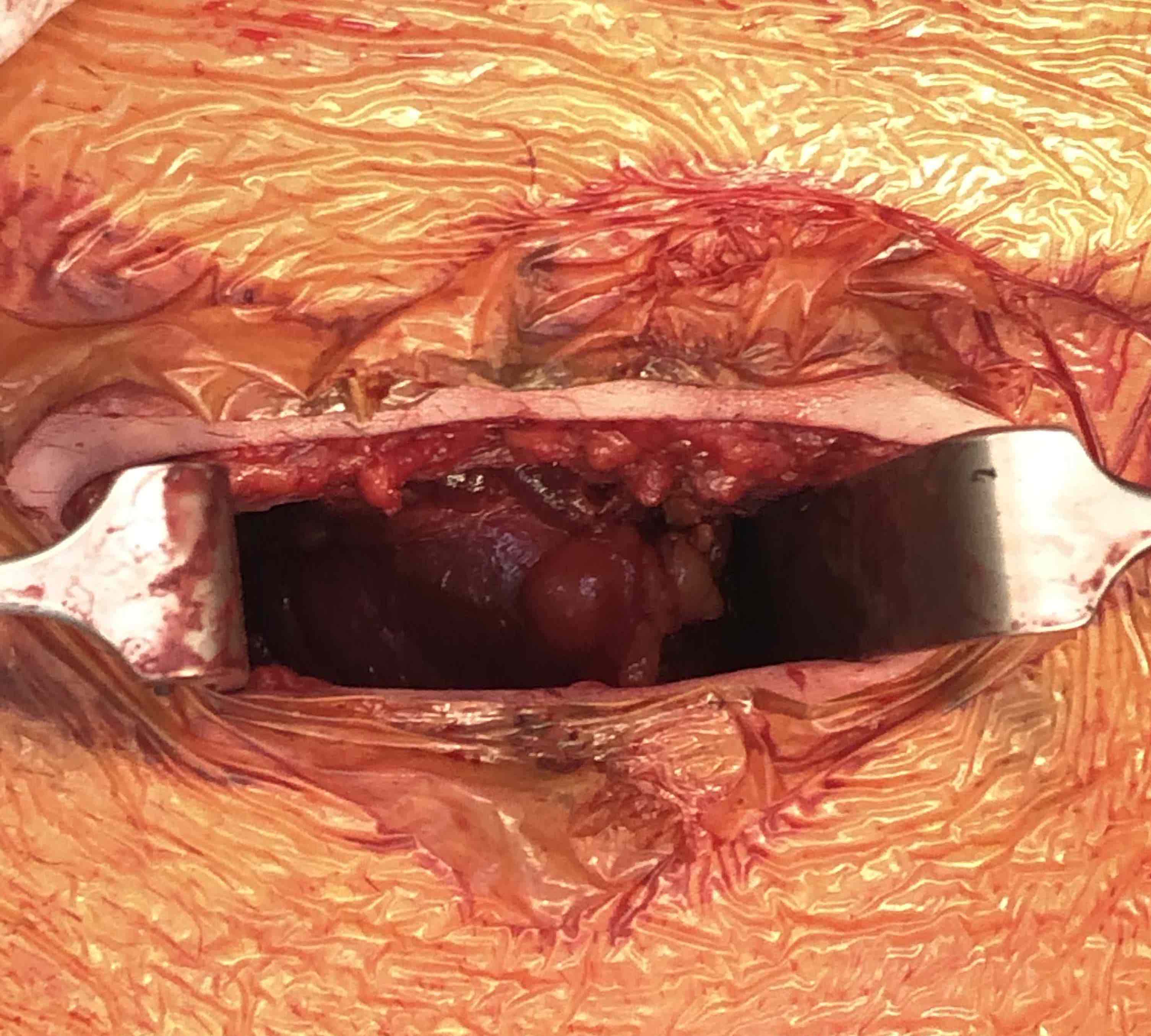
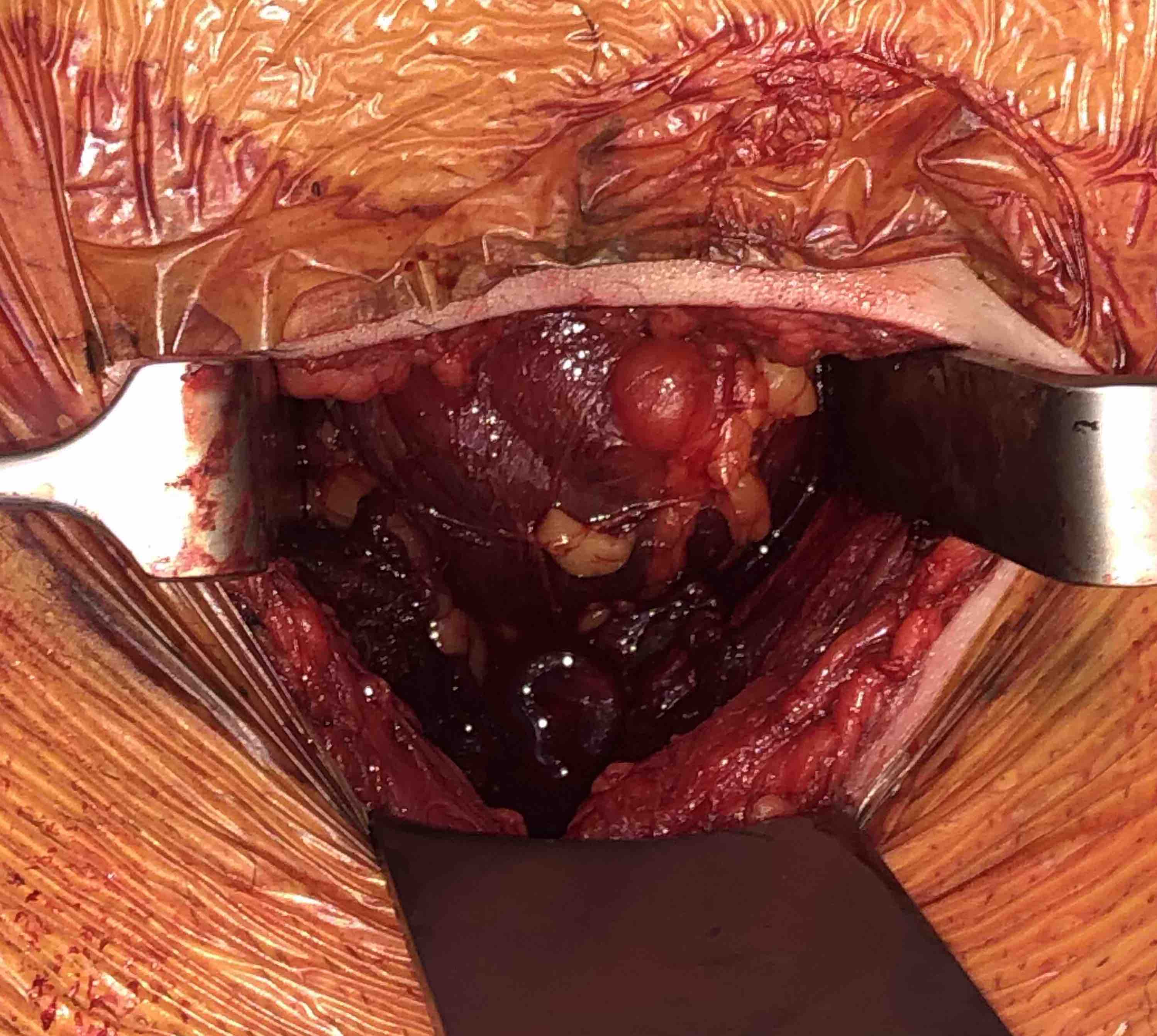
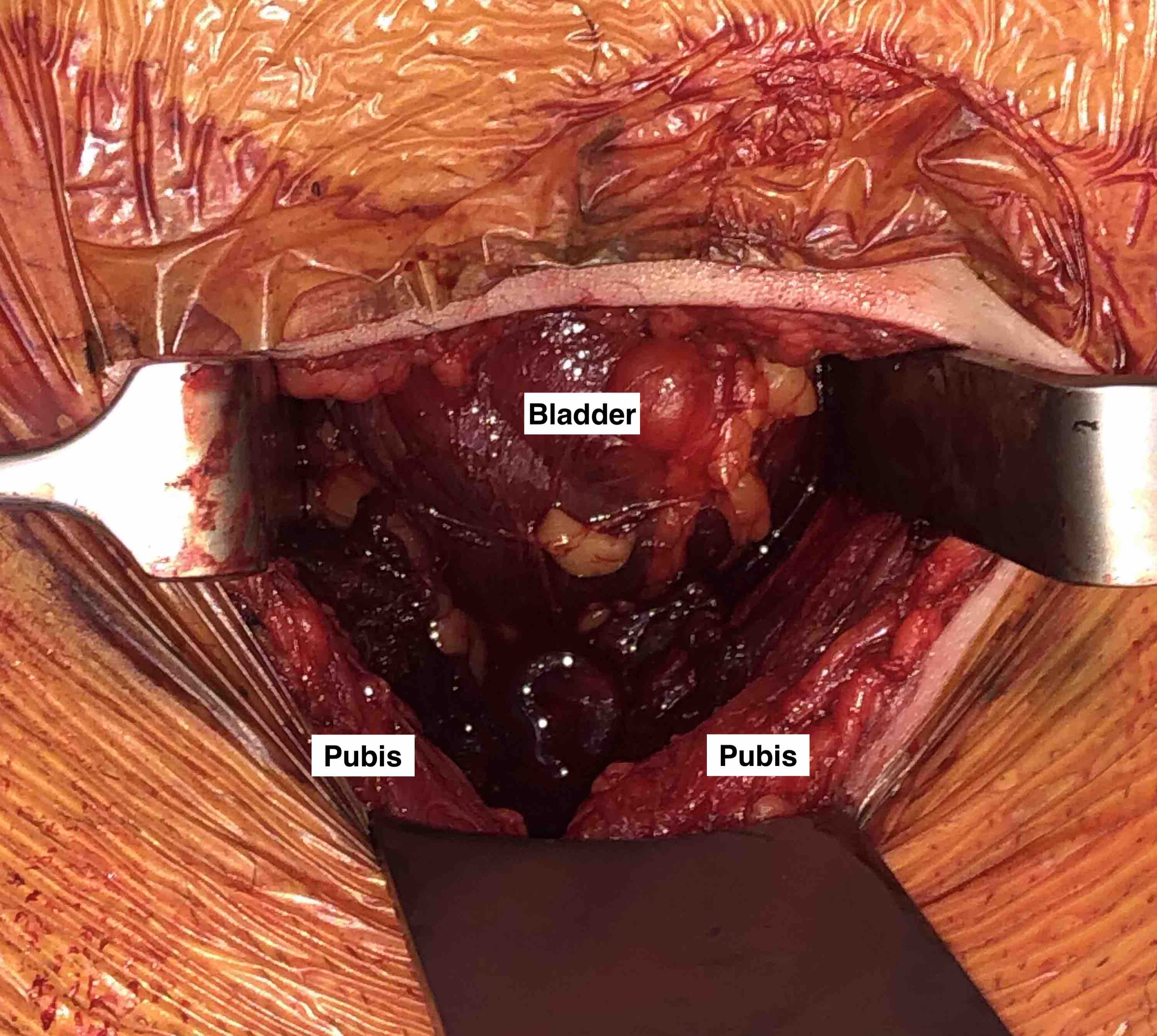
Identify and protect bladder posteriorly
Reduction techniques
- during the reduction care must be taken to avoid trapping bladder or urethra in the symphysis when closing the clamp
- assistant may apply pressure over each iliac crest or an external fixator can be applied
- large pointed reduction clamp can be placed onto each pubic tubercle or through holes drilled in the bone
