Aim
Stable, shoe-able plantigrade foot
Multidisciplinary approach
Multidisciplinary foot clinics (MDFC) 1st established UK 1980s
- shown to significantly reduce rate of diabetic amputations
- involve:
Endocrinologist +/- diabetic nurse
- glycaemic control crucial
Podiatrist
- non-surgical debridement
- orthoses
Orthotist / Plaster tech
Vascular surgeon
- referral if absent or asymmetrical pulses
Orthopaedic surgeon
- TCC
- foot reconstruction; amputations
Infectious Disease Consultant
- infected / nonhealing ulcers
Diabetic Foot Care
Foot Hygiene
- daily wash with mild soap & warm water
- powder between toes & moisturiser to ankle
- plain cotton socks inside out (2 socks ↓shear)
- minimum tds inspection
- report immediately all blisters / ulcers & unilateral warmth / swelling (Charcot’s fractures)
- no walking barefoot
Shoes / Orthoses
- custom made orthoses and shoes reduce DFU recurrence 1
- shoes should be
wide/ deep/ round toe box
soft leather (hard materials irritate)
adjustable
no/low heel
Issues
Infections
Ulcers
Charcot
Fractures
1. Diabetic Foot Infections
(Therapeutic Guidelines; Version 15; 2015)
A. Mild Cellulitis (+/- Ulcer)
Combination oral Abx
- Augmentin Duo Forte
OR Cephalexin PLUS Metronidazole
OR Ciprofloxacin PLUS Clindamycin (Penicillin Allergy)
- offload ulcer (crutches, custom orthotics )
B. Severe Cellulitis (+/- Ulcer)
IV Abs (Timentin or Pip-Taz; IV Cipro + Clind for Penicillin Allergy)
- Offload Ulcer
C. Ulcer with Osteomyelitis
Diagnosis
- probe-to-bone test (Positive predictive value .57; Negative Predictive Value .98) 2
- plain films (low sensitivity; particularly early stage)
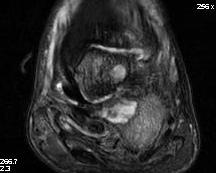
- MRI (high sensitivity and specificity; with plain films Ix of choice)
- Tc Bone Scan + Labelled WCC (if MRI contraindicated)
Management OM
- consider debridement & intra-operative deep MCS (more accurate)
Antibiotics
- broad spectrum initially / timentin or pip-taz
- adjust 2° to MCS
- ID consult
Diabetic Calcaneal Abscess


2. Neuropathic Ulcers

Classification
1)Wagner Classification3
Most used classification for DFU in ortho literature
Grade 0
Pressure area
- Footwear Modification
Grade I
Superficial Ulceration
- local treatment, footwear modification
Grade II
Deep Ulceration (probes to tendon / capsule)
- TCC, footwear modification
Grade III
Deep ulceration + secondary infection
- debridement, antibiotics
Grade IV
Partial foot gangrene
- Abx, amputation, hyperbaric O2
Stage V
Whole foot Gangrene
- regional amputation, Abx
2) University of Texas4
Each wound has a grade and stage
- increasing stage, across all grades, more predictive of amputation & prolonged healing time
- UT better prognosticator than Wagner
Grade 1 Preulcerative
Grade 2 Superficial Wound
Grade 3 Deep wound penetrating to capsule or tendon
Grade 4 Deep penetrating to bone or joint
Stages A Clean
Stages B Nonischaemic Infected
Stages C Ischaemic Noninfected
Stages D Ischaemic Infected
Management
Nonoperative
1) Off-load
TCC remains the gold standard
- other options: removable cast walkers; modified footwear
2) Increase healing rates
Hyperbaric O2 - short-term reduction ulcer size
Negative Pressure Wound Therapy (NPWT)
Biologic Therapy eg amniotic membrane (experimental)
Operative
1) Tendoachilles lengthening (TAL)
Aim to reduce forefoot pressures
Colen et al Plast Reconstr Surg 2013
- level 3 retrospective cohort
- 25% of patients with DFU & no TAL Vs 2% of DFU with TAL had recurrent ulcer
2) Gastrocnemius Recession
3) Toe Flexor Tenotomy
3. Charcot Foot
See Charcot Foot
4. Fractures in Neuropathic / Diabetic Feet
Principles
1. Augment ankle ORIF
2. Double time for sutures
3. Double immobilisation period
- 12 weeks NWB
- 4-5 months in walking cast
4. Brace for 1 year after surgery
- to prevent late Charcot arthropathy
- assume Charcot joint will develop
References
1- http://www.ncbi.nlm.nih.gov/pubmed/22336901
2- http://www.ncbi.nlm.nih.gov/pubmed/17259493
