Definition
Injury to anterior and middle columns, with retropulsion +/- posterior column
Mechanism
Vertical compression
Epidemiology
10% cervical fractures
Most commonly C5/6
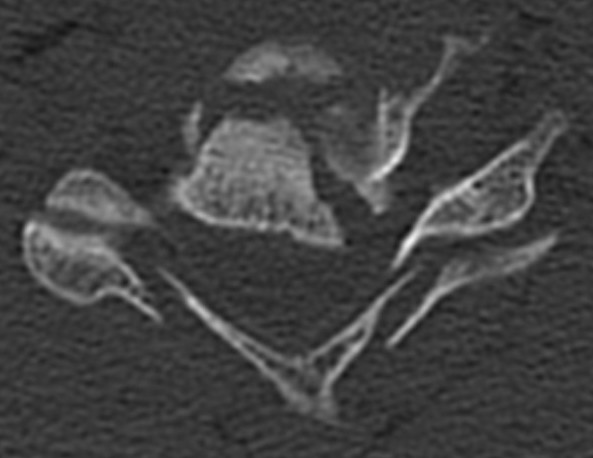
Pathology
Anterior & middle columns fail
- if severe, posterior ligament complex fails
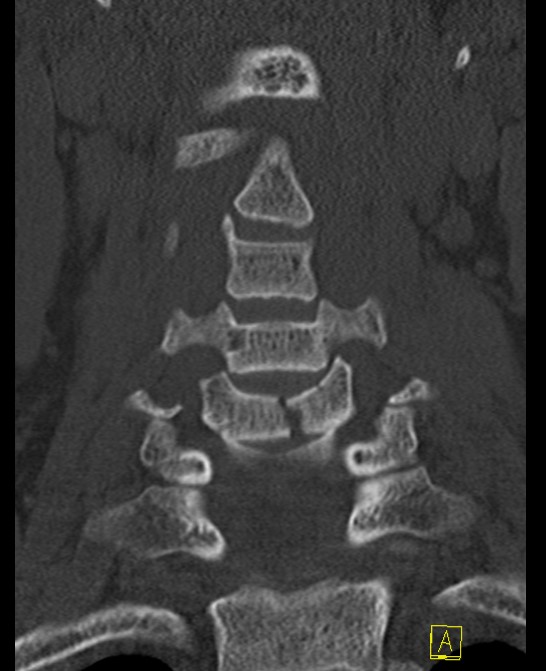
Canal compromise / neurological injury
- retropulsed fragments
- typically one or two main retropulsed fragments
Neurology
More common than in upper cervical spine injuries
Clinical
Neck pain
Complete / incomplete cord lesion
American Spinal Injury Association (ASIA) Classification
- A (complete): no motor or sensory
- B (incomplete): no motor, some sensory intact
- C (incomplete): > 50% muscle groups strength < grade 3
- D (incomplete): > 50% muscle groups strength > grade 3
- E (normal) motor and sensory
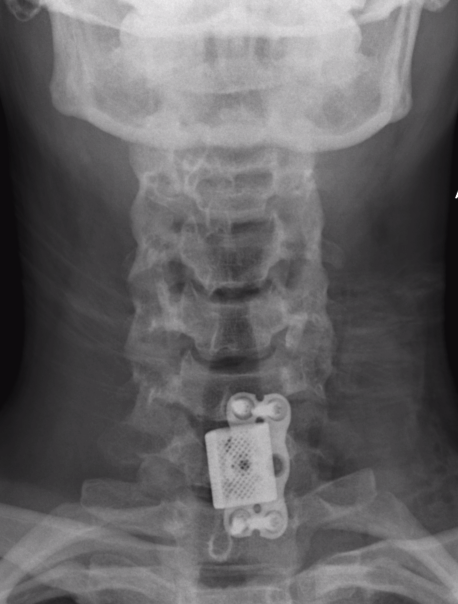
X-ray
AP
- widening between pedicles is hallmark on AP
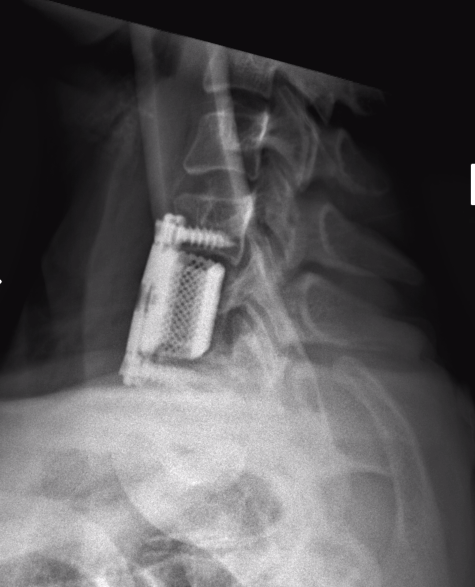
Lateral
- > 50% anterior column loss of height
- loss of posterior vertebral height
CT

MRI
Assess integrity of posterior column
Evaluate cord injury


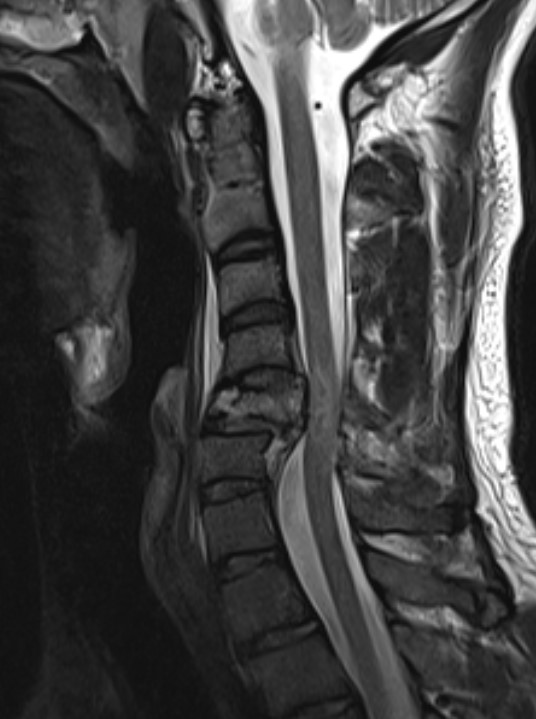

MRI images demonstrating spinal cord injury and posterior ligamentous injury