- expose the medial obturator foramen and application of pelvic reduction forceps thru the medial aspect of the foramen
Superiorly applied plate
- pelvic reconstruction plate

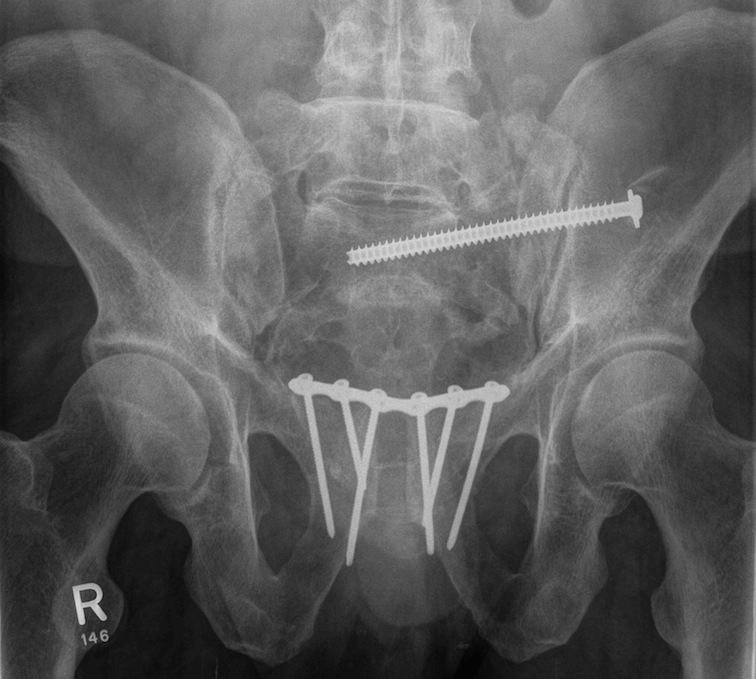
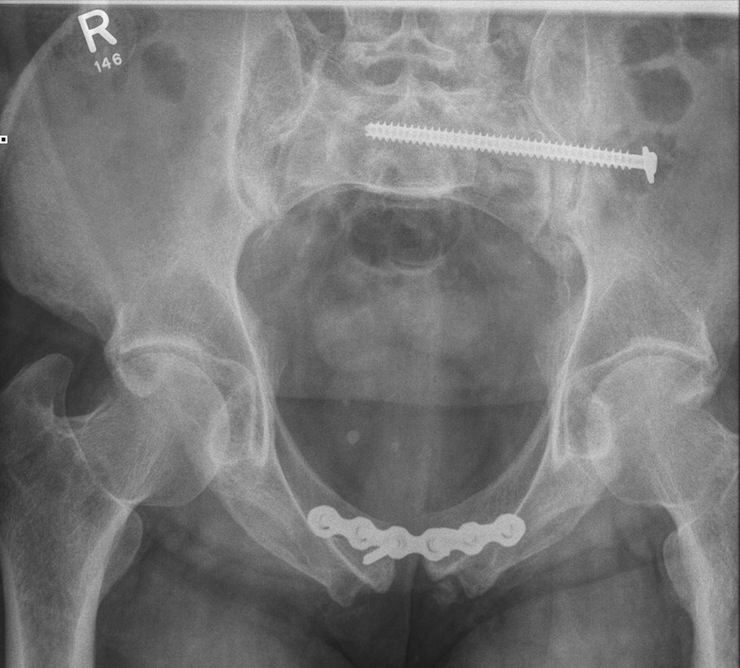
Post-operative XRs: AP, outlet and inlet views
Outcomes of pubic symphysis plating
- 148 patients with pubic symphysis plating
- hardware breakage in 63 patients
- 60% of these patients asymptomatic
