Operative
Indications
Pain / discomfort
Difficulty shoe wear
Lesser toe deformity
Skin issues
Contra-indications
Poor peripheral arterial circulation
Diabetes
Aims
1. Correction of the hallux valgus and intermetarsal angles
2. Creation of a congruent MTP joint
3. Sesamoid realignment
4. Removal of the medial eminence
Surgical Options






DTSP (distal soft tissue procedure) - incongruent joint
Metatarsal osteotomy +/- DTSP
- Distal - Chevron
- Midshaft - Scarf
- Proximal - opening / closing wedge, Chevron, crescenteric
Proximal phalanx osteotomy (Akin) (interphalangeus)
TMT fusion / Lapidus
MTPJ fusion
| Congruent | Incongruent |
Mobile TMTJ Metatarsus varus |
OA / Degenerative / Rheumatoid |
|---|---|---|---|
|
DMAA < 15° - treat hallux interphalangeus - Akin with exostectomy |
Mild - Chevron - DSTP +/- MT osteotomy |
Lapidus fusion + DTSP | Arthrodesis |
|
DMAA > 15° - Chevron with closing wedge |
Moderate - DSTP + osteotomy |
||
|
Severe (HVA > 40o, IMA > 20o) - DSTP + osteotomy +/- Akin - DSTP + Lapidus - Arthrodesis |
Peng et al J Orthop Surg Res 2024
- systematic review of Chevron versus Scarf osteotomy
- 6 RCTs and 500 feet
- better correction of HVA with Chevron
- no difference in functional outcomes or complications
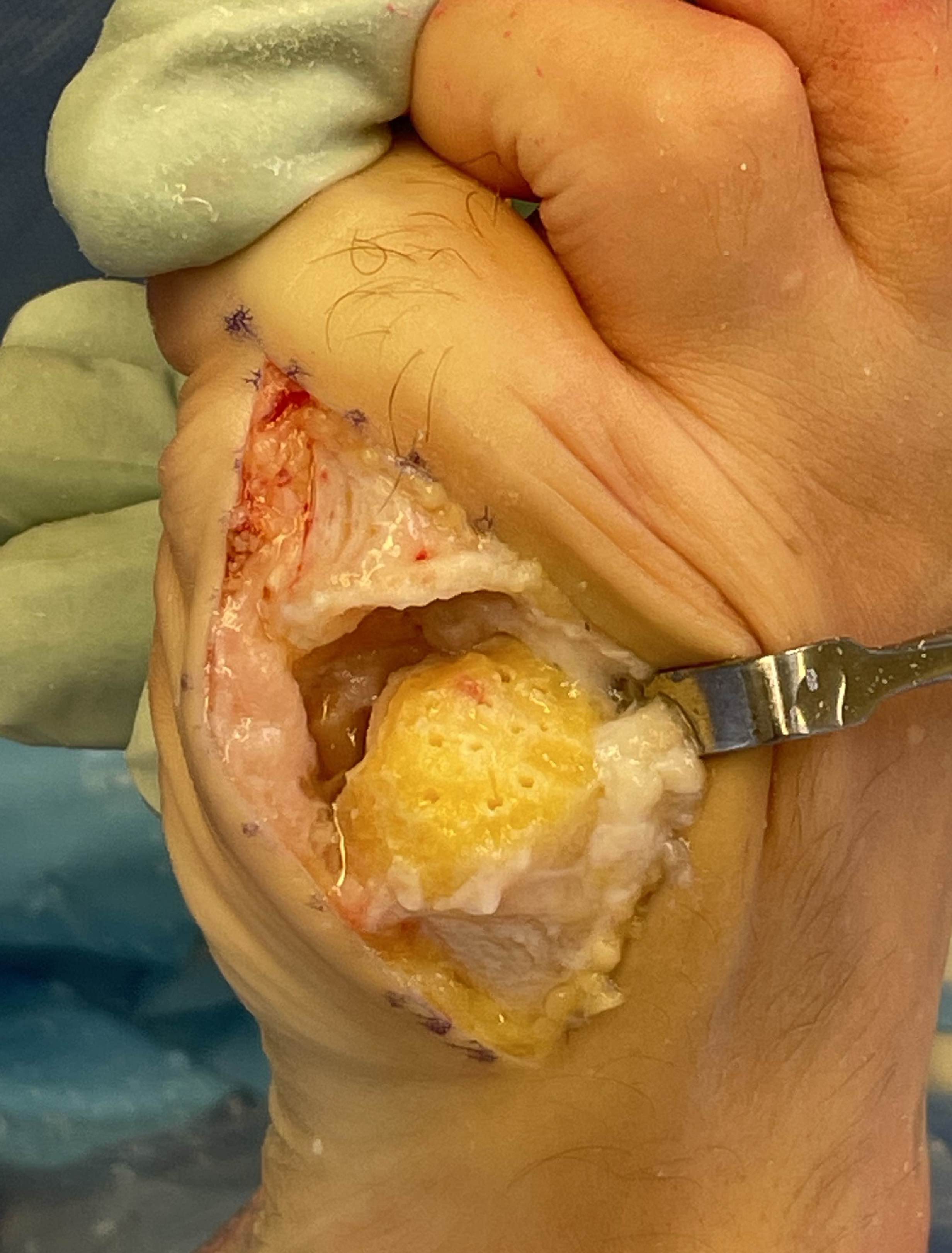
Distal Soft Tissue Procedure / McBride's