Subaxial Injury Classification System / SLIC
| Injury Morphology | Discoligamentous complex | Neurological status | |||
| No abnormality | 0 | Intact | 0 | Intact | 0 |
| Compression | 1 | Indeterminate (MRI change only) | 1 | Root injury | 1 |
| Burst | 2 | Disrupted | 2 | Complete cord injury | 2 |
| Distraction / facet perch | 3 | Incomplete cord injury | 3 | ||
| Rotation / facet dislocation | 4 | Persistent cord compression | +1 |
SLIC 1 - 3 - neurologically intact, non operative
SLIC 4 - equivocal
SLIC > 5 - surgery
Reliability
Spitnale CORR 2020 - variable inter- and intra-observer reliability in the literature
AOSpine subaxial cervical spine injury classification
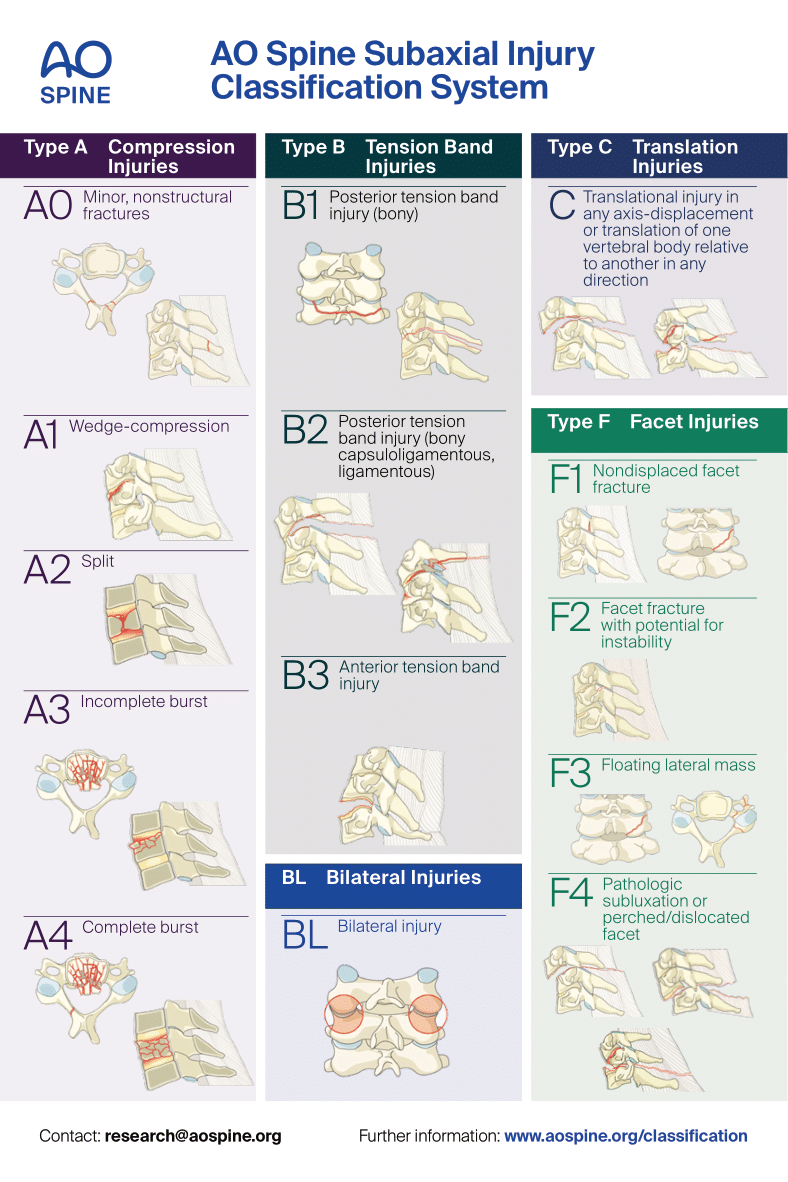
Neurological status:
N0 - neurologically intact
N1 - transient neurological deficit
N2 - radicular symptoms
N3 - incomplete spinal cord injuries
N4 - complete spinal cord injuries
NX - cannot be examined
Specific modifiers:
M1 - incomplete disruption of the posterior ligamentous complex
M2 - critical disk herniation
M3 - presence of comorbid spine conditions (osteoporosis, DISH, ossification of the PLL, AS)
M4 - vertebral artery injury
Reliability
Feuchtbaum et al Curr Rev Musculoskeletal Med 2016 - variable inter- and intra-observer reliability in the literature
Non operative Management
Indications
Wedge fractures
- < 50% height loss
- caused by flexion compression
- injury to anterior column only
Posterior column intact / nil instability / SLIC score 1 - 3
Minimal kyphosis
Nil neurology
Treatment
Collar for 6 weeks
Operative Management
Indications
Instability
Neurology
SLIC >5
Timing
- early (<24 hours) versus delayed (>24 hours) surgery
- 313 patients with acute cervical spinal cord injury
- improved neurological outcomes with decompression < 24 hours
- surgical decompression < 8 hours versus 8-24 hours
- 42 patients with acute cervical spinal cord injury
- improvement of 2 ASIA grades in 46% patients treated < 8 hours
- improvement of 2 ASIA grades in 10% patients treated 8-24 hours
Steroids
Fehlings et al Global Spine J 2017
- evidence of modest improvements in motor functions with methylprednisone infusions within 8 hours
Technique
A. Anterior corpectomy & fusion with tricortical graft + plate
B. Anterior corpectomy & fusion with mesh cage + bone graft + plate
+/- Supplemental posterior fixation / cervical lateral mass screws


Anterior corpectomy and tricortical graft
AO Surgery reference anterior cervical corpectomy
Vumedi anterior cervical corpectomy