- 5 patients required revision for failure of fixation or symptomatic instability
Tseng et al Arch Orthop Trauma Surg 2022
- 9 patients with implant failure including plate breakage
- no difference in functional outcomes
- 58 patients with APC fractures treated with anterior plate versus anterior external fixation
- Majeed score of 70 with external fixation
- Majeed score of 79 with plate
- non significant
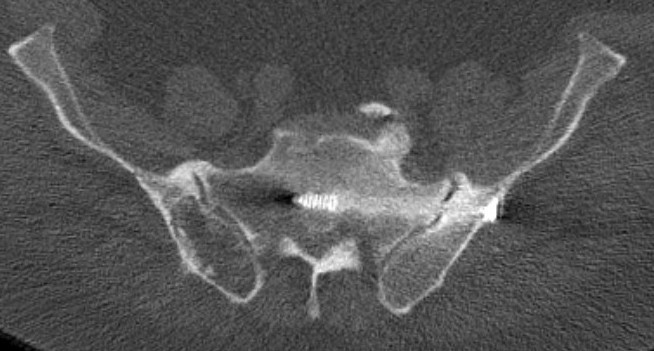
Sacro-iliac screws
Vumedi video percutaneous SI screws
AO surgery reference percutaneous SI screw
Technique
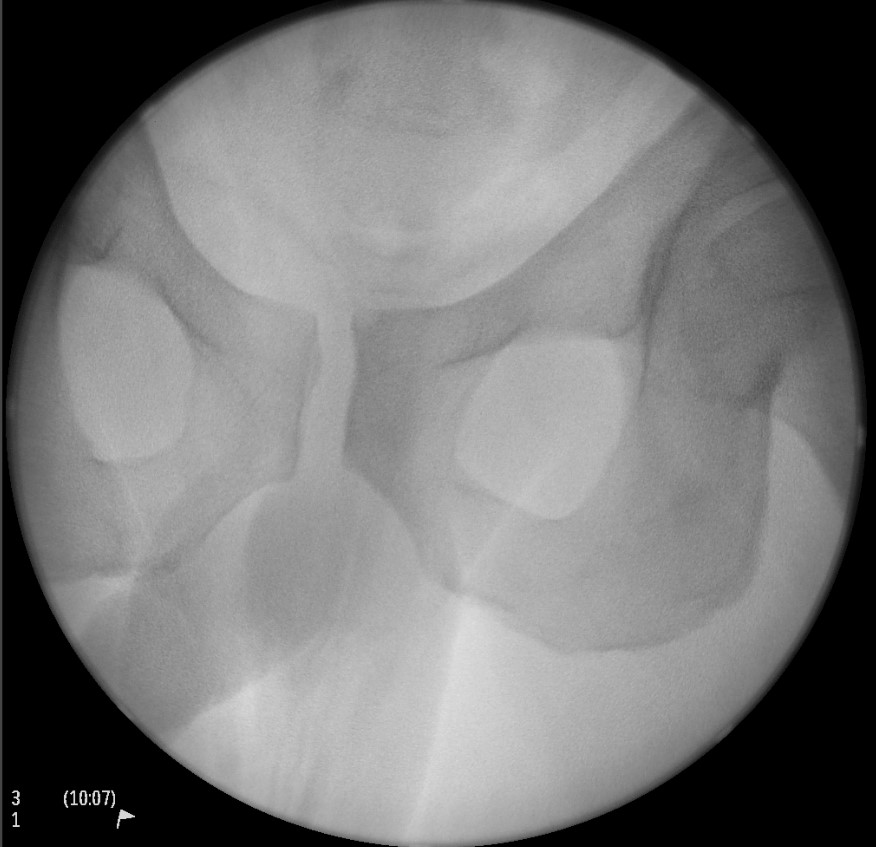
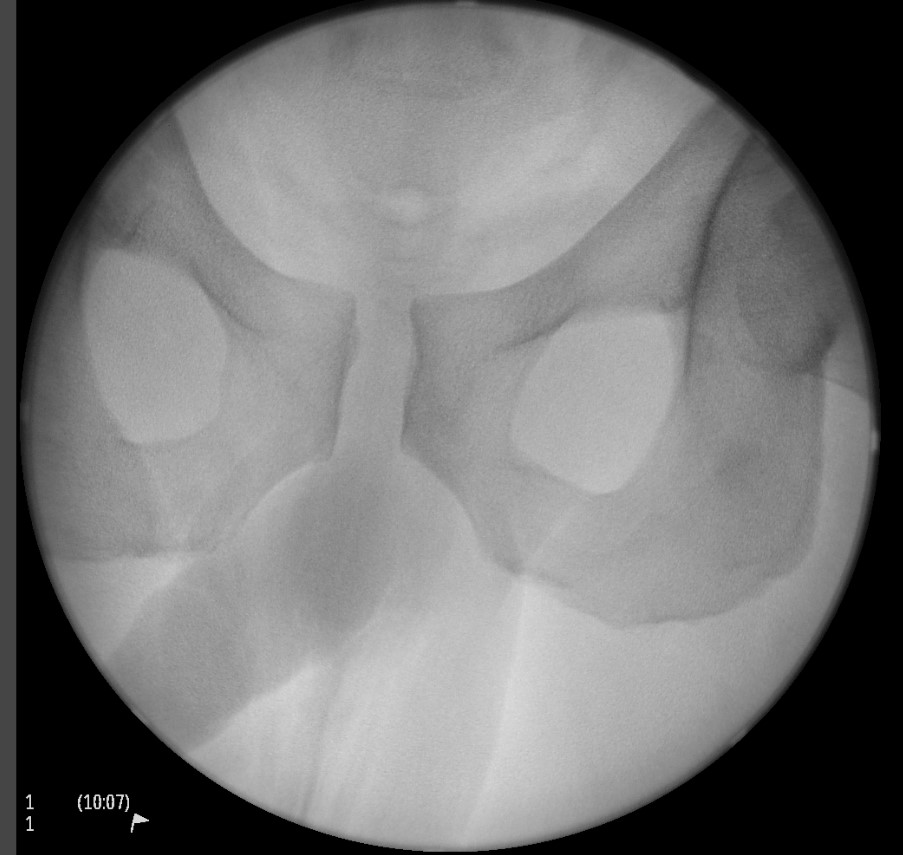
Radiolucent table with image intensifier
- 45o cephalad and caudal / inlet and outlet views
Must reduce SI joint
- reduce vertically with traction on limb / outlet view
- reduce AP usually via anterior plate or external fixation / inlet view
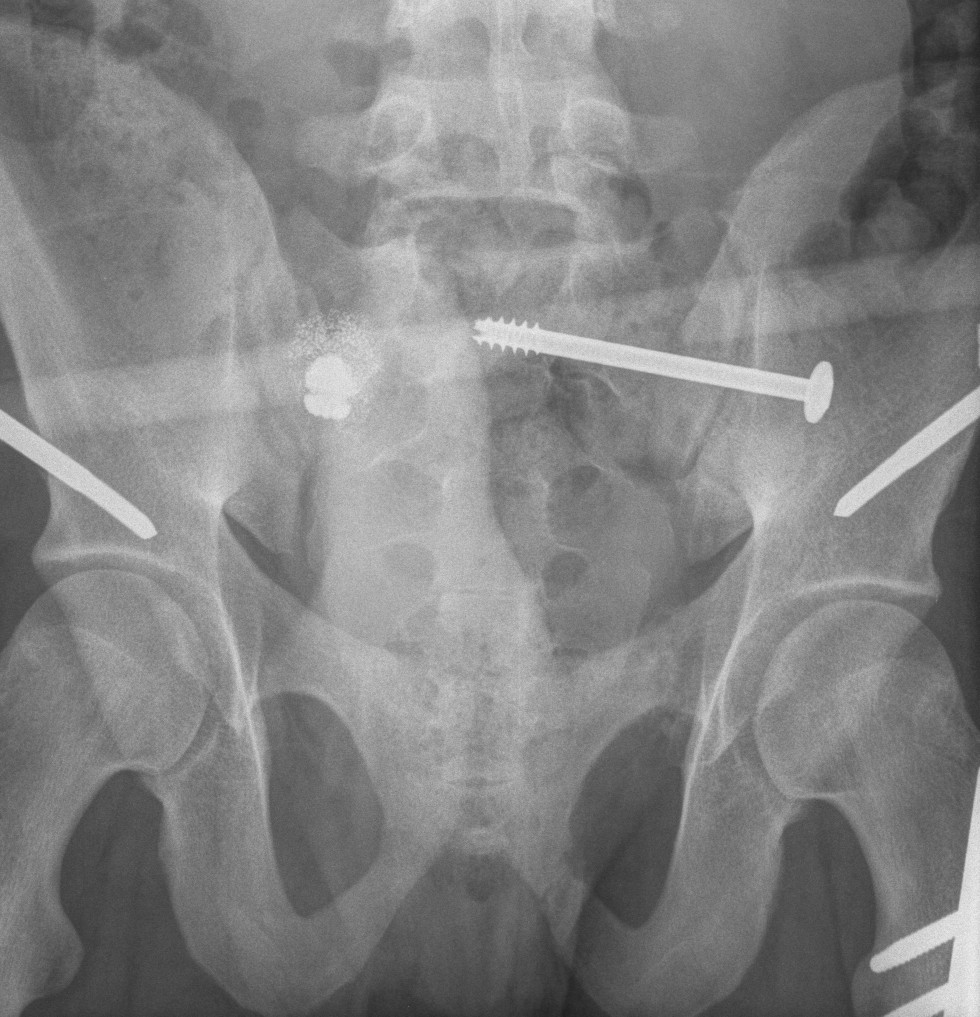