Indications
- joint incongruency
Modified McBride concepts
1. MTPJ lateral release
2. Medial exostectomy (just medial to sagittal sulcus)
3. Medial capsular plication / capsulorraphy
Indications
- mild HV with incongruent joint
- moderate / severe HV - combine with osteotomy
Technique
McBride DTSP surgical technique PDF


1. Dorsomedial approach
- protect nerve
- V shaped capsulotomy
- remove medial prominence
2. Incision first web space and lateral release
- protect branches of DPN
- insert lamina spreader
- release abductor tendon from lateral sesamoid
- release intermetatarsal ligament from lateral sesamoid
- release lateral metatarsosesamoid suspensory ligament from lateral sesamoid
- open lateral capsule / LCL
3. Medial capsulorraphy
Chevron osteotomy +/- DSTP


Indications
- incongruent joint
- mild hallux valgus: HVA < 30o / IMA < 15o
Technique

Vumedi Chevron osteotomy video
Dorsomedial approach
- distally based "V" capsular flap
- expose MTP joint
- remove medial eminence with saw
60° osteotomy apex distal
- apex 1 cm from articular surface
- longer plantar limb to avoid sesamoids and inferior joint surface
Translation
- 5 mm medial
- 1mm displacement corrects IM angle 1º
- can perform medial closing wedge to correct DMMA
Fixation
- sutures / k wire / screw
Closure
- imbricate medial capsule
Scarf osteotomy + DSTP


Indications
- moderate hallux valgus
Technique

Dorsomedial approach
- distal soft tissue release
- medial eminence resection
- preserve blood supply at plantar aspect of the metatarsal neck
Longitudinal cut
- oblique: plantar proximal / dorsal distally
- leave strong plantar portion of head to prevent dorsiflexion
Transverse cuts
- plantar proximal / dorsal distal
- angle of 45o with the long cut
Translation
- plantar fragment medially
- can rotate to reduce pronation
Fixation with screws
Proximal Osteotomy + DTSP
Options
- crescentertic
- Chevron
- opening wedge (lengthens)
- closing wedge (shortens)
Arthrex proximal opening wedge video
Arthrex proximal Chevron osteotomy video
Akin osteotomy

Indications
- hallux interphalangeus > 10o
Technique
- medial closing wedge osteotomy of P1


Minimally invasive Hallux Valgus Surgery
Definition
- incisions < 2 cm
- systematic review
- 6 RCT of open versus MIS
- no difference in clinical or radiographic outcomes
Lapidus Procedure / TMT arthrodesis + DTSP




Indications
- moderate to severe HV
- TMTJ hypermobility
- metatarsus primus varus
Technique
Vumedi Lapidus procedure video
Triplanar correction - coronal / sagittal / rotational
Results
Do et al Orthop Clin North Am 2022
- systematic review of 1800 Lapidus
- complication rate 17%
- hardware pain 3%
- nonunion 3%
- delayed union 2%
- wound complication 1%
Arthrodesis


Indications
- hallux valgus with arthritis
- severe hallux valgus
- neuromuscular disease i.e. cerebral palsy
- rheumatoid arthritis
- salvage procedure for failed procedures
Technique
Vumedi surgical technique 1st MTPJ fusion medial approach video
Vumedi surgical technique 1st MTPJ fusion dorsal approach video
Vumedi surgical technique MIS 1st MTPJ fusion video
Approach
- dorsal approach
- medial approach
Position
- 10 - 15° valgus
- 10- 15° dorsiflexion relative to plantar surface / 20 - 25° relative to metatarsal shaft
Fixation
- screws / plate / screws + plate


Complications of Surgery
Complications
Sieloff et al J Foot Ankle Surg 2023
- systematic review of 1500 scarf osteotomies with 2 year followup
- recurrence 5%
- 3.5% troughing
- 1% AVN, 2% infection
- 2% nonunion, 3% malunion, 3% hallux varus
- 5% CRPS
Infection

Hallux Varus
Cause
- excessive medial resection
- resection of lateral sesamoid
- excessive lateral release or medial plication
Issues
- difficulties with shoe wear
Options
- arthrodesis
- soft tissue reconstruction
EHL Reconstruction
- lateral two thirds of the tendon removed from its insertion
- detached distally, passed under transverse ligament
- inserted into proximal phalanx
AVN

Management - arthrodesis