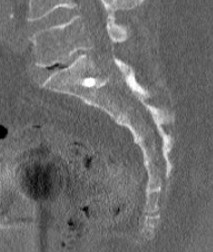
Guide wire insertion into body of S1
- anatomic safe zone
- between S1 foramen and superior ala on outlet view (outlet view)
- between neural canal and anterior body (inlet view)
Insert 6.5 mm partially threaded cannulated screw, to aid compression

Post operative
Check screw position with CT
Protected weight bear for six weeks

Outcomes
Zwingmann et al Arch Orthop Trauma Surg 2013
- systematic review of SI screws inserted using image intensifier versus navigation
- SI screw malposition in 2.6% cases using inlet / outlet views
- SI screw malposition in 0.1% cases using CT navigation

Khaled et al Eur J Trauma Emerg Surg 2015
- 50 patients with one screw, 37 patients with 2 screws
- no difference in outcomes between one or two screws
- systematic review of plates versus SI screws
- no difference in complications or nonunion rates
- implant loosening more common with SI screws
- higher functional outcomes with SI screws
Complications
L5 nerve root
- injured with anterior cortical perforation with screw
- 55 patients with SI screws
- one patient with L5 radiculopathy
- one patient with S1 nerve root injury
Outcomes of APC fractures
Lybrand et al J Orthop Trauma 2017
- 35 APC-2 and 19 APC-3
- trends towards between outcomes with ACP-2
- worse outcomes in patients with higher ISS
- worse outcomes with residual displacement > 15 mm
- APC-2: EQ5D 82, Majeed 77
- APC-3: EQ5D 74, Majeed 81
